Definition/Description
Congenital deformities of the spine are deformities identified at birth that are the result of anomalous vertebral development in the embryo. Minor bony malformations of all types occur in up to 12% of the general population and are usually not apparent. [1] The spine is a complex and vital structure. Anatomically, a variety of tissue types are represented in the spine, including musculoskeletal and neural elements. Several embryologic steps must occur to result in the proper formation of both the musculoskeletal and neural elements of the spine. Alterations in these embryologic steps can result in congenital abnormalities of the spine. [2] Based on the type of malformation, the resulting deformity and the specific region of the spine where the malformation occurs, these congenital malformations of the spine can be classified into three main groups:[2]
- When the neural tube fails to completely close during the embryonic development, this is a neural tube defect. The most common example is spina bifida. This term refers to a defective fusion of the posterior spinal bony elements, but is still incorrectly used to refer to spinal dysraphism in general, [3] Spina bifida aperta is an open spinal dysraphism for example, associated with meningocele or meningomyelocele and Spina Bifida Occulta is an example of closed spinal dysraphisms. [4]
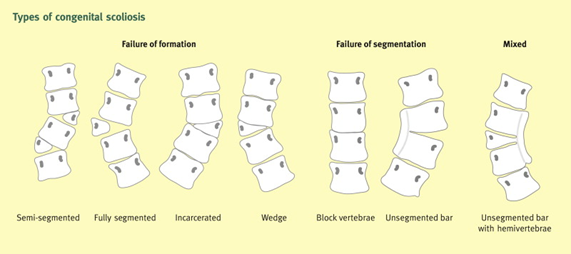
- When two or more vertebrae fail to fully separate and divide with concomitant partial or complete loss of a growth plate, this is called a failure of segmentation. Examples of this type of congenital spine deformity are congenital scoliosis, congenital kyphosis, congenital lordosis and Klippel-Feil syndrome. [5]
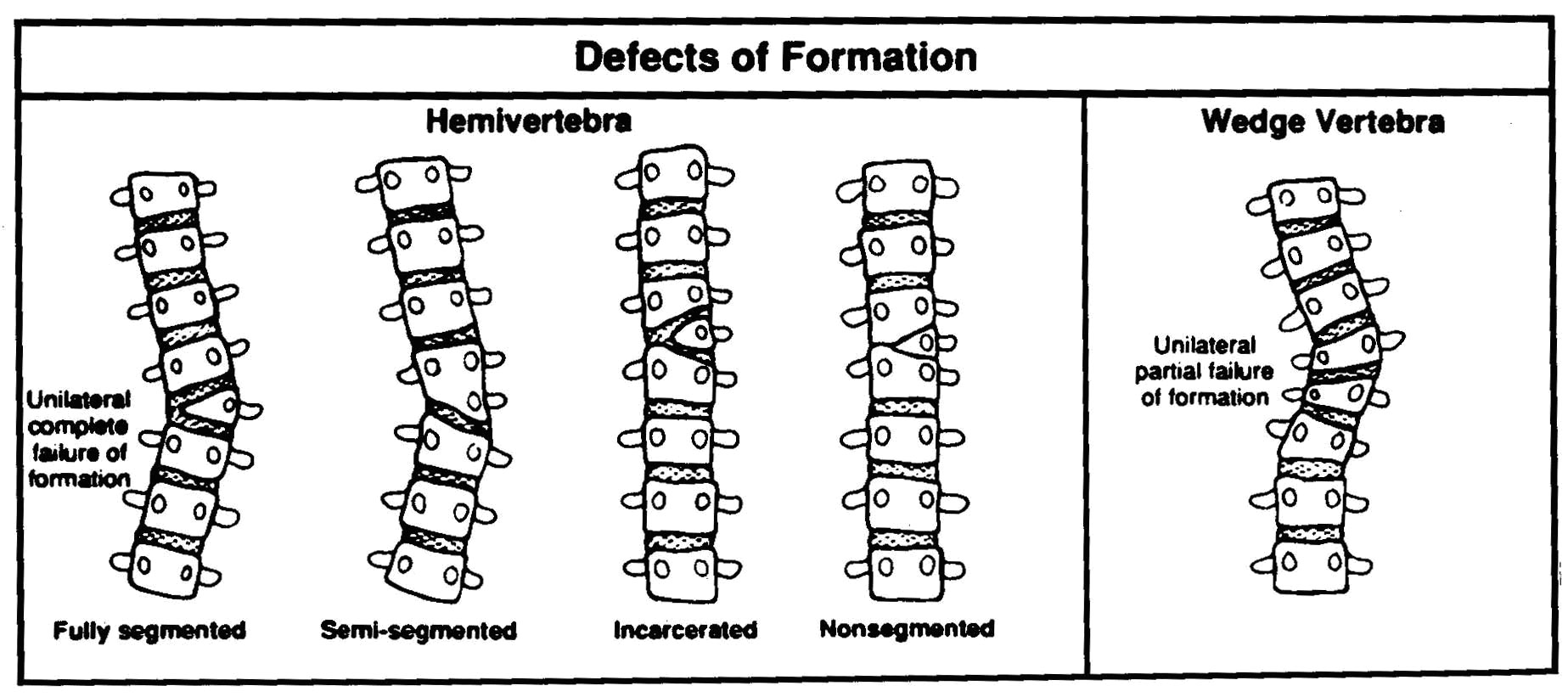
- Congenital scoliosis and congenital kyphosis, and congenital lordosis can also be examples of a failure of formation. This type of congenital spine deformity occurs as a result of an absence of a structural element of a vertebra. Typical observable defects are hemivertebrae or wedge vertebrae. [5][6]
Congenital abnormalities of the spine have a range of clinical presentations. Some congenital abnormalities may be benign, causing no spinal deformity and may remain undetected throughout a lifetime. Others may be associated with severe, progressive spinal deformity leading to cor pulmonale or even paraplegia. Some deformities will result in sagittal plane abnormalities, for example kyphosis or lordosis, whereas others will primarily affect the coronal plane, like scoliosis. The resultant spinal deformity is often a complex, three-dimensional structure with differences in both the coronal and sagittal plane, along with a rotational component along the axis of the spine.[7]
Clinically Relevant Anatomy
Neural tube deformities
Neural tube deformity is a term for congenital anomalies because of incomplete closure of the neural tube in the utero. [8][9] This causes impaired formation of structures along the craniospinal axis. [10] Spinal neural tube defects can be subdivided into those that are open versus those that are closed:
