Definition/description
A pelvic fracture is a disruption of the bony structures of the
Clinically Relevant Anatomy
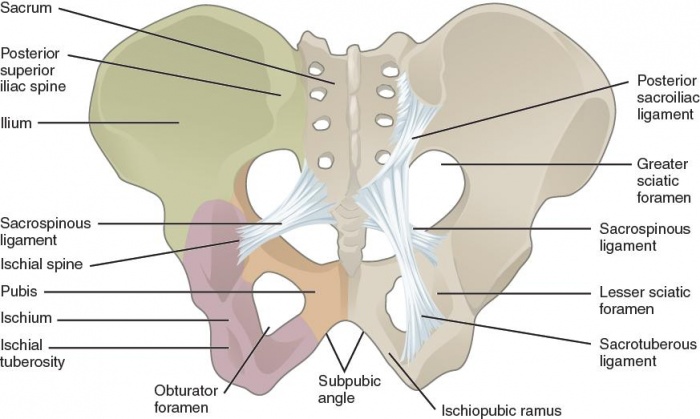
The bony pelvis is the entire structure formed by the two hip bones, the sacrum, and the coccyx, which is attached inferiorly to the sacrum. The paired hip bones are the large, curved bones that form the lateral and anterior aspects of the pelvis. Each adult hip bone is formed by three separate bones that fuse together during the late teenage years. These bony components are the ilium, ischium and pubis. [2]
The stability of the pelvis relies on the integrity of the posterior weight-bearing sacroiliac complex and the transfer of weight bearing forces from the spine to the lower extremities. The hip joints and lower limbs and vice versa. This joint also acts as a shock absorber. Several muscles influence the movement and the stability of the SI joint either through attachment to the sacrum or the ilium, or ligamentous attachment to the strong anterior and posterior SI-joint ligaments.Two thirds of the joint includes the posterior superior ligamentous section and one third of the joint includes the anterior inferior synovial component. [3] [4]
The pelvis contains sliding, tilting and rotation movement components.
Major nerves, blood vessels, and portions of the bowel, bladder, and reproductive organs all pass through the pelvic ring. The pelvis protects these important structures from injury. It also serves as an anchor for the muscles of the hip, thigh and abdomen.
Epidemiology/Etiology
Pelvic fractures occur after both low-energy and high-energy events. The appearance of pelvic fractures is the greatest in people aged between 15 and 28. In persons, younger than 35, pelvic fractures occur more in males than in females. In persons, older than 35, pelvic fractures are more likely to happen to females than males[5]. In younger people, pelvic fractures occur mostly as a result of high-energy mechanisms. In older people, they occur from minimal trauma, such as a low fall. Elderly people with [6] (level of evidence: 2B)
The video clip below gives in detail a summary of pelvic fractures aetiology and treatments/complications.
Characteristics/Clinical Presentation
A pelvic fracture should always be considered when history of a significant trauma is present. Pelvic fractures may be recognised by: tenderness, pain, bruising, swelling and crepitus of the pubis, iliac bones, hips and sacrum. Other presenting factors are: haematuria, rectal bleeding, haematoma and neurological and vascular abnormalities in the legs. Physical findings could include abnormal position of the lower limbs and pelvic deformity or pelvic instability. With avulsion injuries, there is often pain associated with contraction of the involved muscles.[8]
There must be a differentiation between high impact unstable fractures and low impact stable pelvic fractures. This can be done by determination of the circumstances of the trauma. Patients with unstable fractures are usually unable to stand, in contrast to patients with stable fractures who can often walk unaided.
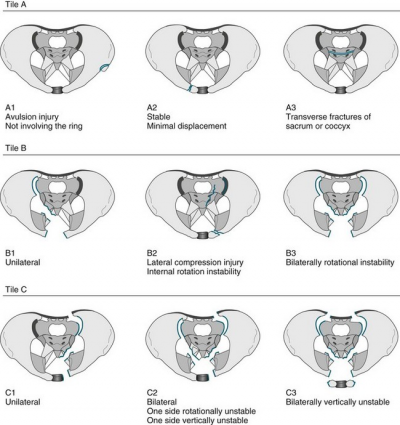
Pelvic fractures can be classified by several classification systems. The two most commonly used systems are Tiles classification and the Young-Burgess Classification.
