Definition / Description
Osteoporotic (fragility) fractures are fractures that result from mechanical forces that would not ordinarily result in a fracture, known as low-level (or low-energy) trauma according to National Institute for Health and Care Excellence (NICE) clinical guidelines[1].
Osteoporosis is a disease that is characterised by low bone mass[2], causing bones to be more fragile and likely to fracture[3]. The word osteoporosis means porous bone[4]. One of the significant consequences of osteoporosis is fractures. Common types of fracture include wrist fractures, hip fractures and vertebral fractures[2][5].
Osteoporosis in older adults is caused by an imbalance of bone resorption in excess of bone formation. The dominant factor leading to bone loss in older adults appears to be gonadal sex steroid deficiency, with multiple genetic and biochemical factors, such as Vitamin D Deficiency or hyperparathyroidism, that may accelerate bone loss.
Conditions that adversely affect growth and development may limit development of peak bone mass and accelerate subsequent bone loss. Studies of bone microarchitecture have shown that trabecular bone loss begins in the third decade of life, before gonadal sex steroid deficiency develops, whereas cortical loss typically begins in the sixth decade, about the time of menopause in women and about the same age in men.
Antiresorptive agents for the treatment of osteoporosis act primarily by limiting osteoclast activity, whereas osteoanabolic agents, such as teriparatide, act primarily by stimulating osteoblastic bone formation. Clinical investigation of new compounds for the treatment of osteoporosis is mainly directed to those that stimulate bone formation or differentially decrease bone resorption more than bone formation. Therapies for osteoporosis are associated with adverse effects, but in patients at high risk of fracture, the benefits generally far outweigh the risks.
Important: Bone mass alone does not explain the risk of fractures in at least 50% of osteoporosis cases; bone quality also plays a role[6].
Clinically Relevant Anatomy
Due to the osteoporosis that made the bone density low and made the bone weak (higher activity of osteoclasts and lower activity of osteoblasts), the vertebra can ‘collapse’. This is called a vertebral body fracture. The fracture can lead to hyperkyphosis or hyperlordosis depending on the vertebral level. People with osteoporosis break down bone faster than it can regenerate. Trabecular bone is more active and because of this, trabecular bone is more likely to be affected. When people stand up causing pressure on the spine, the weak trabecular bone of the spine body’s can start to collapse, leading to an osteoporotic vertebral fracture. This fracture occur on the posterior part of the vertebra or the vertebral body. Because of the decrease of height of the vertebra, the anterior longitudinal ligament and posterior longitudinal ligament lose tension. This can cause vertebral instability.
Epidemiology / Etiology
Osteoporotic vertebral fractures are a significant problem. The number of vertebral fractures in the UK in 2010 was estimated to be 30,994, this number is expected to increase by 17.9% by 2020[8]. In America 700,000 vertebral fractures occur within the population who have osteoporosis[9]. In addition to this once a vertebral fracture has been sustained the risk of subsequent vertebral, hip or wrist fractures increase[10].
Osteoporosis affects up to 30% of women and 12% of men at some point in their lives. Two of the most important risk factors are increasing age and female gender, although other common and potentially modifiable risk factors include long-term corticosteroid therapy, chronic inflammatory disease, malabsorption and untreated premature menopause[11].
There is a higher prevalence for osteoporotic vertebral fractures for elderly and females with equal frequency in both Caucasian and Asian women. One out of four postmenopausal women suffer osteoporotic vertebral fractures. Osteoporotic vertebral fractures are multiple in up to 20% of patients and affect more than 20% of those older than 50 years with slight female prevalence that markedly increases when they age above 80 years[12].
Symptomatic osteoporotic vertebral fractures affect 1 in 6 women and 1 in 12 men during their lifetime. In Europe the annual incidence of osteoporotic vertebral fractures is 10.7 per thousand for women and 5.7 per thousand for men. Statistically, men got less osteoporotic fractures then women because men lose less bone density when they age. These figures may underestimate the actual size of the problem as most osteoporotic vertebral fractures go unreported and undiagnosed. With the prevalence of osteoporosis predicted to increase by 2021, a rise in associated fractures is also likely. The main causes and risk factors of fractures and vertebral fractures are a decay in bone density and previous fractures[13][14].
Looking more closely to the specific regions of the spine and the prevalence of osteoporotic fractures, we can conclude that osteoporotic fractures in the thoracic spine are mostly affected. There is a prevalence of 2,4/1000 (age 35-44), 5,1/1000 (age 44-75), 29/1000 (age > 75) in the thoracic spine. (Corresponding figures for men: 5,2/1000, 15/1000, 28/1000)[15].
The below short video gives a brief overview of compression fractures
Clinical Presentation
Symptoms of vertebral fracture can include pain, curvature of the spine, height loss, difficulties with ADLs, loss of self-esteem related to changes in body shape, and in cases of severe kyphosis respiratory and gastrointestinal problems[6][17] in addition to vertebral fractures being linked to mortality[18].
