Referred Pain
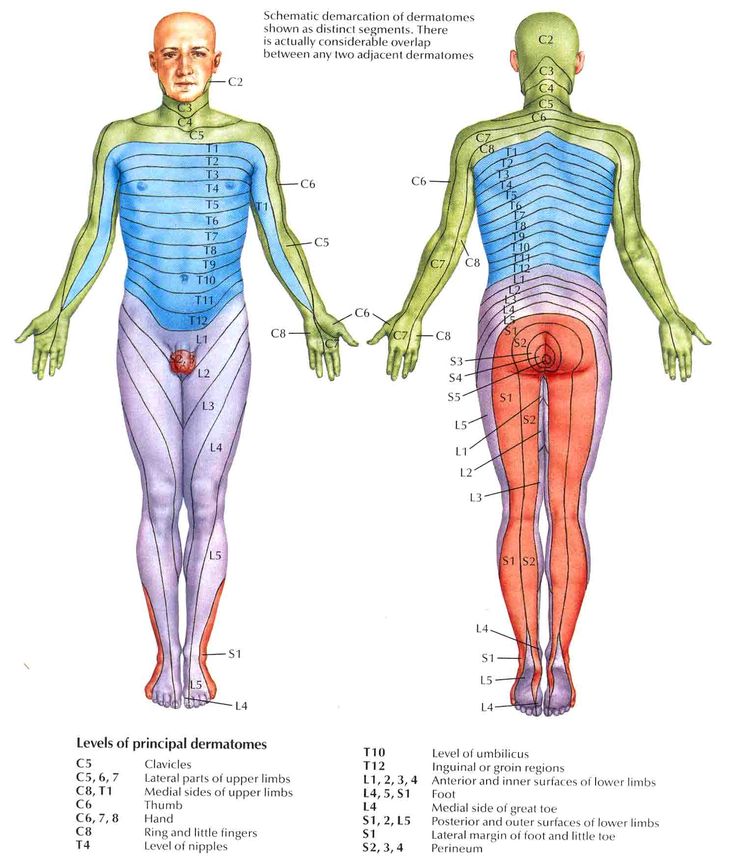
Referred pain is pain perceived at a location other than the site of the painful stimulus. It usually originates in one of the visceral organs but is felt in the skin or sometimes in another area deep inside the body. Its mechanism is likely due to the fact that pain signals from the viscera travel along the same neural pathways used by pain signals from the skin. The result is the perception of pain originating in the skin rather than in a deep-seated visceral organ or neural structure.
Visceral nociceptors project into the spinal cord via small diameter myelinated and unmyelinated fibres from the autonomic nervous system. They go on to synapse close to the point of embryonic origin in the spine. When an organ develops pain, it can therefore be perceived as being at a different point in the body, on the surface, rather than in the organ itself.[1]
Mechanism
Hyperalgesia
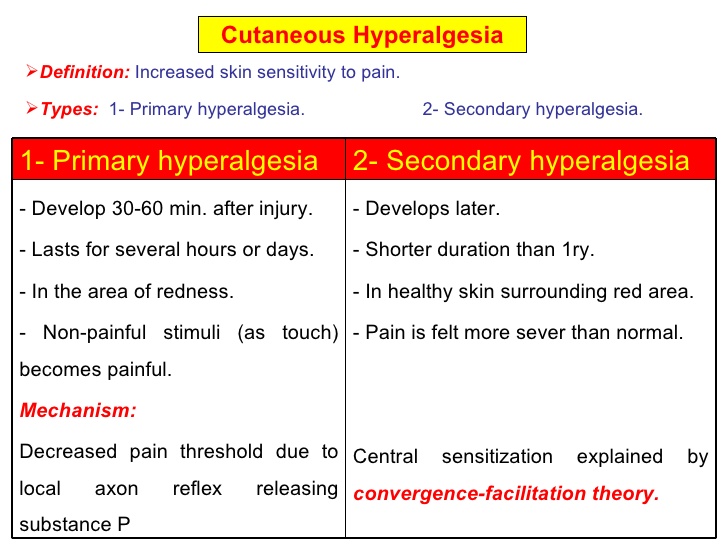
Hyperalgesia is defined as “An increased sensitivity to pain, which may be caused by damage to nociceptors or peripheral nerves”.[2]
It is divided into 2 types, primary and secondary.
- Primary hyperalgesia – pain and sensitivity in the damaged tissues.
- Secondary hyperalgesia – pain and sensitivity that occurs in area around the damaged tissues.
Substance P appears to have a significant role in the sensitiation of nociceptors, which may explain the heightened feeling of pain in injured tissue (primary hyperalgesia). Although this doesn’t account for the perception of non-painful stimuli as painful. Secondary hyperalgesia is most likely accounted for by changes in the dorsal horn which affect the processing of sensory information. [1] It is likely that normally silent nociceptors are recruited, and sprouting of large diameter sensory afferent occurs projecting into the dorsal horn laminae.
Allodynia
Central pain sensitization (increased response of neurons) following painful, often repetitive, stimulation. Allodynia can lead to the triggering of a pain response from stimuli which do not normally provoke pain.[3]
Types of allodynia:
- Mechanical allodynia (also known as tactile allodynia)
- Static mechanical allodynia – pain in response to light touch/pressure[4]
- Dynamic mechanical allodynia – pain in response to stroking lightly[5]
- Thermal (hot or cold) allodynia – pain from normally mild skin temperatures in the affected area
- Movement allodynia – pain triggered by normal movement of joints or muscles.
Inflammatory Pain
One of the cardinal features of inflammatory states is that normally innocuous stimuli produce pain[6]
References
- ↑ 1.01.1 Roger, Barker, Barasi, Neal. Neuroscience at a glance.1999 Blackwell science.
- ↑ Hart BL (1988). “Biological basis of the behavior of sick animals”. Neurosci Biobehav Rev 12 (2): 123–37.
- ↑ Merskey & Bogduk (Eds.) Classification of Chronic Pain. Seattle: IASP Task Force on Taxonomy, 1994
- ↑ Attal N, Brasseur L, Chauvin M, Bouhassira D (1999). “Effects of single and repeated applications of a eutectic mixture of local anaesthetics (EMLA) cream on spontaneous and evoked pain in post-herpetic neuralgia”. Pain 81 (1–2): 203–9
- ↑ LoPinto C, Young WB, Ashkenazi A (2006). “Comparison of dynamic (brush) and static (pressure) mechanical allodynia in migraine”. Cephalalgia 26 (7): 852–6.
- ↑ B. L. Kidd1 and L. A. Urban2. Mechanisms of inflammatory pain. Oxford JournalsMedicine & Health BJA Volume 87, Issue 1Pp. 3-11