Definition/Description
Osteoarthritis of the cervical spine may be defined as a degenerative disorder of C1-C7, complicated by inflammatory reactions. It is a very complex disease with multiple causes[1] which affects the intervertebral discs, vertebral bodies, intervertebral ligaments, the hyaline cartilage, the underlying bone, joint capsule and zygoapophyseal joints. It can lead to the formation of osteophytes or subchondral cysts and can cause hypertrophy of the articular process.[2] Cervical osteoarthritis can also be referred to as cervical spondylosis.
Clinically Relevant Anatomy
There is a ‘three joint complex’ at every spinal level except C1–C2. This motion segment is formed by the three articulations between adjacent vertebrae. These three articulations consist of one disc and two facet joints. The superior articular processes of the lower vertebra are positioned upwards and will articulate with the smaller inferior articular processes of the vertebra above it. The cervical facet articular surface area is about two-thirds the size of the area of the vertebral endplate. The facet joint has features typical of a synovial joint: articular cartilage covers the opposed surfaces of each of the facets, resting on a thickened layer of subchondral bone, and a synovial membrane covers this portion of the joint. A superior and inferior capsular pouch, filled with fat, is formed at the poles of the joint, and a baggy fibrous joint capsule covers the joint like a hood. A fibro-adipose meniscus projects into the superior and inferior aspect of the joint and consists of a fold of synovium that encloses fat, collagen, and blood vessels. The menisci serve to increase the contact surface area when the facets are brought into contact with one another during motion, and slide during flexion of the joint to cover articular surfaces exposed by this movement.[2]
The cervical spine components that are affected by osteoarthritis are;
- Articular cartilage. [1] Initially fibrillation and shallow pitting occur, which affects the surface of the cartilage focally at first. At a more progressed stage, this can evolve to deeper fibrillation and fissuring, peeling off and pitting until the subchondral bone is affected. [2]
- Synovium[1]
- Uncovertebral joints. Osteophytes are formed on the articular surfaces of the uncinate process. These osteophytes can impinge anatomical structures like the cervical spinal cord, spinal nerve root, radicular artery, vertebral artery and cervical sympathetic trunk.
- Facet joints. They are inclined 45° from the horizontal. The joint surfaces are generally planar, but not flat.[2]
- Intervertebral discs. Between C0–C1 and C1-C2 there is no intervertebral discs. Major factors in the development and progression of osteoarthritis of the facet joints are joint alignment and load distribution.[2]
- Cervical plexus. Osteophyte formation or progressive cartilage thinning may narrow the intervertebral foramen through which the cervical nerve roots emerge.[2] [3]
- Intervertebral ligaments.
Epidemiology/Etiology
Cervical osteoarthritis may be generalised, sometimes involving the entire cervical region, but it is usually more localised between the 5th and 6th and the 6th and 7th cervical vertebrae.
Anyone can develop cervical osteoarthritis, but it is rare in people younger than 40-50 years, the incidence increasing with age, women having a higher risk for cervical OA than men.[4] It is common in people above the age of 50 and especially if those people who have had jobs that included remaining in a single static position for long periods, i.e. reading, writing and other desk-based careers.[5]
Cervical OA can have many causes such as mechanically over-stressing of a joint (e.g. working with tools which generate intense vibration), previous bone fractures or other injuries to the neck, overload at a young age, postural asymmetry or asymmetric loading of a joint.
Facet joint osteoarthritis (FJOA) is intimately linked to the distinct but functionally related condition of degenerative disc disease, which affects structures in the anterior aspect of the vertebral column. FJOA and degenerative disc disease are both thought to be common causes of back and neck pain, which in turn have an enormous impact on the health-care systems and economies.[2]
Characteristics/Clinical Presentation
OA is characterised by pain, stiffness, crepitus, limited range of movement and sometimes joint instability and mild synovitis. The pain is usually localised around the affected joint, but referred pain may occur. Pain associated with FJOA can arise from nociceptors within and surrounding the joints, including nociceptors in the bone itself, as the facet joints and their capsules are well innervated. Pain can radiate to the occiput, the medial border of the scapula and the upper limbs. Pain often becomes worse with joint movement and can be more severe at the end of the day. Morning stiffness can be a common feature but usually dissipates with movement. Restricted movement can occur due to pain, capsular thickening and the presence of osteophytes.[6]
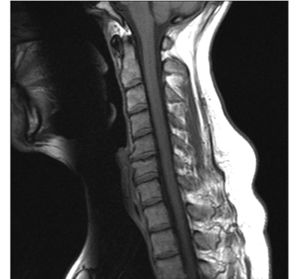
Osteophytes can form around the intervertebral joints and cause neurological symptoms due to compression of the spinal nerves (Cervical Radiculopathy). Narrowing of the spinal canal (Cervical Stenosis) can also cause compression on the spinal cord and circulation problems from compression of vascular structures. Performing an MRI can be useful to confirm the presence of any spinal cord compression (Cervical Myelopathy).