- Open: the failure is primary neuralation
- Closed: the structural deformities are mostly limited to the spinal cord. [11][12]
It is not only the elements of the spine that can be affected. Other bodily organs which formed during the same embryonic stage can also be affected. This is because the paraxial mesoderm is responsible for the formation of the vertebrae, whereas the other two areas of mesoderm (intermediate and lateral) are involved in the development of the urogenital, pulmonary and cardiac systems. Many patients may have difficulty with respiration due to the abnormal curvatures of the spine [5]. It has also been observed that these associated anomalies have an influence on the progression of untreated congenital Scoliosis.[13]
Failure of segmentation/ formation
The bony structure of the spine is determined in the first 6 weeks of intrauterine life, at the mesenchymal stage of embryonic development. Somites form and undergo a process of segmentation and recombination. This is necessary to give rise to the cartilaginous mould that afterwards will ossify to form the bony spine. Errors during this process can lead to either failure of formation, failure of segmentation or a combination of both. [14]
Examples of a failure of segmentation are:
Examples of a failure of formation are:
The anomaly is present at birth, so a curvature is noted much earlier than patients with idiopathic scoliosis. Large deformities can result due to the number of years of growth remaining. [16]
Epidemiology /Etiology
The etiology of congenital spine deformities varies greatly because there are many different types. It is difficult to identify one factor that may be responsible with prevalence being different for each of them. [5] They can be divided into 3 groups:
- Neural tube deformities such as spina bifida which is not a very common disease. It is believed that spina bifida is caused during pregnancy due to a deficiency of vitamin B and is also dependant on genetic and environmental factors. Obese women with poorly controlled diabetes have a greater risk of having children with spina bifida. In America less than 1 in 1000 children are born with it each year. Having a child with spina bifida increases the chance that further children will also develop the condition by 8 times [17][18]
- Congenital spine deformities due to failure of segmentation. In this case, the vertebrae are fused together and cause congenital kyphosis, congenital lordosis, and Scoliosis. [19] Congenital Scoliosis is not the most common type as it only accounts for 15% of the total cases [20] with thoracic scoliosis being the most common at 64% of the total cases, Thoracicolumabar scoliosis accounts for 20% with 11% located in the lumbar region and 5% in the lumbosacral region. [5]Klippel-Feil syndrome is also due to a failure of segmentation. There is not much known about the prevalence of this syndrome.
