Original Editors
Lead Editors
Definition/Description
A continuum of shoulder instability exists with laxity at one end and complete dislocation of the joint at the other. Defining posterior shoulder instability (PSI) is therefore difficult, not only defining it within this continuum but differentiating it from other shoulder pathologies. PSI is described as posterior glenohumeral translation that reproduces symptoms outside the normal physiologic translation in an individual and only accounts for about 5% of all patients with shoulder instabilities.[1] [2] [3] Translation that is not symptomatic is considered laxity.
Epidemiology/Etiology
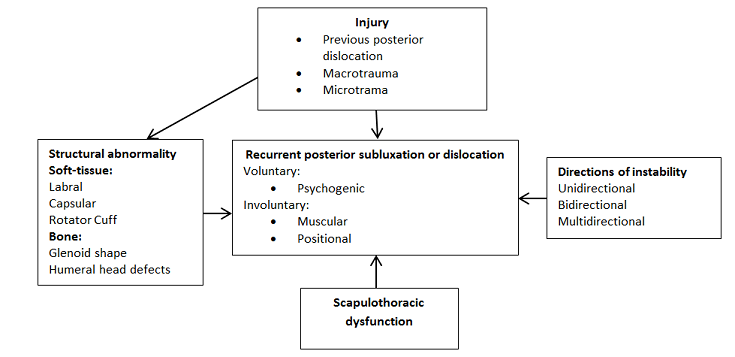
The etiology of posterior shoulder instability is very complex and multifactorial. The paucity of research leaves it challenging to accurately diagnose, classify, and treat PSI.[1][4]The typical patient population consists of active men 20-30 years of age engaging in high contact sports. Approximately 50% of patients report a distinct injury that brought on the instability or symptoms they have, yet only 17% report having a dislocation requiring reduction. [1] [3] Posterior shoulder instability is generally uncommon and rarely occurs alone. Contributing existing/coexisting factors include microtrauma or macrotrauma injuries to the shoulder, previous dislocations, soft-tissue and/or boney structural abnormalities, and scapulothoracic dysfunction. PSI can occur through volitional means or from positional or muscular instabilities.
Trauma
Microtrauma is an important factor in the development of instability due to the repetitive shearing forces and loads to the posterior shoulder in the flexed, adducted, and interally rotated position. Microtrauma can lead to degeneration of anatomical structures that function to stabilize the joint. This type of trauma occurs in weight lifters doing bench-presses, overhead sport athletes, swimmers, and military personel. [1] [4]Macrotrauma is a mechanism from a substantial injury such as a blow to the anterior shoulder or axial load while the shoulder is flexed. This type of trauma is common for patients involved in high contact sports such as football.
Pathoanatomy
Structural abnormalities are shown to attribute to posterior instability of the shoulder. Important structures that stabilize the shoulder and can be the cause of dysfunction include the posterior band of the inferior gleno-humeral ligament, glenoid, coracohumeral ligament, posterior capsule, the rotator cuff muscles and the biceps tendon.
Soft-Tissue etiologies that can contribute to structural abnormalities include, but are not limited to: [1] [3] [4] [5]
- Reverse-bankart lesion involving tearing of the posterioinferior region of the capsulolabral complex
- Kim lesion or avulsion to the posteroinferior labrum
- Osseous avulsion of the posterior aspect of the glenoid rim from a reverse osseous Bankart lesion
- Reverse Hills-sachs lesion
- Capsular laxity from recurrent subluxation
- Chondrolabral erosion of the glenoid rim
- Tear of rotator cuff and/or tendons
- Avulsion of the glenohumeral ligaments
Boney abnormalities that are associated with posterior instability of the shoulder are:[1]
- Glenoid retroversion
- Anterior humeral head defects
- Glenoid erosion.
Scapulothoracic Dysfunction
The importance of scapulothoracic dysfunction in PSI is poorly understood. Winging of the scapula often occurs as the shoulder subluxates during a provocative position and dynamic anatomical movement. It is unclear whether it is due to a compensatory motion or a contributor to instability. Also, weakness of the serratus muscle may attribute to instability. [1]
Volitional
Volitional subluxation from an unstable shoulder can be psychogenic; where the patient voluntarily subluxes their shoulder for some secondary gain, such as attention. These patients can develop symptomatic instabilites but are not surgical candidates. Other volitional subluxers include a group that is usually physically active and have involvement of involuntary subluxation and instability that interferes with their sports. [1] [3] These patients are surgical candidates.