Classification of pelvic fractures by Tile is based on the integrity of the posterior sacroiliac complex. [2] [3]
- Type A: rotationally and vertically stable, the sacroiliac complex is intact. Type A fractures are mostly managed non-operatively.
o A1: avulsion fractures
o A2: stable iliac wing fractures or minimally displaced pelvic ring fractures
o A3: transverse sacral or coccyx fractures - Type B: rotationally unstable and vertically stable, caused by external or internal rotational forces, results in partial disruption of the posterior sacroiliac complex.
o B1: open-book injuries
o B2: lateral compression injuries
o B3: bilateral rotational instability - Type C: rotationally unstable and vertically unstable, complete disruption of the posterior sacroiliac complex. These unstable fractures are mostly caused by high-energy trauma like falls from height, motor vehicle accidents or crushing injuries.
o C1: unilateral injury
o C2: bilateral injuries in which one side is rotationally unstable and the controlateral side is vertically unstable
o C3: bilateral injury in which both sides are vertically unstable
Seventy to eighty percent of all pelvic injuries are type A or type B fractures.[4]
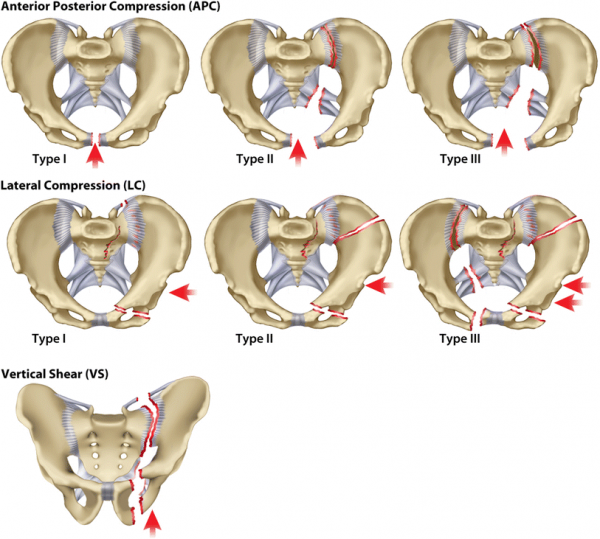
Classification of pelvic fractures by Young and Burgess is based on the mechanism of injury. [9][10][11]
Anterior posterior compression
- Lateral compression
- Vertical shear
- Complex: a combination of any three primary patterns
The Young and Burgess classification system is limited as it provides little guidance for treatment. [12]
Differential Diagnosis
Pelvic fractures rarely occur as a single injury. They should be differentiated from, or could be accompanied by many disorders like: [13][14][15][16] (levels of evidence: 4)
– – – genito-urinary injuries
– bowel injury
– muscular injuries
– neurovascular injuries
– bladder injury
– urethral injury
Diagnostic Procedures
The diagnosis of a pelvic fracture mostly will be made by medical imaging. Imaging tests can determine the location of a fracture, how many bones are affected and whether an injury has damaged surrounding soft tissues, such as tendons, ligaments, blood vessels or nerves: [17]
- X-rays: antero-posterior view, inlet view and outlet view
- CT scan
- Ultrasound
- Bone scans
The severity and correlated injuries can be investigated by: [18] (level of evidence: 2B)
- Urinalysis
- Measurement of haemoglobin and hematocrit: to measure blood loss
- Retrograde urethrography
- Arteriography
- Cystography
Outcome measures
To measure the outcome of patients with pelvic fractures many questionnaires can be used. They can be divided in disease specific or patient specific outcome measures. [19]
Disease specific:
– – Examination
Because a high-energy trauma could damage the primary organ systems, the examination of a pelvic fracture should start with investigation of life-threatening injuries. The abdomen, perineum, genitals, rectum and lower back must be examined very carefully. [8] High-energy fractures are often associated with severe injuries of other organs. [10] When life-threatening injuries are excluded the examination should include an inspection and palpation of the pelvis to identify crepitus and to determine pelvic stability. It is necessary to examine whether related injuries are present. Some injuries that could be associated with pelvic injuries are: soft-tissue injuries, urethral injuries, skeletal injuries, neurovascular injuries and neurologic injuries.
Soft-tissue injuries like haematomas, abrasions and lacerations commonly accompany pelvic ring injuries. Haematomas located at the scrotum, labium, flank and the inguinal region are indicative of intrapelvic haemorrhage [20]. Lacerations of the perineum, rectum and vagina are indicative of severe injuries and could be indicative for contamination by urine or stool. Ohmori et al. concluded that the risk factors for massive haemorrhage are: Lactate level, AO/OTA classification, and pelvic extravasation of contrast fluid on CT. They created a new effective predictive score of massive haemorrhage in pelvic ring fractures. [14] Pelvic fracture urethral injury is an uncommon but potentially devastating result of pelvic fracture. Symptoms of urethral injuries are blood at the external urethral meatus, a high-riding (non-palpable) prostate gland in man, and perineal and genital swelling. Pelvic fractures often are present with bladder disruptions. The disruption may be intraperitoneal, extraperitoneal, or both. In patients with a bladder disruption gross haematuria will be present.[15]
Frequently pelvic fractures are associated with skeletal injuries. It is necessary that the clinician examines the spine and extremities. There could be limb length discrepancies, or internal/external rotational deformities.