Awareness of potential red flags is essential, which may indicate a more serious issue:[7]
- Malignancy, infection, or inflammation
- Fever, night sweats
- Unexpected weight loss
- History of inflammatory arthritis, infection, tuberculosis, HIV infection, drug dependency, or immunosuppression
- Excruciating pain
- Intractable night pain
- Cervical lymphadenopathy
- Exquisite tenderness over a vertebral body
- Gait disturbance or clumsy hands, or both
- Objective neurological deficit
- Sudden onset in a young patient suggests disc prolapse
- History of severe osteoporosis
- Drop attacks, especially when moving the neck, suggest vascular disease
- Intractable or increasing pain
Prolonged peripheral inflammation in and around facet joints can lead to central sensitisation, neuronal plasticity, and the development of chronic spinal pain.
Differential Diagnosis
There are other conditions to consider before making a diagnosis:[7]
- Other non-specific neck pain lesions: acute neck strain, postural neck ache, or whiplash
- Fibromyalgia and psychogenic neck pain
- Mechanical lesions: disc prolapse
- Diffuse idiopathic skeletal hyperostosis
- Inflammatory disease: rheumatoid arthritis, ankylosing spondylitis, polymyalgia rheumatica, psoriatric arthritis, septic arthritis, reactive arthritis
- Metabolic diseases: Paget’s disease, osteoporosis, gout, or pseudo-gout
- Osteomyelitis or tuberculosis
- Malignancy: primary tumous, secondary deposits, or myeloma
Diagnostic Procedures
A diagnosis is usually based on the clinical presentation.[8]
- Pain on range of motion
- Limitation of range of motion
- Lower extremity sensory loss, reflex loss, motor weakness caused by nerve root impingement
- Pseudoclaudication caused by [8]Kellgren and Lawrence developed a grading system for the radiological appearance of a joint with osteoarthritis.[9] If more than one joint in a group is assessed, then the most severe grade is reported:
Radiological appearance of osteoarthritis Grade Parameters normal (no signs of osteoarthritis) 0 doubtful change (uncertain) 1 osteophytes at the joint margins and periarticular ossicles definite, minimal to mild 2 narrowing of the joint space definite, moderate 3 cystic areas with sclerotic walls in subchondral bone definite, severe 4 deformity of bone (altered shape) Outcome Measures
Functional status and disability measure (evaluation of the activities of daily living) can be assessed by the Neck Pain and Disability Scale (NPAD) and the Neck disability index (NDI).[10]
- The Neck pain and disability scale (NPAD) is a composite index including 20 items, which measure the intensity of neck pain, its interference with vocational, recreational, social, and functional aspects of living and also the presence and extent of associated emotional factors.
- The Neck disability index (NDI) is a patient completed and condition-specific functional status questionnaire. This questionnaire consists of 10 items, including pain, personal care, lifting, reading, headaches, concentration, work, driving, sleeping and recreation. This questionnaire has been designed to give information as to how neck pain has affected the patient’s ability to manage in daily life.
The NPAD and NDI are both seen as valid measures of self-reported neck pain related disabilities.
Examination
As osteoarthritis is primarily a clinical diagnosis, patient history and the physical examination is usually sufficient to make a confident diagnosis. Joint pain and limited range of motion are usual symptoms in patients with cervical osteoarthritis. The pain tends to worsen with activity, especially following a period of rest (gelling phenomenon). [11]
Physical examination follows a normal cervical examination and includes:[2]
- Inspection: posture, oedema, erythema, evidence of trauma, muscle atrophy, skin abnormalities and joint deformity.
- Palpation of facet joints, examining of anatomic abnormality, temperature and tenderness.
- Range of motion of the cervical region and shoulder region.
- Stress of the facet joints: pain increases with hyperextension, extension-rotation of the neck. Pain decreases while doing flexion of the neck.
- Neurological evaluation: motor and sensory evaluation of sensation, reflexes and muscle strength. Other special tests may be indicated: L’hermitte sign, Hoffman’s test, Babinski.
- Muscle testing: searching for myofascial trigger points in the sternocleidomastoid, cervical paraspinal muscles, levator scapulae, the upper trapezius and suboccipital musculature.
Medical Management
The following medical management strategies are only indicated when all other conservative treatment has failed.