- Congenital spine deformities due to failure of formation are rare. The prevalence of hemivertebrae is 0.33 out of 1000 births and there is an equal number of women and men affected. Goldstein showed that 23 out of the 26 children with hemivertebrae developed a congenital spine deformity like scoliosis, congenital lordosis or congenital kyfosis. [21]
Environmental factors, genetic factors, vitamin deficiency, chemicals, and drugs, singly or in combination, have all been implicated in the development of congenital abnormalities during the embryonic period. Whatever the factor is that influences the embyo it must affect the embryo at a very early stage of development, before cartilage bone can develop. These defects can lead to a failure of segmentation or a failure of formation of the spine. [22]
Studies carried out confirmed various possible causes that may help in the prevention of these anomalies. showing that during critical stages of development, fetal exposure to thalidomide can lead to severe congenital malformations. Ghidini et al. suggested that mothers taking lovastatin have an increased risk for congenital abnormalities. Certain progestin/estrogen compounds may also increase the incidence of these anomalies. [5]
Characteristics/Clinical Presentation
A defect early in fetal life may have a variety of clinical presentations as several systems develop from a common precursor.[5] Examples of these clinical presentations are scoliosis, hyperlordosis and/or hyperkyphosis. Congenital abnormalities of the spine also have the potential to affect the spinal cord and associated nerve roots. The neurological symptoms can vary from minor motor or sensory signs to paraplegia, depending on the type and severity of the congenital spine deformity, but congenital spine deformities are not always immediately obvious at birth. [23] They can present as a deformity with growth or with clinical signs of neurologic dysfunction during adolescence or adulthood.
Neural tube deformities
As described earlier, neural tube deformities can be divided into two groups:
- Open: neural elements and/or membranes are exposed to the external environment.
Myelomeningocele is characterised by being most frequently present in the lumbosacral region, [24] a bulging of a sac like structure covered by a thin membrane with CSF that will drain if the sac is disrupted [25]
Myelocele Is associated with similar clinical implications as myelomeningocele but is flat [25]
Hemimyelomeningocele is a rare lesion where the spinal cord has been divided by a bony spur with one segment open and the other closed [12]
- Closed: spinal abnormalities covered by skin. Some go undetected or remain asymptomatic, [12][26] but there are variants that can be associated with cord tethering, subcutaneous mass or more severe spine abnormalities. The lumbosacral region is the most common location of these defects [10] An affected child has an intellectual function and other functions are as well less affected [11] Lipomyelomeningocele and lipomyelocele are characterised by subcutaneous fatty mass above the gluteal crease [25]
Failure of segmentation
Congenital scoliosis is charaterised by:
- a three-dimensional deformity involving lateral curvature and rotation
- a benign prognosis
- the fact that worst curves occur with unilateral defects
- a curve site dependent on the location of apical vertebra [27]
Congenital kyphosis
- Can progress rapidly and may cause spinal cord compression and paralysis [28]
Failure of formation
Congenital scoliosis
Congenital kyphosis
Differential Diagnosis
Most congenital spine deformities are diagnosed in the uterus, and if not, at birth. as they are clearly present e.g. Spina Bifida, scoliosis. Some disorders, however, might not become symptomatic until childhood or even adulthood [4] In these cases, MRI scans or ultrasound can be used to diagnose the specific disorder, [30] therefore, for many conditions there is not a differential diagnosis as the deformity/anomaly will be clear on an MRI.
Neural tube deformities
Spina bifida is an out dated term for spinal dysraphism. [31] This modern term includes many congenital anomalies where the neural tube is defective, which leads to hernia’s of the meninges or other neural tissues.
- open: with a non-skin covered back mass, where you have to differentiate between myeolecele and myelomeningocele
- closed: with a skin-covered back mass, where you have to determine whether there is a subcutanuous mass present or not [32]
Failure of segmentation
Congenital scoliosis:
In most of the severe cases, scoliosis can be detected without medical imaging. There are different forms that can be present as a result of failure of segmentation:
- A block vertebra, which is a bilateral failure with complete fusion of the disc between the involved vertebrae.
- A unilateral unsegmented bar has fused discs and facet joints on one side of the vertebral column. [3]
Congenital kyphosis:
- idiopathic hyperkyphosis
- neuromuscular
- spinal cord tumor
- connective tissue disorders
- skeletal dysplasia
- infection (tuberculosis, pyogenic, fungal)
- tumor
- myelomeningocele[3]
Congenital spinal canal stenosis
The sagittal diameter must be
- Cervical: MS, Myelitis, B12 hypovitaminosis, spinal tumors, polyneuropathy (PNP), ateriovenous malformations
- Thoracal: disc herniation (often calcified), OPLL, arteriovenous malformations, spinal tumors
- Lumbar: vascular claudication, spinal metastasis, polyneuropathy. [3]
Failure of formation
Congenital scoliosis
As mentioned above there are different types of scoliosis. The following are as a failure of formation:
- A Hemivertebra, which is a complete unilateral failure of the vertebral formation that can be:
○ Fully segmented
○ Partially segmented
○ Non-segmented
A hemivertebra can be further described as incarnated or non-incarnated. - A wedge vertebra is a partial unilateral failure.[33]
Congenital kyphosis
- idem failure of segmentation
- Klippel-Feil syndrome
- Congenital muscular torticollis [34]
- Wildervanck syndrome
- MURCS association
- Turner or Noonan syndrome
- Morquio syndrome
- Tuberculosis of the cervical spine
- Nevoid basal cell nevus syndrome
- Crouzon syndrome
- Apert syndrome
- Binder syndrome
- Oculo-auriculo-vertebral spectrum [35]
- Osteopetrosis
- Leukemia [36]
- Dysosteosclerosis [37]
Diagnostic Procedures
There are several different procedures that can be used to carry out the imaging of the spine. The choice of imaging depends on what is required to be analysed, such as bone vs spinal canal. In children, it is important to start with less invasive procedures such as US, due to their cartilage and non-ossified bones. [30]
X-Rays are useful for showing structural deformities such as hemivertebrae, butterfly vertebra, or incomplete fusion of posterior elements. X-ray is used if no imaging of the spinal cord is required. For scoliosis, erect posterior-anterior frontal and/or lateral views (with breast shielding) are usually obtained. [38]
MRI is most frequently used for imaging of the spine in adults as the spinal canal and its content can be analysed.