Back pain is common in elderly patients. Most vertebral fractures go unrecognized, with symptoms attributed to degenerative change. This is particularly so as osteoporotic vertebral fractures classically occur during normal day-to-day activities such as bending, walking or lifting relatively light objects. Three quarters of patients with vertebral fracture do not seek medical attention and even up to 2/3 of vertebral fractures may not result in notably severe symptoms [19].
Vertebral compression fractures (VCF) are characterised by loss of height and acute pain. Height loss of the osteoporotic fractured vertebra may be mild (20-25%), moderate (25-40%) or severe (> 40%). It commonly affects the thoracolumbar region, though any vertebra may be disturbed.
The pain of acute fracture usually lasts 4 to 6 weeks with intense pain at the site of fracture. The pain resolves over a period of six to 12 weeks. Chronic pain may also occur in patients with multiple compression fractures, height loss and low bone density. Although this is probably due to structural changes or osteoarthritis.
Osteoporotic vertebral fractures are mostly wedged with anterior or mid-body shortening, and minimal posterior vertebral body curbing. However discoid biconcave or crush-like fractures may also be seen.
Radiographic VCF may not be symptomatic. The greater the deformity, the greater the likelihood of pain and disability. As height is lost, patients experience discomfort from the rib cage pressing downward on the pelvis. Patients develop an exaggerated thoracic kyphosis and/or an exaggerated lumbar lordosis[19]. The reduced thoracic space may result in decreased exercise tolerance and reduced abdominal space may give rise to early satiety and weight loss.
Sleep disorders may also occur. Patients lose self esteem. Self care may become difficult. They are often depressed. They become fearful of further fracture. They have distorted body image and poor health perception. Patients with one vertebral fracture are at increased risk of peripheral fracture and further vertebral fracture. The aims of acute management are to reduce symptoms and mobilise the patient as quickly as possible. Long-term goals are to maintain or increase skeletal mass and improve mobility and function[12][20][21].
Together with an increased morbidity, vertebral fractures are also associated with increased mortality[19].
Despite the clear undisputed clinical relevance of vertebral fractures, these remain underdiagnosed in everyday clinical practice[22]. Two main reasons account for this inadequacy. First, as mentioned, vertebral fractures frequently do not present as a clinically recognizable event. Second, many radiologically apparent vertebral fractures go unreported. Of patients aged more than 60 years attending emergency departments, about 1/6 had a moderate to severe vertebral fracture evident on lateral chest radiographs of which only about 1/2 were noted on radiology reports and fewer still received specific medical attention[23].
Differential Diagnosis
Vertebral fractures aren’t only due to osteoporosis. It’s possible that a vertebral fracture is caused due to[24]:
● Osteomalacia/ Rickets: softening of the bones due to a Vitamin D deficiency in adults. In time it can result in decalcification of the bone, fractures, skeletal deformities, bone pain and muscle weakness. Rickets is a similar condition in children.
● Paget’s Disease: Bone is resorbed and formed at an increased rate, which may lead to pain, fractures, deformity, headaches, dizziness, osteoarthritis, spinal stenosis, and increased size of clavicle are a few common presentation.
● Bone Infection
● Pediatric osteogenesis imperfecta
● Cancer: Low-energy fractures may also be result of bone cancer or metastatic cancer.
● Multiple Myeloma
● Renal osteodystrophy
● Scurvy: Vitamin C deficiency
Diagnostic Procedures
The diagnosis of osteoporosis can be confirmed by Dual Energy X-ray Absorptiometry (DXA). DXA should only be performed in patients who have an increased risk of fracture on the basis of clinical risk factors. DXA should be considered if the 10-year risk of major osteoporotic fracture is > 10%. If the Bone Mineral Density (BMD) T-score valued by DXA at the lumbar spine, femoral neck or total hip are at or below -2.5 then the diagnosis of osteoporosis is confirmed. Vertebral fractures are generally taken as diagnostic of osteoporosis, even if spine BMD values are not in the osteoporotic range[11].
There is evidence that fractures occur in glucocorticoid-induced osteoporosis at higher levels of bone mineral density (BMD) than in postmenopausal osteoporosis so therapy should be considered in patients with a BMD T-score of [11].
A patient with presence of a prevalent fragility fracture despite T-score >-2.5 is also diagnosed with osteoporosis. The presence of an low-energy, insufficiency vertebral fracture overrides bone densitometry and is an indication to treat for osteoporosis[19].
Category T-score
Normal > -1.0
Osteopenia -1.0 > x > -2.5
Osteoporosis -2.5 >
Severe Osteoporosis -2.5 > + insufficiency fractures
Radiography is quick, widely available and of low cost and is a good imaging modality to diagnose vertebral fracture. Lateral spinal radiography will usually suffice and should include a high quality standardized image of the C7-S1 vertebrae[19].
Preferentially, conventional X-rays are crucial for diagnosing and grading osteoporotic vertebral deformities and for differential diagnosis during assessment for osteoporotic deformity. However, more advanced imaging techniques such as Computed Tomography (CT), Bone Scintigraphy (BS), and Magnetic Resonance Imaging (MRI) may be required to further investigate the etiology in some of these deformities as well as to differentiate chronic from acute fractures, to assess compromise of the spinal canal, and for follow-up after specific treatments such as vertebroplasty[25].