Intra-articular Injections
Intra-articular corticosteroids are recommended for hip and knee osteoarthritis. The effects of corticosteroids on cervical osteoarthritis need to be researched.[11]
Surgical Treatment
There are indications that excision and fusion of the anterior cervical intervertebral disc (Cloward operation) together with the removal of associated arthritic bone spurs pressing on the nerves and spinal cord can give relief of pain and muscle weakness in patients who have cervical osteoarthritis with neurologic pain.[11]
Pharmacology
In the short-term, some benefit may be gained from using chondroitin (alone or in combination with glucosamine). Other options can be acetaminophen, NSAIDS or opoids.[11]
Physical Therapy Management
The main goals of management for cervical OA are:
- reducing pain and stiffness
- improving joint mobility
- inhibiting any further progression of joint damage
Advice and Education
Providing information related to the disorder, stress management and postural advice in daily activities, work and hobbies should also be part of any treatment plan.[7] Providing encouragement and motivation where necessary is also a key component.[12]
Advice and education regarding good neck posture is a key part of treatment as the condition progresses, as neck posture can negatively affect any patient. Sleeping advice is that side lying is the preferred position and a single pillow only under the head is recommended, although a butterfly pillow offers the best support, as it is flattened in the middle and the elevated sides support the head.
Exercise Therapy
Treatment for cervical osteoarthritis is usually conservative and it can be treated using a variety of therapy possibilities with exercise therapy being a key element. Exercise includes mobilisation exercises, strengthening of local muscles around the affected joint and improving overall aerobic fitness[7][12] There is considerable evidence that suggests physical activity can help in the management of chronic pain and should play a key role in the overall treatment plan. This will improve the disability over time and has other multiple health benefits.
Manual Therapy
Manual therapy such as massage, mobilisation, and manipulation may provide further relief for patients with cervical osteoarthritis[12]. Mobilisation is characterised by the application of gentle pressure within or at the limits of normal motion to improve ROM.
Manipulation may be considered, but there are numerous contraindications, such as myelopathy, severe degenerative changes, fracture or dislocation, infection, malignancy, ligamentous instability and vertebrobasilar insufficiency which have to be taken into consideration.
Heat and cold modalities
It is recommended that when application of superficial heat or cold is considered in the management of OA that patients experiment to identify the intervention that offers them the greatest relief.[13]
Hydrotherapy
It has been shown that hydrotherapy can give some relief to patients struggling with pain and OA. However, the research is poor and points to mostly short term effects.[12]
Acupuncture
The use of acupuncture is associated with significant reductions in pain intensity, improvement in functional mobility and quality of life. Evidence supports the use of acupuncture as an alternative for traditional analgesics in patients with osteoarthritis.[14]
Electrotherapy
Ultrasound
Ultrasound may be beneficial, but there is only low quality evidence for its effectiveness on osteoarthritis. Most studies, however, have investigated its effectiveness on hip and knee osteoarthritis. The magnitude of the effects on pain relief and function is still unclear and any positive results may wholly be due to placebo.[15]
TENS
TENS can also provide symptomatic relief.[16]
References
- ↑ 1.01.11.2 Musumeci G, Aiello F, Szychlinska M, Di Rosa M, Castrogiovanni P, Mobasheri A. ↑ 2.02.12.22.32.42.52.62.7 Gellhorn AC, Katz JN, Suri P. ↑ Rand RW, Crandall PH. ↑ Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. ↑ Plotnikoff R, Karunamuni N, Lytvyak E, Penfold C, Schopflocher D, Imayama I, Johnson ST, Raine K. ↑ Hunter DJ, McDougall JJ, Keefe FJ. ↑ 7.07.17.27.3 Binder AI. ↑ 8.08.1 Zhang Y, Jordan JM. ↑ Kohn MD, Sassoon AA, Fernando ND. Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clinical Orthopaedics and Related Research. 2016. 474: 1886. Available from: ↑ MacDermid JC, Walton DM, Avery S, Blanchard A, Etruw E, Mcalpine C, Goldsmith CH. Measurement properties of the neck disability index: a systematic review. Journal of orthopaedic & sports physical therapy. 2009 May;39(5):400-17. Available from: https://www.jospt.org/doi/pdfplus/10.2519/jospt.2009.2930 [Accessed 19 June 2019]
- ↑ 11.011.111.211.3 Sinusas K. ↑ 12.012.112.212.3 Cibulka MT, White DM, Woehrle J, Harris-Hayes M, Enseki K, Fagerson TL, Slover J, Godges JJ. Hip pain and mobility deficits—hip osteoarthritis: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Association. Journal of Orthopaedic & Sports Physical Therapy. 2009 Apr;39(4):A1-25. Available from: https://www.jospt.org/doi/pdfplus/10.2519/jospt.2009.0301 [Accessed: 18 June 2019]
- ↑ Denegar CR, Dougherty DR, Friedman JE, Schimizzi ME, Clark JE, Comstock BA, Kraemer WJ. ↑ Manyanga T, Froese M, Zarychanski R, Abou-Setta A, Friesen C, Tennenhouse M, Shay BL. ↑ Loyola-Sánchez A, Richardson J, MacIntyre NJ. ↑ Osiri M, Welch V, Brosseau L, Shea B, McGowan JL, Tugwell P, Wells GA. function gtElInit() { var lib = new google.translate.TranslateService(); lib.setCheckVisibility(false); lib.translatePage('en', 'pt', function (progress, done, error) { if (progress == 100 || done || error) { document.getElementById("gt-dt-spinner").style.display = "none"; } }); }