Basu et al. suggest that MRI and echocardiography should be an essential part in any evaluation of patients with congenital spinal deformity, [39] with numerous other studies demonstrating the high degree of confidence with MRI use. [40][41][30][42][43]
CT Scans continue to be the preferred method for the assessment of localised bony abnormalities, or a calcified component, of the spinal canal, foramina, neural arches, and articular structures. [38]
Outcome Measures
These are the most commonly used questionnaires with patients who have undergone spinal surgery, the most common treatment for congenital spine deformities.
Examination
The physical examination of a patient with kyphosis has various components: [48]
- postural analysis, which may reveal a gibbus deformity or a round back.
- palpation to assess for spinal abnormalities and may identify tenderness of the paraspinal musculature, which is often present.
- range of motion during flexion, extension, side bending and spinal rotation of the back. Asymmetry is be noted. Adam’s forward bend test may reveal a thoracolumbar kyphosis, although Karachalios et al suggested that this test is not a sure diagnostic criterion for the early detection of scoliosis due to the unacceptable number of false-negative findings. [49] Rather, the combined back-shape analysis methods is recommended.
Côté Pierre et al. however, suggested that the Adam’s forward band test is more sensitive compared to the scoliometer and consider it to be the best non-invasive clinical test to evaluate scoleosis. [50]
A complete neurologic evaluation should also be carried out to rule out in the presence of intraspinal anomalies [48]. Patients with congenital spondylolisthesis show deficits in their neurological examinations. [5] A neurological evaluation includes an evaluation of pain, numbness, paresthesia, tingling, extremity sensation and motor function, muscle spasm, weakness and bowel/bladder changes. [3]
For the examination of spina bifida oculta, X-ray examination is the only valid test to confirm this type of neural tube defect. [2]
Medical Management
The natural history, the character and location of the deformity ultimately influence the choice of treatment.[1] Spinal instrumentation for congenital spine deformity cases is safe and effective, [51][52] as is growing rod surgery for selected patients with congenital spinal deformities. [53][54] The size and weight of the patient determines the size of the spinal implants, whereas the surgical fixation anchors are determined by the anatomy of the patient and the anomalies present. [52] The complications associated with the use of this spinal instrumentation are infrequent and the curve correction, length of immobilisation and fusion rate is improved.[52]
Growing rod surgery
Growing rod surgery is one of the options for the correction of scoliosis, a modern alternative treatment for young children with early onset scoliosis. Elsebai HB et al. focused on its use in progressive congenital spinal deformities. The incidence of complication remained relatively low [53][54] and is also recommended for patients where the primary problem is at the vertebral column.
Expansion thoracostomy and VEPT
For severe congenital spine deformations, when a large amount of growth remains, expansion thoracostomy and VEPTR (a curved metal rod designed for many uses), are the most appropriate choice. These methods are used when the primary problems involve the thoracic cage, for example when there are rib fusions and/or with developing Thoracic Insufficient Syndrome, [54] but the incidence of complications using VEPTR is, however, relatively high.[55]
Resection and fusion
For treating congenital scoliosis caused by hemivertebra posterior hemivertebra, resection and monosegmental fusion appears to be effective. This treatment results in an excellent correction in both the frontal and sagittal planes. [56] Early surgery is typically prescribed as a treatment for children with congenital scoliosis, even though there is little evidence for its long term results. Evidence base is also lacking to confirm the hypothesis that spinal fusion surgery for children with congenital scoliosis is effective Additionally, there are conflicting data about the safety of hemivertebra resection and segmental fusion which uses pedicle screw fixation. [55]
Physical Therapy Management
Physical therapy helps patients to continue with daily activities. There are various interventions for congenital spine deformities, such as bracing and postural training and surgical, as described under medical management.