Deleskog L et al concluded that vertebral fracture assessment (VFA) by DXA is inferior relative to X-ray in visualizing vertebrae properly in the upper spine. This resluts in vertebrae not being assessable for analysis and reduced diagnostic performance in detecting fractures[26].
Torres and Hammond concluded that Computed Tomography (CT) or Magnetic Resonance (MR) are needed to differentiate between a low-intensity vertebral fracture caused by osteoporosis or a low-intensity vertebral fracture caused by neoplastic metastasis. This is crucial for a population of elderly with a history of cancer[27].
Outcome Measures
R. Buchbinder et al. used the following outcome measures to evaluate the progression of a patient who suffers from an osteoporotic vertebral fracture[28]:
- Visual analogue scale for overall pain (VAS).
- Quality of Life questionnaire: this can be measured with the use of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). An other possibility is to use the Assessment of Quality of Life (AQoL) questionnaire or the European Quality of Life–5 Dimensions (EQ–5D) scale.
- Physical functioning: measured bij a modified 23-item version of the Roland–Morris Disability Questionnaire.
- Pain at night and at rest (VAS score)
- According to Lavelle EA, Cheney and Lavelle WF [29] the American Society of Anesthesiologists Physical Status score (ASA) is a predictive outcome measure of mortality in a surgical population of vertebral compression fractures. The same study also concluded that the Charlson Comorbidity Index (CCI) was highly predictive of mortality in a non-surgical population of vertebral compression fractures.
Examination
Clinical assessment of vertebral fractures is generally poor and reliance is made on imaging studies for diagnosis[20].
However in a study of James Langdon et al. they validated 2 tests that ensure and enable the practioner to predict more accurately wich patients have an acute vertebral fracture[30].
- Closed-fist percussion sign[30]
This test has a sensitivity of 87,5% and a specificity of 90%, which is good. The examinator stands behind the patiënt and the patiënt stand in front of a mirror so the examinator can see the reaction of the patiënt. Firm closed-fist percussion is used to examine the entire lenght of the spine. The clinical sign is positive when the patiënt complains of a sharp, sudden,
fracture pain.
2. The supine sign[30]
This test has a sensitivity of 81,25% and a specificity of 93,33%, wich is also pretty good. The patiënt is asked to lie supine with only one pillow for the head. The clinical sign is positive when the patiënt is unable to lie supine due to severe pain.
Medical Management
Good quality evidence supports that several medications (e.g. bisphosphonates) for bone density reduce fracture risk. Nevertheless side effects vary among drugs. (Crandall CJ, 2014: LoE 1A) [31].
At first, conservative treatment still is the method of choice. In case of resulting deformity, sintering and persistent pain vertebral cement augmentation techniques today are widely used.Treatment after vertebral fracture should include appropriate pain management and possibly bracing[32]. Forms of conservative treatment commonly used in these patients include bed rest, analgesic medication, physiotherapy and bracing. Vertebral fractures can also be treated surgically using vertebroplasty and kyphoplasty[31][33]. Percutaneous vertebroplasty (VP) began as a simple, low-cost procedure that aimed to provide pain relief for patients with vertebral compression fractures (VCF). Balloon Kyphoplasty (KP) was introduced later, and was presented not only as a ‘‘pain killer,’’ but also as a deformity correction procedure[33].
The vidoe clip below tells of an elderly lady with an osteoporotic insufficiency fracture and an animated version of a vertebroplasty.
Frequently used analgesia are paracetamol or salicylates and non-steroidal anti-inflammatory drugs (NSAIDs). The risk of gastrointestinal bleeding and insufficiency should be taken into account when prescribing NSAIDs[33]
There is only low or very low-quality evidence on the efficacy of non-surgical treatment of symptoms of acute osteoporotic VCFs. Immediate- and short-term effects of opioids on pain were found inconsistent across trials with different comparators. Low-quality evidence supports immediate- and short-term effects of an NSAID on reducing pain intensity. There is low-quality evidence indicating the value of spinal orthoses for pain relief and disability at medium term. At present, there is insufficient evidence to inform conservative care for acute pain related to VCF. This was concluded by Rzewuska M. and colleaguesafter a 2015 systematic review with meta-analysis[32].
The primary goal of bracing is to reduce pain by stabilising the spine and limiting progression of the deformity. A spinal orthosis should reduce gross spinal movement and segmental movement at the injured segment. Bracing allows a reduction in the period of bed rest, facilitating earlier mobilisation according to Kim DH and colleagues[35]. An ideal brace should be light-weight and easy to put on. It should be comfortable to obtain patient compliance and it has to avoid respiratory impairments. Examples of braces are the Jewett brace, Taylor brace and cruciform anterior spinal hyperextension (CASH) orthosis, they keep the spine in hyperextension. Even though bracing is widely used in these patients, its use is still opinion-based. Important: the evidence for a conservative spinal orthosis in patients with osteoporotic vertebral fractures is based on evidence from studies in patients with non-osteoporotic vertebral burst fractures[33].