Because many structures transverse the pelvis, it is possible that a pelvic injury causes injury to a neurovascular structure. Vascular injuries occur more often than arterial injuries. Both may contribute to haemorrhage. A vascular injury is very urgent to treat. [16]
Sometimes there will also be neurological injuries. The nerve roots that are typically injured are L5 and S1. Sometimes L4 (severe pelvic injury) or S2-S5 nerves (sacral injuries) can be damaged too. The clinician should carefully detect these nerve injuries by a neurological examination.
Pelvic fractures should be considered in the context of a polytrauma management, rather than in isolation. The treatment and management of each patient requires careful, individualised decision making (3) (level of evidence: 4). Medical management of pelvic fractures consists of many parts. First of all, if necessary, resuscitation must be done. Afterwards, the patient and the fracture should be stabilised. After the medical management is finished the rehabilitation can start.
The stabilisation of pelvic fractures has historically been treated non-operatively. Lately operative management has increased in the treatment of unstable pelvic fractures. Operative management of an unstable pelvic ring injury allows earlier mobilisation, and thereby diminishes the complications of immobilisation. Stabilisation may also be important for the survival of the patient and may be desirable to improve the long-term functional results. It allows correction and prevention of significant pelvic deformities, so the clinical outcomes of the patient will improve [21].
In emergency, the fracture will be stabilised by an external fixator (for antero-posterior injuries) or a ‘C-clamp’ (for vertical shear injuries). The definitive fixation can be done anteriorly or posteriorly and internal or external. Mostly plates or screws are used to stabilise a fracture. Rommens et al. (2015) concluded that more studies are needed to find the optimal treatment for each type of instability. [22] Other methods used to treat pelvic fractures are traction, spica casts, pelvic slings, and turnbuckles. Physical therapy is an important part of the rehabilitation in both, low-energy and high-energy pelvic fractures. Low-energy injuries are usually managed with conservative care. This includes bed rest, pain control and physical therapy. [8] High-energy injuries, especially the unstable fractures must be reduced by surgical treatment. Afterwards physical therapy includes the same treatment as in low-energy fractures. Early mobilisation is very important because prolonged immobilisation can lead to many complications, including respiratory and circulatory dysfunctions. Physical therapy helps the patient to get out of bed as soon as possible.
The goals of the physical therapy program should provide the patient with an optimal return of function by improving functional skills, self-care skills and safety awareness. [23] The main goals are to improve the pain level, strength, flexibility, speed of healing, and the motion of the hip, spine and leg. Another important goal is to shorten the time needed to return to activity and sport.
The intensity of the rehabilitation depends on whether the fracture was stable or unstable.
In people with surgical treatment, physical therapy starts after 1 or 2 days of bed rest. It is initiated with training of small movements, transfers and exercise training. The following exercises can start immediately after surgery and should be done at least four times a day (unless told otherwise). The number of repetitions are guidelines and can vary with every patient. [24]
Plantar flexion and dorsiflexion of the feet Abduction of the hip Contraction of the quadriceps Extension of the knee: lying Extension of the knee: sitting Short-term goals for patients after surgery are: independence with transfers and wheelchair mobility. Depending on the medical status of the patient these goals can be achieved in 2 to 6 weeks. The physical therapy program can be continued in the hospital or at home. The home-based program includes basic range of motion, stabilising and strengthening exercises intended to prevent contracture and reduce atrophy.
During the non-weight bearing status the patient performs isometric exercises of the gluteal muscle and quadriceps femoris muscle, range of motion exercises and upper-extremity resistive exercises (for example shoulder and elbow flexion and extension) until fatigued. The number of repetitions can vary with the patient. [25]
Once weight-bearing is resumed, physical therapy consists of gait training and resistive exercises for the trunk and extremities, along with cardiovascular exercises (for example treadmill or bicycle training). Stabilisation exercises and mobility training should also be remained in the program. [26] Aquatherapy is also good and helpful when available. [25]
Mobility training is useful to regain the range of motion in the hip, knee and ankle after immobilisation. Gait training should start with walking between parallel bars. Afterwards the patient should learn how to walk with a walker or with a cane. Balance and proprioception training should also be included in the rehabilitation. Resistive training should be progressive to improve the muscle strength in the hip and leg. In the final stage functional exercises should be included to provide the patient with an optimal return of function.