Scoliosis:
Various approaches for conservative management can be considered, although opinions are divided for the its early treatment. Braces cannot correct a spinal curve, but they can be used for preserving the spine’s shape and delaying early surgery. [57] LoE 5 [24] LoE 2a. It is important, therefore, that conservative management is considered before surgery. External support with casts or braces is considered to be successful in only a small percentage of cases and that surgery is the definitive treatment [58] LoE 2b, although this is refuted by Fender et al. who claim that surgical intervention during infancy is the aim of the treatment before compensatory curves can develop. [59] LoE 5
Few cases have been reported on the influence of conservative treatment. Kaspiris et al claim that segmentation failure should be treated with early surgery before growth in puberty. For scoliosis due to failure of formation, further investigation is needed to determine whether a conservative approach would be necessary.[60] LoE 2b. More research is needed to prove the effectiveness of conservative treatment in congenital scoliosis.
Numerous brace designs have been developed for the spine. The type of brace chosen depends on different factors such as: location of the curve, flexibility of the curve, number of curves and position and rotation of some of the vertebrae. Braces have to be worn until the patient stops growing, then surgery can take place. [61] LoE 5
Milwaukee brace: used for scoliosis. The brace is initially worn for a limited number of hours until the patient is can comfortably wear it all day and night to eventually lead a normal life. The brace may only be removed once a day. Creswell suggested 2 exercises that the patient should do while wearing this brace:
- Standing, displace the trunk away from the primary lateral pressure pad.
- Standing, breathe in and expand chest posteriorly on side opposite to primary pressure pad. [61] LoE 5
When the brace can be discarded, the patient should gradually reduce its use, so long as their posture remains unchanged. During periods where the brace is not worn, it is recommended that the patient is as active as possible. [61] LoE 5
Until surgery takes place exercise has to be done twice daily to maintain and improve mobility in multiple directions, especially for spinal extension and strength of the trunk muscles. There are different sorts of exercises for every age. Creswell suggests the Klapps’ protocol: [61] LoE 5
- Teach correct pelvic tilting in supine lying, prone lying, standing, and kneestanding.
- Teach the patient to correct their posture infront of a mirror, so that the shoulders are directly above the pelvis.
- If the primary curve is deteriorating or measures 25° or more, patients aged 2 1/2 years upwards are fitted with a Milwaukee Brace. Once this is fitted, it is worn day and night and is removed only once daily for bathing and exercises.
- If at any time the curve continues to deteriorate rapidly even with a Milwaukee Brace, the patient may have a corrective localised plaster jacket applied for a period of 3 to 4 months. This is put on with the patient lying on a frame, with traction. Jacket use usually considerably improves the scoliosis. When the jacket is removed, Milwaukee Brace use is resumed immediately and exercises are again done regularly.
- The patient stays in the Milwaukee Brace for a number of years, until surgery is undertaken, or until all the following criteria are satisfied:
- They are no longer growing
- They are able to easily maintain the same posture out of the brace as in it
- X-rays of the pelvis show that the iliac apophyses have closed posteriorly. [61] LoE 5
Post surgery rehabilitation is essential. Children who undergo anterior and posterior hemivertebral excision have to wear a plaster for 3 months to maintain the spinal correction. After 3 months of immobilisation, retraining of the postural muscles is crucial to maintain the stability of the spine. [62] LoE 2b
Neural Tube Defects:
As with spina bifida, therapy depends on the type of condition. Spina bifida occulta does not require any treatment. With spina bifida aperta, surgery is done immediately after birth. Physiotherapy is needed following surgery for strength and mobility to make sure that the child to walk normally when older. Wearing a brace can also help to improve control and function.
According to Strohkendl et al, children with spina bifida also have shortage of environmental experience. Specifically selected and individualised physical education, depending on the child’s age, can help a child to acquire the necessary mobility and social experiences. This is to make sure that there is fulfilment of their individual inclinations, encouragement of independence, development of community life and the fulfilment of everyday tasks, [63] LoE 5
Kyphosis:
If kyphosis isn’t treated, the curve will continue to progress at approximately 7 degrees each year. During the adolescent growth spurt, the curve will reach its maximum orientation and brace treatment during this period was seen to be ineffective. [64] LoE 5
When operative treatment doesn’t take place, patients with myelomeningocele and congenital kyphosis can be managed by modified wheelchairs and orthoses. Patients are able to function with reasonable comfort with these wheelchair modifications.