We could only find one study evaluating spinal orthoses in the treatment of osteoporotic VCFs. Pfeifer, Begerow and Minne[8] performed a prospective randomised trial using a thoracolumbar orthosis (TLO) to manage VCFs in women with postmenopausal osteoporosis. They reported increased trunk muscle strength and improvement of posture and body height in patients treated with an orthosis. They noted that patients had less pain, a better quality of life and restoration of their ability to perform daily living tasks.
In a vertebroplasty bone cement, usually polymethylmethacrylate (PMMA), is injected into the vertebral bone. In a kyphoplasty a balloon is inserted into the vertebral body, the balloon is inflated to attempt to re-establish normal height and posture, the balloon is remove and cement injected. It permits kyphosis correction if performed within 3 months post-fracture. Height restoration is not a perquisite for pain control[17].
Indications for surgery are: failed medical treatment for pain control, patients with co-morbidities that make prolonged bed rest dangerous, patients with fractures that fail to heal, resulting deformity, an unstable fracture (pattern) and involvement of spinal cord[10]. This was proved in both retrospective and prospective studies as well as in meta-analysis[6][8][36]. The procedures are proved to be cost effective[9].
Buchbinder R. et al (2009) performed a randomized controlled trial in which they compared a vertebroplasty surgery with a sham treatment in patients who suffer from an osteoporotic vertebral fracture. There were significant improvements at all follow-up measurements for several outcome measures: overall pain, pain at night, pain at rest, physical functioning and quality of life. They concluded that there is no beneficial effect of vertebroplasty as compared with a sham procedure in patients with painful osteoporotic vertebral fractures[9]. This has been confirmed by a Cochrane review[6].
Diamond TH. et al (2003) compared a conservative and percutaneous vertebroplasty treatment for patients with an osteoporotic vertebral fracture. As outcome measures they used physical functioning and pain scores. They concluded that the operatively treated group scored significantly higher on the outcome measures than the conservatively treated group. This was the case for the short-term as well as the long-term measurements[32].
Alvarez L. et al.[33] compared a conservative and operative treatment (percutaneous vertebroplasty). Similar to the results of Diamond TH. et al[32], they found that treatment with percutaneous vertebroplasty gives a rapid and significant relief of pain and improvement in quality of life.
Anderson, Froyshteter and Tontz[9] conducted a meta-analysis on vertebral augmentation (kyphoplasty). They compared vertebral augmentation with conservative treatment for osteoporotic spinal fractures. The meta-analysis showed greater pain relief, functional recovery and helath-related quality of life with cement augmentation compared with controls. Cement augmentation results were significant in the early (
Chang X et al (2015) compared vertebroplasty to kyphoplasty in a meta-analysis of prospective comparative studies. They concluded that percutaneous vertebroplasty takes less time in the operation, has a greater risk of cement leakage, was inferior in reducing cobb angle in the long term and results in lower anterior vertebral body height after surgery. For pain relief (main desire of patients) both procedures still remain effective[18].
Low bone mineral densitiy, presence of multiple treated vertebrae and a history of steroid usage were associated with new VCFs after vertebroplasty according to a meta-analysis from Cao J et al. (2016). Patients with these factors should be informed of the potential increased risk[17].
Song D and colleagues (2015) found no differences in the incidence of secondary fractures between vertebral augmentation techniques and conservative treatment for patients with osteoporotic vertebral compression fractures. They conducted a systematic review and meta-analysis of randomized controlled trials and prospective non-randomized controlled trials[31].