The videoclip below shows a good progression of physiotherapy, the progressions not applicable for the old or frail. In pelvic fractures in the elderly population, the rehabilitation process will be focused on optimising their quality of life. Rapid mobilisation and sufficient pain relief are the main objectives of treatment[28] and appointment of the home to assess the need for eg rails, ramps, increased lighting, removal of loose mats. Appropriate walking aids should also be supplied. A falls prevention outpatient program could be of benefit.
Zidén et al. (2010), investigated the long-term effect of a home rehabilitation program. They concluded that one year after the start of the rehabilitation process, most patients didn’t consider themselves fully recovered, compared to their situation before the fracture. [29] There should be more investigations to describe the short-term and long-term effects of the rehabilitation for pelvic fractures. Little research is focused on an optimal conservative management of pelvic fractures. Most studies focus on the medical management. There is more evidence needed to define an optimal physical therapy protocol.
First, the type of pelvic fracture should be determined. The medical management and further rehabilitation depends whether the fracture is stable or unstable. If the fracture is unstable, mostly surgery will be necessary. Pelvic fractures should be considered in the context of polytrauma management, rather than in isolation due to the complexity of the injuries leading to pelvic fractures.
In people with surgical treatment, physical therapy starts after 1 or 2 days of bed rest. Physical therapy starts with non-weight bearing exercises. Only when the fracture is stable enough weight bearing exercises can be initiated. Walking aids will be necessary and must be reduced gradually.
We can conclude that the treatment and management of each patient requires careful, individualised decision making and thereby see this as the main idea regarding pelvic fractures. Li et al., 2014, investigated the clinical efficacy of two types of operative treatment in unstable pelvic fractures. They compared percutaneous sacroiliac screw internal fixation with sacroiliac joint anterior plate fixation. Perioperative period clinical indicators, the postoperative Matta score and the postoperative Majeed function score were measured in both groups. The results of the study revealed less injury, less bleeding, less pain and more rapid recovery in patients treated with percutaneous sacroiliac screws compared to the plate fixation. The complication rate was significantly lower and the rate of Matta score and Majeed function score were significantly higher in the group with percutaneous sacroiliac screw fixation. [30] (level of evidence: 1B)
Sherrington et al., 2016, is a randomised controlled trial that aims to evaluate the effects of an exercise and fall prevention self-management intervention on mobility-related disability and falls in older people following fall-related lower limb or pelvic fracture. Unlike previous post-fracture studies, the intervention and follow-up will be long-term, and the majority of exercise will be undertaken independently, aiming for a balance between sufficient intensity for effectiveness and reduced cost for feasibility of implementation. As the proportion of older rises globally, the costs associated with lower limb and pelvic fractures will increase. There is systematic review evidence that outcomes after fall-related fractures can be improved with well-designed intervention programs but the best approach to improve function is not evident. Existing trials of post-fracture rehabilitation leave many questions unanswered. Almost all of the studies included in these earlier systematic reviews give evidence for hip fracture rehabilitation and not specific for pelvic fractures.[31] (level of evidence: 1B)Medical Management
Physical Therapy Management
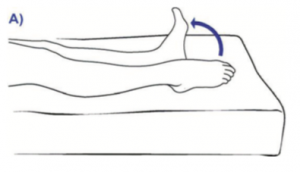
Sit up or lie down. Keep your legs straight and move your feet up and down at the ankles, pointing your toes and then relaxing.
Repeat 10 – 15 times every hour.
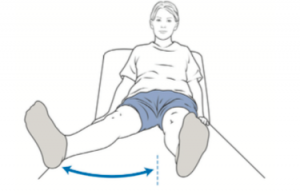
Move your leg out to the side and then back to the middle.
Repeat both sides 10 times.
Keep your legs flat on the bed. Push the knee down so that your leg is straight and then tighten your thigh muscle and hold for five seconds.
Repeat 5 – 10 times.
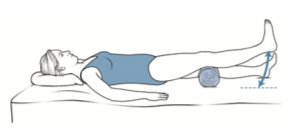
Lie on your back. Put a rolled towel under your knee.
Tighten your thigh muscles and straighten your knee, lifting your heel off the bed. Hold your leg straight for five seconds and lower it gently.
Repeat both sides 10 times.
Once you can sit in a chair or wheelchair comfortably: Pull your foot up towards you, tighten your thigh muscle and straighten your knee. Hold this position for five seconds.
Repeat 10 – 15 times every hour. Key Research
Clinical Bottom Line
Recent Related Research (from Pubmed)
References