Introduction
Stroke remains public health issue with attendance sequelae. Stroke is the one of major leading cause of disability[1] and this impact stroke survivor’s quality of life[2] including their sexual quality of life.
Definition
Physical Disability can be defined as impairment in body structures and functions, activities limitation and participation restrictions. International Classification of Functioning, Disability and Health (ICF).
Sexual Dysfunction can be defined as low sexual functioning as a result of “decline in libido and coital frequency for both genders, decline in vaginal lubrication and orgasm in females and in erection and ejaculation in males”[3].
Physical Disability
Disability is commonly reported among stroke survivors[2][4][5]. A third of stroke survivors have moderate to severe disability and another third have mild disability[5]. About 95% of the stroke survivors had moderate/severe global disability[4]. This disability may lead to hamper community reintegration and participation restriction of community-dwelling stroke survivors[6]. Focusing on reducing disability during rehabilitation will not only improve quality of life and reduce burden of stroke but will as well enhance self-reliance and productivity[1].
Assessment of Physical Disability
There are many assessment tools in form of outcome measure to assess physical disability among stroke survivors. Some are regional, general and condition specific. see Stroke Outcome Measures Overview.
Sexual Dysfunction
Sexuality is an important issue in post-stroke rehabilitation. Most stroke survivors reported low sexual functioning[7][8]. This dysfunction may be ‘‘a difficulty that occurs during the sexual response cycle that prevents the individual from experiencing satisfaction from sexual activity’’[9] or dysfunction characterized by pain following sexual intercourse[10].
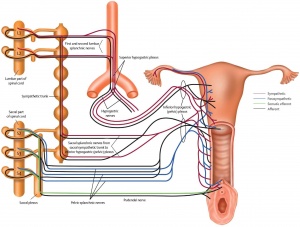
Sexual dysfunctions among stroke survivors are multi-factorial in nature. The cause can be primary, secondary and tertiary in nature. The primary causes include: stroke directly affect sexual functioning e.g. “decline in libido and coital frequency for both genders, decline in vaginal lubrication and orgasm in females and in erection and ejaculation in males”[3]; and medical related sexual problems such as medication and premorbid medical conditions. Secondary causes include: sensorimotor problems which unable the stroke survivors to position themselves during sexual activity. Cognitive, behavioural and psychosocial adjustment issues formed the tertiary causes[3].
Assessment of Sexual Dysfunction
There are numerous outcome measure tools to assess sexual dysfunction in stroke survivors. The list are not limited to these: International Index of Erectile Function (IIEF), Derogatis Interview for Sexual Functioning (DISF), Changes in Sexual Functioning Short-Form (CSFQ-14), Sexual Function Questionnaire (SFQ), Arizona Sexual Experience Scale (ASEX), Sexual Satisfaction Scale for Women (SSS-W), Sexual Self-Perception and Adjustment Questionnaire (SSPAQ), etc[3][11].
Management
Management of physical disability
One of the goals of rehabilitation post stroke is to reduce disability to achieve maximum function and participation. There are several means of achieving this through physical therapy intervention. The role of physical activities cannot be over emphasized in improving function and reducing disability. see Stroke: The Role of Physical Activity and Physical Activity in Individuals with Disabilities.
Management of sexual dysfunction[3]
- pharmacological interventions
- non-pharmacological interventions such as: mechanical devices (e.g. vacuum pumps, penile implants, penile prostheses and lubricating gels); psycho-educational interventions (e.g. counseling and psychotherapy); physical therapy (e.g physiotherapy for bed mobility)
- complementary medicine interventions
Physical Therapy management of sexual dysfunction
Couples may need to be thought bed mobility when one or both partners have hemiparesis after stroke[12]. Reference