Physical Therapy Management
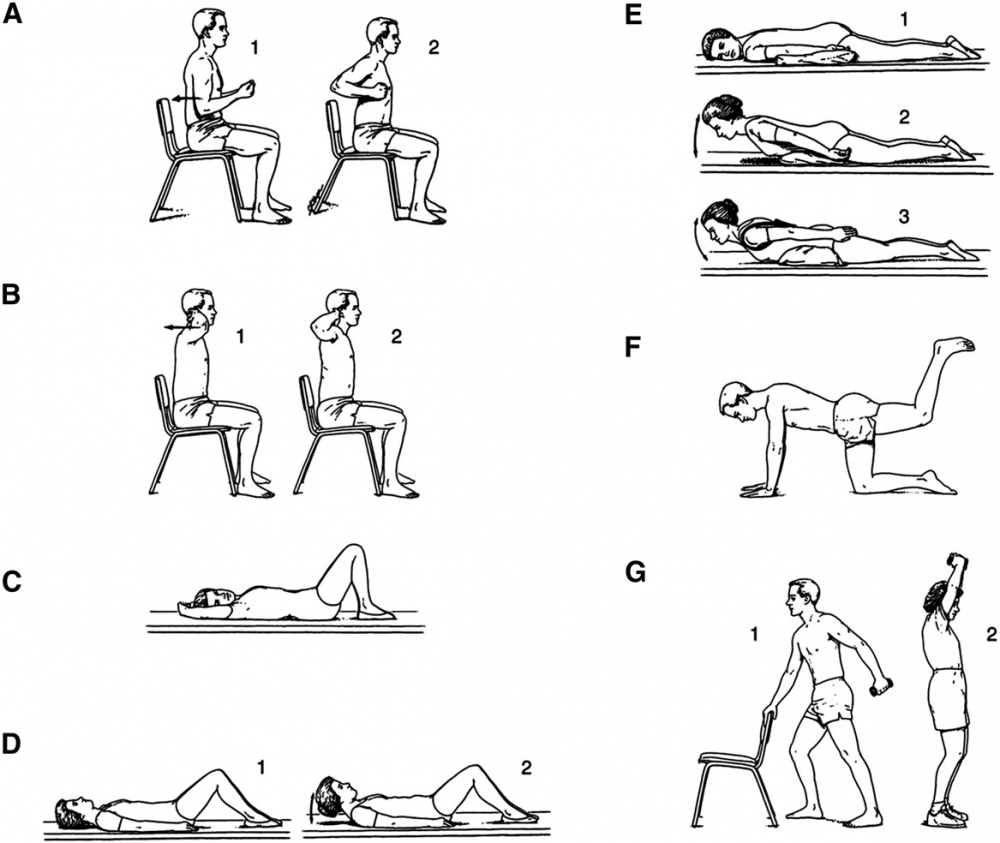
After a short period of bed rest patients should begin mobilisation with a rehabilitation and exercise program. The goals of rehabilitation are the prevention of falls, reduction of the kyphosis, enhancing axial muscle strength and providing correct spine alignment[37].
Regarding Physiotherapy management, there are a number of treatment approaches, including strengthening exercise, stabilisation exercise, balance training, stretching, relaxation techniques, manual therapy and taping[38][39]. Currently a large RCT is comparing exercise based and ‘hands on’ manual therapy based physiotherapy against a control[39].
Zehnacker and Bemis‐Dougherty conducted a systematic review to study the effect of weighted exercises on bone mineral density in post menopausal women[40]. Exercises such as walking has been shown to maintain or improve bone density in an osteoporotic population. Strengthening exercises, using weights or resistance bands, has also been shown to maintain or improve bone density at the location of the targeted muscle attachments. Maintaining bone health is extremely important, especially in the elderly as there typically is a decline in bone mass with age.
Strengthening and flexability exercises improve overall physical function and postural control. Improving postural control is important to reduce risk for falls. Falls often result in fractures in an osteoporotic population. Balance exercises are also important to further reduce the risk of falls[41].
Studies from De Kam et al. (2009, LoE:1A), Karinkanta et al. (2007, LoE:1B) and Hourigan SR et al. (2008, LoE:1B) all found that a combined balance and progressive strength training programme produced the best results in terms of maintaining leg strength, balance, bone mineral density and physical function compared to balance or strength training alone[42][43][44].
Sinaki et al demonstrated that a spinal extensor strengthening programme and a dynamic proprioceptive programme increased bone density and reduced the risk of VCFs. Moreover the incidence of new fractures associated with back extension exercises is lower than the incidence related to abdominal flexion exercises (16% versus 89%)[45].
Exercise and exercise technique that focuses on spinal extension play an important role in reducing the risk of osteoporosis-related fractures. In addition, reports have shown that strenuous spinal flexion exercise, whether therapeutic, recreational, or job related, may induce compression fracture if beyond the biomechanical competence of the vertebral bodies. In other words, extreme flexion is contra-indicated[46].
Back extensor exercises improve muscle strength, providing a better dynamic-static posture and reduction of the kyphotic deformity. Correction of the kyphosis also results in pain relief, increased mobility and an improvement in the quality of life[47].
It has been previously hypothesized that horizontal nonloading back extension exercises from a prone position can decrease the incidence of vertebral fractures[48]. Back extension exercises performed from the prone position load vertebral horizontal trabeculae without the risk of vertebral compression fracture that can occur with vertical loading[46].
Chen BL and colleagues studied the effectiveness of systematic back muscle exercises after vertebroplasty for spinal osteoporotic compression fractures. They found that systematic back muscle exercises resulted in a significant better outcome on the Oswestry Disability Index and pain level (VAS) compared to the control group. Control group only received general postoperation therapy without systematic back exercises[49].
Wendlova J. concluded that after a biomechanical analysis that carrying a backpack on the back is recommended to patients with osteoporotic vertebral fractures. This is based upon removing the muscular dysbalance of the trunk muscles and upon increasing the bone strength by compressive force acting upon the vertebrae. Compressive forces activate osteoblasts to enhance osteoformation.The backpack load is differentiated: patients with vertebral fractures put a weight up to 1 kg into their backpacks, patients without vertebral fractures but diagnosed with osteoporosis increase the load up to 2kg. Further research is needed[50].
To prevent falls and fractures, an exercise program should include balance and lower extremity strength training combined with a coordinated approach[46].
Postural taping can help in maintaining postural alignment. Tape is applied to the skin to provide increased proprioceptive feedback about postural alignment, improve thoracic extension, reduce pain and facilitate postural muscle activity and balance[51].