Clinical Bottom Line
Congenital spine deformities are identified in the uterus or at birth which are the result of anomalous vertebral development in the embryo. They can classified into three groups:
- due to neural tube deformities/defects,
- due to failure of segmentation
- due to failure of formation.
Numerous factors such as environmental factors, genetic factors, vitamin deficiency, chemicals and drugs, singly or in combination, have been implicated in the development of congenital abnormalities during the embryonic period. Diagnose imaging is used to confirm a deformity, such as ultrasound, X-rays, MRI and CT scans.
With children, it is important to start with a less invasive procedure due to their cartilage and non-ossified bones, such as ultrasound. Diagnose is completed with observation, palpation, assessment of range of motion of the spine and a neurological evaluation. If the patient has an open deformity due to a tube defect, surgery is done directly after birth or surgery can be delayed in the case of a closed deformity due to neural tube defect. There is some debate over the treatment of congenital spine deformities due to a failure of segmentation/formation with some clinicians recommending surgery during infancy, whereas others would initially treat using conservative management techniques, such as braces and exercise, before considering surgery.
Congenital scoliosis presents a major challenge to the clinician due the wide variety of primary and secondary abnormalities. These abnormalities develop during fetal development and treatment often necessitates numerous tests and thorough, repetitive examinations.
References
- ↑ 1.01.1 Alexander PG. and Tuan RS. (2010). Role of environmental factors in axial skeletal dysmorphogenesis. Birth Defects Res C Embryo Today, 90 (2), pp 118-132
- ↑ 2.02.12.2 AKBARNIZ B. A. et al. (2011). The Growing Spine, Management of Spinal Disorders in Young Children. Springer, p. 247, 263, 318.
- ↑ 3.03.13.23.33.43.53.63.7 BOOS N. and AEBI M. (2008) Spinal Disorders, Fundamentals of Diagnosis and Treatment, Springer, p. 311, 434, 695-696
- ↑ 4.04.1 SCHWARTZ E.S. and ROSSI A., 2015 “Congential spine anomalies: the closed spinal dysraphisms“, Advances in Pediatric Neuroradiology, vol. 45, supp. 3, p. 413-419,
- ↑ 5.05.15.25.35.45.55.65.7 Kaplan K.M et al. (2005). Embryology of the spine and associated congenital abnormalities. Spine J, 5 (5), pp 564-576.
- ↑ Goldstein I. (2005). Hemivertebra: prenatal diagnosis, incidence and characteristics, Fetal Diagn Ther,. 20 (2), pp 121-6
- ↑ Kawakami N, et al. (2009). Classification of congenital scoliosis and kyphosis: a new approach to the three-dimensional classification for progressive vertebral anomalies requiring operative treatment, Spine (Phila Pa 1976), 34 (17), pp1756-65
- ↑ Au K.S. et al. (2010). Epidemiologic and genetics aspects of spina bifida and other neural tube defects. Dev. Disabil. Res Rev, 16 (1), pp 6-15
- ↑ Swenson L. (2012). Neural tube defects. Nursing Care of the pediatric neruosurgery partient. 4, 119-139
- ↑ 10.010.1 Sewell, M. J. et al. 2015, “Neural Tube Dysraphism: Review of Cutaneous Markers and Imaging. “, Pediatric Dermatology, vol 32, pp 161–170,
- ↑ 11.011.1 McComb J.G., Spinal and cranial neural tube defects. Neurosurgical Issues for the pediatric patient, 1997;4(3):156-166
- ↑ 12.012.112.2 Amarante M.A. et al. (2012). Management of urological dysfucntion in pediatric patiens with spinal dysraphism: review of the litarature. Neurosurg. Focus, 33 (4).
- ↑ Marks D.S. et al. (2009). The natural history of congenital scoliosis and kyphosis. Spine (Phila Pa 1976). 34 (17), pp 1751-1755
- ↑ Fender, D. et al. Jan 2014 “Spinal disorders in childhood II: spinal deformity“, Surgery (Oxford), Vol. 32, Nr1, pp 39–45,
- ↑ Klemme WR et al. (2001). Hemivertebral excision for congenital scoliosis in very young children. J Pediatr Orthop. 21 (6), pp761-764.