Key Research
The following articles are key evidence pieces for physical therapy interventions:
- Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials[36]
- A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: a randomized, controlled trial [8]
- Positive effects of exercise on falls and fracture risk in osteopenic women[9]
- Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study
- Identifying osteoporotic vertebral fracture[10]
- Position Statement of the Korean Society for Bone and Mineral Research[10]
Resources
www.nhs.uk/conditions/Osteoporosis/Pages/Introduction.aspx
www.nos.org.uk/about-osteoporosis
Clinical Bottom Line
Osteoporotic vertebral fractures are fractures of one ore more of the vertebrae due to osteoporosis. Osteoporosis causes the bones to be more fragile and more likely to fracture. Osteoporotic vertebral fractures classically occur during normal day-to-day activities such as bending, walking or lifting relatively light objects.
The pain of acute fracture usually lasts 4 to 6 weeks with intense pain at the site of fracture. Chronic pain may also occur in patients with multiple compression fractures, height loss and low bone density. Although this is probably due to structural changes or osteoarthritis.
Vertebral fractures doesn’t only occur due to osteoporosis. Also a trauma or metastasis can cause a vertebral fracture. The diagnosis of osteoporosis can be confirmed by Dual Energy X-ray Absorptiometry (DXA).
Often used outcome measures to evaluate the progression of a patiënt are: Visual analogue scale for overall pain and pain during day and night (VAS), a Quality of Life questionnaire and a Physical functioning questionaire ( modified 23-item version of the Roland–Morris Disability Questionnaire).
Conservative treatment (bed rest, analgesic medication, physiotherapy and bracing) still is the method of choice as medical treatment. Vertebral fractures can also be treated surgically using vertebroplasty and kyphoplasty.
As physical therapy management there are a number of treatment approaches, including strengthening exercise, stabilisation exercise, balance training, stretching, relaxation techniques, manual therapy and taping.
Recent Related Research
- Rzewuska M. The efficacy of conservative treatment of osteoporotic compression fractures on acute pain relief: a systematic review with meta-analysis.Eur Spine J. 2015 Apr;24(4):702-14. Level of Evidence: 1A.
- Buchbinder R, Golmohammadi K, Johnston RV, Owen RJ, Homik J, Jones A, Dhillon SS, Kallmes DF, Lambert RG.Percutaneous vertebroplasty for osteoporotic vertebral compression fracture.Cochrane Database Syst Rev. 2015 Apr 30;4:CD006349. Level of Evidence: 1A.
References
- ↑ Yoo JH, Moon SH, Ha YC, Lee DY, Gong HS, Park SY, Yang KH.Osteoporotic Fracture: 2015 Position Statement of the Korean Society for Bone and Mineral Research.J Bone Metab. 2015 Nov;22(4):175-81. 30. Level of Evidence: 2B.
- ↑ 2.02.1 NICE. Osteoporosis: assessing the risk of fragility fracture: NICE Guidelines CG146. Manchester: National Institute for Health and Care Excellence, 2012.
- ↑ NOS. What is Osteoporosis? National Osteoporosis Society. https://www.nos.org.uk/about-osteoporosis (accessed 03/02/15)
- ↑ Ström O, Borgström F, Kanis JA, Compston J, Cooper C, McCloskey EV, Jönsson B. Osteoporosis: burden, health care provision and opportunities in the EU: A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 2011 6:59–155 DOI 10.1007/s11657-011-0060-1
- ↑ NHS. Osteoporosis. National Health Service. http://www.nhs.uk/conditions/Osteoporosis/Pages/Introduction.aspx (accessed 03/02/15)
- ↑ 6.06.16.26.3 Buchbinder R, Golmohammadi K, Johnston RV, Owen RJ, Homik J, Jones A, Dhillon SS, Kallmes DF, Lambert RG.Percutaneous vertebroplasty for osteoporotic vertebral compression fracture.Cochrane Database Syst Rev. 2015 Apr 30;4:CD006349. Level of Evidence: 1A.
- ↑ Spine live. Spinal compression fractures reasons. Available from: https://www.youtube.com/watch?v=LILgFAEMAbg (last accessed 12.4.2019)
- ↑ 8.08.18.28.3 Gauthier A, Kanis JA, Jiang Y, Martin M, Compston JE, Borgström F, Cooper C, McCloskey EV. Epidemiological burden of postmenopausal osteoporosis in the UK from 2010 to 2021: estimations from a disease model. Arch Osteoporos 2011 6:179–188.
- ↑ 9.09.19.29.39.4 Kim DH, Vaccaro AR. Contemporary Concepts in Spine Care: Osteoporotic compression fractures of the spine; current options and considerations for treatment. The Spine Journal. 2006 6 479–487.
- ↑ 10.010.110.210.3 NICE. Alendronate, etidronate, risedronate, raloxifene and strontium ranelate for the primary prevention of osteoporotic fragility fractures in postmenopausal women (amended): NICE technology appraisal guidance 160. Manchester: National Institute for Health and Care Excellence, 2011.
- ↑ 11.011.111.2 Ralston SH, Fraser J.Diagnosis and management of osteoporosis.Practitioner. 2015 Dec;259(1788):15-9, 2. (Level of Evidence: 3A)
- ↑ 12.012.1 El-Fiki M. Vertebroplasty, Kyphoplasty, Lordoplasty, expandable devices and current treatment of painful osteoporoticvertebral fractures.World Neurosurg. 2016 Apr 9
- ↑ Steven R. Cummings et al. Epidemiology and outcomes of osteoporotic fractures. The Lancet. 2002
- ↑ Goodwin VA et al. Orthotics and taping in the management of vertebral fractures in people with osteoporosis: a systematic review. British Medical Journal.2016 (Level of Evidence 2A)
- ↑ Seppo Santavirta’, Yrjo T. Konttinen*, Markku Heliovaara3, Paul Knekt3, Peter Luthje4 and Arpo Aromaa. Determinants of osteoporotic thoracic vertebral fracture, Acta Oflhop Scand 1992; 63 (2): 198-202 (LoE 2B)
- ↑ Pain doctor Nevada. Spinal compression fracture. Available from: https://www.youtube.com/watch?v=dLiOQfr4e_A&t=20s (last accessed 12.4.2019)
- ↑ 17.017.117.2 NOF. Osteoporosis and your spine. National Osteoporosis Foundation. http://nof.org/articles/18 (accessed 03/02/15.
- ↑ 18.018.1 Puisto V, Rissanen H, Heliövaara M, Impivaara O, Jalanko T, Kröger H, Knekt P, Aromaa A, Helenius I. Vertebral fracture and cause-specific mortality: a prospective population study of 3,210 men and 3,730 women with 30 years of follow-up. Eur Spine J 2011 20:2181–2186 DOI 10.1007/s00586-011-1852-0.
- ↑ 19.019.119.219.319.4 Griffith JF. Identifying osteoporotic vertebral fracture. Quant Imaging Med Surg. 2015 Aug;5(4):592-602. (Level of Evidence: 2C)
- ↑ 20.020.1 Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V. Conservative management of patients with an osteoporotic vertebral fracture: a review of the literature. J Bone Joint Surg Br. 2012 Feb;94(2):152-7. (Level of Evidence: 2A)
- ↑ Silverman SL. The Clinical Consequences of Vertebral Compression Fracture. Bone 13, S27-S31. 1992. (Level of Evidence: 3B)
- ↑ Delmas PD, van de Langerijt L, Watts NB, Eastell R, Genant H, Grauer A, Cahal DL. Underdiagnosis of Vertebral Fractures Is a Worldwide Problem: The IMPACT Study. J Bone Miner Res. 2009. Accessed 31 January 2019.
- ↑ Gehlbach SH, Bigelow C, Heimisdottir M, May S, Walker M, Kirkwood JR.Recognition of vertebral fracture in a clinical setting.Osteoporos Int. 2000;11(7):577-82. (Level of Evidence: 4)
- ↑ Medscape. Osteoporosis Differential Diagnoses. http://emedicine.medscape.com/article/330598-differential (accessed 10 May 2016) (Level of Evidence: 5)
- ↑ Yoo JH, Moon SH, Ha YC, Lee DY, Gong HS, Park SY, Yang KH.Osteoporotic Fracture: 2015 Position Statement of the Korean Society for Bone and Mineral Research.J Bone Metab. 2015 Nov;22(4):175-81. 30. (Level of Evidence: 2B)
- ↑ Deleskog L, Laursen NØ, Nielsen BR, Schwarz P.Vertebral fracture assessment by DXA is inferior to X-ray in clinical severe osteoporosis.Osteoporos Int. 2016 Feb 18. (Level of Evidence: 3B
- ↑ Torres C, Hammond I.Computed Tomography and Magnetic Resonance Imaging in the Differentiation of Osteoporotic Fractures From Neoplastic Metastatic Fractures.J Clin Densitom. 2016 Jan-Mar;19(1):63-9. (Level of Evidence: 4)
- ↑ Diamond TH. et al. Management of Acute Osteoporotic Vertebral Fractures: A Nonrandomized Trial Comparing Percutaneous Vertebroplasty with Conservative Therapy. Am J Med. 2003;114:257–265. (Level of Evidence: 2B)
- ↑ Lavelle EA, Cheney R, Lavelle WF.Mortality Prediction in a Vertebral Compression Fracture Population: the ASA Physical Status Score versus the Charlson Comorbidity Index.Int J Spine Surg. 2015 Nov 12;9:63. (Level of Evidence: 3B)
- ↑ 30.030.130.2 James Langdon et al. Vertebral compression fractures – new clinical signs to aid diagnosis. Ann R Coll Surg Engl 2010; 92: 163–166 (Level of evidence: 2C)
- ↑ 31.031.131.2 Crandall CJ, Newberry SJ, Diamant A, Lim YW, Gellad WF, Booth MJ, Motala A, Shekelle PG.Comparative effectiveness of pharmacologic treatments to prevent fractures: an updated systematic review. Ann Intern Med. 2014 Nov 18;161(10):711-23. Level of Evidence: 1A.