- ↑ Lonstein J.E. (1999). congenital spine deformaties: scoliosis, kyphosis, and lordosis. orthopedic clinics of north america, 30 (3), pp387-405
- ↑ Fichter M. A. et al. 2008 “Fetal spina bifida repair–current trends and prospects of intrauterine neurosurgery”, Fetal Diagnosis and Therapy, vol 23, nr 4 , pp 271–286,
- ↑ Burke R., Liptak G. (2011) . Providing a Primary Care Medical Home for Children and Youth with Spina Bifida, American Academy of Pediatrics, 128, pp 1645-1657
- ↑ McMaster Mj., singh H. 1999 “Natural History of Congenital Kyphosis and Kyphoscoliosis. A Study of One Hundred and Twelve Patients” ,Journal of Bone no People and Joint Surgery, vol 81 , nr 10, pp 1367 -83,
- ↑ Elizabeth D Agabegi, Agabegi, Steven S. Step-Up to Medicine. 3de edition. Baltimore:Lippincott Williams & Wilkins, 2008
- ↑ Goldstein I. (2005). Hemivertebra: prenatal diagnosis, incidence and characteristics, Fetal Diagn Ther,. 20 (2), pp 121-6
- ↑ Hensinger RN. (2009). Congenital scoliosis: etiology and associations. Spine (Phila Pa 1976)., 34 (17), pp1745-1750.
- ↑ Oskouian R.J. Jr. et al. (2007). Congenital abnormalities of the thoracic and lumbar spine. Neurosurg, Clin. N. Am., 18 (3), pp 479-498,
- ↑ 24.024.124.2 Rolton D. et al. 2014, “Scoliosis: a review Paediatrics and Child Health“, Vol 24, nr 5, pp 197–203, LoE 2a
- ↑ 25.025.125.2 Salih M.A. et al. 2014, “Classification, clinical features, and genetics of neural tube defects“,Saudi Med. J., vol 35, pp5-14,
- ↑ McComb J.G., Spinal and cranial neural tube defects. Neurosurgical Issues for the pediatric patient, 1997;4(3):156-166
- ↑ Rolton D. et al. 2014 “Scoliosis: a review Paediatrics and Child Health“, Vol 24, nr 5, pp 197–203
- ↑ Fichter M. A. et al. 2008 “Fetal spina bifida repair–current trends and prospects of intrauterine neurosurgery”, Fetal Diagnosis and Therapy, vol 23, nr 4 , pp 271–286
- ↑ Priya K. et al. (2015). congenital kyphosis in thoracic spine secondary to absence of two vertebral bodies, J clin diagn res, 9 (1).
- ↑ 30.030.130.2 SORANTIN E. et al., 2008 “MRI of the Neonatal and Paediatric Spine and Spinal Canal“, European Journal of Radiology, vol. 68, nr. 2, p. 227 – 234
- ↑ Venkatatamana NK., “Spinal dysraphism“, Journal of Pediatric Neuroscience, vol. 6, supp. 1, p. 31-40, 2011.
- ↑ Schwartz E.S. and Rossi A., “Congential spine anomalies: the closed spinal dysraphisms“, Advances in Pediatric Neuroradiology, vol. 45, supp. 3, p. 413-419, 2015.
- ↑ Debnath UK. et al., “Congenital scoliosis – Quo vadis? “, Indian Journal of Orthopaedics, vol. 44, nr. 2, p. 137 -147, 2010
- ↑ Gray E et al. “Congenital fusion of the cervical vertebrae“, Surg Gynecol Obstet, 1964 vol118, pp373-85, feb .
- ↑ Naikmasur V.G. et al., “Type III Klippel-Feil syndrome: case report and review of associated craniofacial anomalies“, Springer, vol. 99, nr. 2, p. 197 – 202, 2011
- ↑ Taner S. et al., “Diagnosis: Infantile Malign Osteopetrosis”, Turkish Journal of Hematology, vol. 31, nr. 3, p. 335 – 336, 2014
- ↑ Wilson C.J. and Vellodi A., “Autosomal recessive osteopetrosis: diagnosis, management, and outcome“, Archives of Diseases in Childhood, vol. 83, p. 449 – 452, 2000
- ↑ 38.038.1 Patrick D Barnes. (2009). Pediatric radiology : chapter 9, spine imaging. (3). Mosby
- ↑ Basu S.et al., 2002 “Congenital Spinal Deformity: A Comprehensive Assessment at Presentation“, Spine, Vol 27, nr 2, pp 2255-2259
- ↑ Fabry G. (2009). Clinical practice: the spine from birth to adolescence, Eur J Pediatr, 168 (12), pp1415-1420
- ↑ Durand D.J., Huisman T.A., Carrino J.A. (2010). MR imaging features of common variant spinal anatomy, Magn Reson Imaging Clin N Am, 18 (4), pp717-726
- ↑ . Grimme J.D. (2007). Castillo M. Congenital anomalies of the spine. Neuroimaging Clin N Am, 17 (1), pp 1-16
- ↑ Brophy JD et al. (1989). Magnetic resonance imaging of lipomyelomeningocele and tethered cord, Neurosurgery, 25 (3), pp336-340
- ↑ SVENSSON E. et al., 2009 “The Balanced Inventory for Spinal Disorders: The validity of a Disease Specific Questionnaire for Evaluation of Outcomes in Patients With Various Spinal Disorders“, Spine, vol. 34, nr. 18, p. 1976 – 1983
- ↑ 45.045.145.2 COPAY A.G. et al.2008 “Minimum Clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study Questionnaire Short Form 36, and Pain Scales“, The Spine Journal, vol. 8, nr. 6, p. 968 – 974, .
- ↑ 46.046.146.2 DEVIN C.J. and McGIRT M.J.2015, “Best evidence in multimodal pain management in spine surgery and means of assessing postoperative pain and functional outcomes“, Journal of Clinical Neuroscience, vol. 22, nr. 6, p. 930 – 938,
- ↑ FARLEY F.A. M.D. et al .2014, “Congenital Scoliosis SRS-22 Outcomes in Children Treated With Observation, Surgery, and VEPTR“, Spine, vol 39., nr. 22. p. 1868 – 1874,
- ↑ 48.048.1 Chaén G., Dormans J.P. (2009). Update on congenital spinal deformities: preoperative evaluation. Spine (Phila Pa 1976). 1;34(17), pp1766-1774
- ↑ Karachalios Theofilos et al.,1999 “Ten-Year Follow-Up Evaluation of a School Screening Program for Scoliosis: Is the Forward-Bending Test an Accurate Diagnostic Criterion for the Screening of Scoliosis? “, Spine, Vol 24, nr22, pp 2318
- ↑ . Côté Pierre et al., “A Study of the Diagnostic Accuracy and Reliability of the Scoliometer and Adam’s Forward Bend Test“, Spine, Vol. 23, nr. 7, pp 796–802, 1 April 1998
- ↑ Hedequist D.J. (2009). Instrumentation and fusion for congenital spine deformities, Spine (Phila Pa 1976), 1;34 (17), pp1783-90
- ↑ 52.052.152.2 Hedequist D.J. et al. (2004). The safety and efficacy of spinal instrumentation in children with congenital spine deformities, Spine (Phila Pa 1976), 15;29 (18), pp 2081-2086
- ↑ 53.053.1 Elsebai HB et al.,2011 “Safety and Effficacy of Growing Rod Technique for Pediatric Congenital Spinal Deformities“, J Pediatr Orthop, vol 31, nr 1, pp 1-5. Jan-Feb,
- ↑ 54.054.154.2 Yazici M. and Emans J.2009, “Fusionless Instrumentation Systems for Congenital Scoliosis: Expandable Spinal Rods and Vertical Expandable Prosthetic Titanium Rib in the Management of Congenital Spine Deformities in the Growing Child“, Spine, Vol 34, Nr 17, pp 1800-1807
- ↑ 55.055.1 Moramarco M and Weiss HR. (2015). Congenital Scoliosis, Curr Pediatr 2015 Nov 17
- ↑ Zhu X. et al. 2014, “Posterior hemivertebra resection and monosegmental fusion in the treatment of congenital scoliosis. “, Article from Annals of The Royal College of Surgeons of England, Vol 96, Nr5, pp. 41-44
- ↑ Götze HG. (1978). Prognosis and therapy of the congenital scoliosis, Z Orthop Ihre Grenzgeb., 116 (2), pp258-266 LoE 5
- ↑ Leatherman K. et al. Two-stage corrective surgery for congenital deformities of the spine. journal of bone and joint surgery, pp 324-328 LoE 2b
- ↑ Fender, D. et al. 2014 “Spinal disorders in childhood II: spinal deformity“, Surgery (Oxford), Vol. 32, Nr1, pp 39–45, LoE 5
- ↑ Kaspiris A., Theodoros B. Grivas, Weiss H-R. and Turnbull D.2011, “Surgical and conservative treatment of patients with congenital scoliosis: a search for long-term results“, Scoliosis, Vol. 6, nr. 12, pp. 1-17, . LoE 2b
- ↑ 61.061.161.261.361.4 Creswell E.J.1969, “The conservtaive managment of scoliosis in children and adolescents, and the use of the milwaukee brace “, Australian Journal of Physiotherapy, Vol. 15, Nr.4, pp 149–152, LoE 5
- ↑ Klemme WR et al. (2001). Hemivertebral excision for congenital scoliosis in very young children. J Pediatr Orthop. 21 (6), pp761-764 LoE 2b
- ↑ trohkendl H. et al. 1978, Physical education for spina bifida children in special schools for the physically handicapped (primary school). Int J Rehabil Res., 1(1), P39-58 LoE 5
- ↑ Winter R.B, Moew J.H, Wang J.F,(1973). Congenital Kyphosis its natural history and treatment as observed in a study of one hunderd and thirthy patients. J Bone Joint Surg Am, 55 (2), PP 223 -274 LoE 5