- ↑ 32.032.132.232.3 Gerdhem P. Osteoporosis and fragility fractures: Vertebral fractures. Best Practice Research Clinical Rheumatology 2013 27: 743–755.
- ↑ 33.033.133.233.333.4 NICE. Percutaneous vertebroplasty and percutaneous balloon kyphoplasty for treating osteoporotic vertebral compression fractures: NICE technology appraisal guidance TA279. Manchester: National Institute for Health and Care Excellence, 2013.
- ↑ Lee Health. Fixing a fractured spine. Available from: https://www.youtube.com/watch?v=QjvKkYehpUI (last accessed 12.4.2019)
- ↑ Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment.Spine J. 2006 Sep-Oct;6(5):479-87. Level of Evidence: 3A.
- ↑ 36.036.1 Liu JT et al. Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture: a prospective, comparative, and randomized clinical study. Osteoporos Int. 2010 Feb;21(2):359-64. Level of Evidence: 1B.
- ↑ Yoo JH, Moon SH, Ha YC, Lee DY, Gong HS, Park SY, Yang KH.Osteoporotic Fracture: 2015 Position Statement of the Korean Society for Bone and Mineral Research.J Bone Metab. 2015 Nov;22(4):175-81. 30. (Level of Evidence: 2B)
- ↑ Pratelli E, Cinotti I, Pasquetti P. Rehabilitation in osteoporotic vertebral fractures. Clin Cases Miner Bone Metab. 2010 7(1): 45–47.
- ↑ 39.039.1 Barker K, Javaid MK, Newman M, Minns Lowe C, Stallard N, Campbell H, Gandhi V, Lamb S. Physiotherapy Rehabilitation for Osteoporotic Vertebral Fracture (PROVE): study protocol for a randomised controlled trial. Trials 2014 15:22
- ↑ Zehnacker CH, Bemis‐Dougherty A. Effect of Weighted Exercises on Bone Mineral Density in Post Menopausal Women A Systematic Review. Journal of Geriatric Physical Therapy. 2007; 30(2):79-88. (Level of Evidence: 1A)
- ↑ Burke TN, Franca FJR, Ferreira de Meneses SR, Pereira RMR, Marques AP. Postural control in elderly women with osteoporosis: comparison of balance, strengthening and stretching exercises. A randomized controlled trial. Clinical Rehabilitation; 26 (11): 1021-1031. 2012. (Level of Evidence: 1B)
- ↑ De Kam D, Smulders E, Weerdesteyn V, Smits-Engelsman BCM. Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials. Osteoporos Int. 2009;20:2111–2125 (Level of evidence: 1A)
- ↑ Karinkanta S, Heinonen A, Sievänen H, Uusi-Rasi K, Pasanen M, Ojala K. A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: a randomized, controlled trial. Osteoporos Int. 2007;18:453–462. (Level of evidence: 1B)
- ↑ Hourigan SR, Nitz JC, Brauer SG, O’Neill S, Wong J, Richardson CA. Positive effects of exercise on falls and fracture risk in osteopenic women. Osteoporos Int. 2008;19:1077–1086. (Level of evidence: 1B)
- ↑ Sinaki M, Lynn SG. Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study.Am J Phys Med Rehabil. 2002 Apr;81(4):241-6. (Level of Evidence: 3B)
- ↑ 46.046.146.2 Sinaki M. Exercise for patients with osteoporosis: management of vertebral compression fractures and trunk strengthening for fall prevention.PM R. 2012 Nov;4(11):882-8. (Level of Evidence: 3A)
- ↑ Itoi E, Sinaki M.Effect of back-strengthening exercise on posture in healthy women 49 to 65 years of age.Mayo Clin Proc. 1994 Nov;69(11):1054-9. (Level of Evidence: 3B)
- ↑ Sinaki M.The role of physical activity in bone health: a new hypothesis to reduce risk of vertebral fracture.Phys Med Rehabil Clin N Am. 2007 Aug;18(3):593-608, xi-xii. (Level of Evidence: 5)
- ↑ Chen BL, Zhong Y, Huang YL, Zeng LW, Li YQ, Yang XX, Jiang Q, Wang CH. Systematic back muscle exercise after percutaneous vertebroplasty for spinal osteoporotic compression fracture patients: a randomized controlled trial.Clin Rehabil. 2012 Jun;26(6):483-92. (Level of Evidence: 1B)
- ↑ Wendlova J. The importance of carrying a backpack in the rehabilitation of osteoporotic patients (biomechanical analysis).Bratisl Lek Listy. 2011;112(1):41-3. (Level of Evidence: 4)
- ↑ Bautmans I, Van Arken J, Van Mackelenberg M, Mets T. Rehabilitation using manual mobilization for thoraic kyphosis in elderly postmenopauzal patients with osteoporosis. J Rehabil Med 2010, 42: 129-135. (Level of Evidence: 3B)