Characteristics/Clinical Presentation
Patients will commonly present with complaints of pain and a poorly localized aching and/or clicking in the posterior aspect of their involved shoulder more often than actual instability symptoms. [1] [4][6] [7] They may carry their arm in an internally rotated position revealing a prominence of the humeral head on the posterior shoulder, with the coracoid process also appearing more prominently. [8] This pain or sense of instability is often elicited when their arm is in the position of forward flexion, adduction, and internal rotation. [1] [6] [7] For overhead athletes this translates into feeling PSI symptoms during their follow through phase or pull-through phase if they are a swimmer. [1] Depending on the mechanism of injury, patients may report a traumatic incidence leading to dislocation & reduction of the shoulder or a more insidious onset often from repeated overuse. [1] [7] Some patients may also be able to volitionally sublux their shoulder [1] [3]
Differential Diagnosis
Diagnosing posterior instability may be difficult because some of the symptoms are similar to other conditions of the shoulder or patients may have other concomitant injuries. [4] If a patient’s main complaint is vague shoulder pain, the clinician may first need to rule out injuries such as a SLAP or [4] Also, patients with PSI may test positive for [9] Furthermore, PSI patients often report feeling pain or unstable when their arm is in a forward flexed, adducted and internally rotated position; however, this is also a position of discomfort for patients with subacromial impingement. To distinguish the two impairments, patients with subacromial impingement should not test positive for the PSI diagnostic tests. [6]
It is also important to distinguish PSI from other versions of shoulder instability, especially multidirectional instability (MDI). Multidirectional instability is defined as “involuntary symptomatic shoulder laxity in more than one direction”. [3] Some patients with PSI may also have a sulcus sign, which is considered an indication of inferior shoulder instability. While some clinicians automatically categorize these patients as having MDI, Fritsch & Taylor suggest that if it is an asymptomatic sulcus sign (no pain is elicited) then it is insignificant and the patient may only have posterior instability.
Examination
Physical Exam
As with any injury it is important to rule out the joints above and below for possible involvement, and therefore a complete upper quarter exam is recommended.
The shoulder exam should include observation, palpation and manual testing that includes motion, strength, and laxity tests of both the involved shoulder and the uninvolved shoulder for comparisons. [4] [10] Upon observation the therapist should be looking for any obvious dislocation or asymmetry of the shoulders, abnormal motion, muscle hypertrophy or atrophy, swelling, and an altered scapulothoracic movement. [4] The patient may have tenderness with palpation at the posterior glenohumeral joint line. [4] They may also present with weakness of the rotator cuff muscles and scapular stabilizers. Diagnostic tests for posterior instability include: the Posterior Apprehension/Stress Test, the Jerk Test, the Kim Test, the Load-and-Shift, and Posterior Drawer Test. [4] [7] [9] [10] [11] [12] [13] During these tests the clinician is trying to reproduce the subluxation or the patient’s symptoms of pain and instability.
Jerk Test [14] Posterior Apprehension/Stress Test [15]
Posterior Drawer Test [16] Kim Test [17]
Imaging
It is important to determine the cause, degree and direction in order to properly treat PSI and prevent recurrent instability. Plain radiographs are often interpreted to be normal in patients with PSI, but may reveal any possible damage to the glenoid. [4] [7] [12] In addition to the routine anterior-posterior and lateral radiographs, it is recommended that patients also get an Axillary view, as it reveals the most diagnostic information for a posterior dislocation or subluxation. [4] [10] However, Magnetic Resonance (MR) Imaging, especially MR arthrography, is the radiological tool of choice and an important diagnostic tool to identify any possible soft tissue lesions that may be contributing to or associated with the instability. [3] [4] [6] [7] [10] [12] MR imaging may also be used to help determine if the patient would benefit from an open surgical approach or an arthroscopic approach. [6] If a plain radiograph reveals there may be bony abnormalities then Computerized Tomography (CT) scans are recommended for their ability to better delineate bone quality and glenoid morphology. [10] [12]
Medical Management
Operative stabilization should be considered in patients who fail to return to activity or continue to experience pain or instability, are psychologically stable, and have failed a trial of physical therapy. [1] [4] The success of surgical intervention depends on the ability to correct the underlying impairment. Therefore, operative treatment may involve more than one procedure to address the factors contributing to the instability. [1] Factors that influence the choice of operative intervention include volitional instability, injury to the shoulder, degree of instability, structural abnormalities, and direction of instabilities. [1]
Volitional Instability
Operative treatment is contraindicated for patients with voluntary instability due to psychological problems. Patients without psychological problems usually respond well to a trial of physical therapy that includes pain management, activity modification, and strengthening of the scapulothoracic and rotator cuff muscles. [1] Operative treatment is usually recommended if conservative treatment fails after a trial of 6 months. [1]
Shoulder Injury
In patients with posterior instability with a traumatic etiology, operative treatment is recommended because conservative treatment is usually unsuccessful. [1] [3] Bottoni et al. found good results in patients with posterior instability secondary to trauma after an open or arthroscopic procedure. [3]
Degree of Instability
Patients with recurrent dislocation often have anterior defects of the humeral head and posterior defects of the glenoid rim. In these patients, operative treatment may include bone-grafting of defects of the humeral head and glenoid rim, and soft-tissue reconstruction. In cases of recurrent subluxation, posterior-soft tissue stabilization is often performed. [1]
Structural Abnormalities
Recently, the trend in operative intervention has been towards lesion-specific surgery to correct soft-tissue or boney abnormalities. [1]
In cases of soft-tissue injury, correction of the abnormalities can be performed with open or arthroscopic procedures. Operative treatment for soft tissue structures typically involves the reattachment of the posteror capsulolabral complex and retensioning of the redundant posteroinferior aspect of the capsule. [1] [3]
- Open procedures for posterior instability secondary to soft-tissue abnormalities include the posterior capsular shift, scapularis tendon transfer, posterior-capsular plication with infraspinatous advancement, reverse Putti-Platt plication, reverse Bankart repair, Boyd-Sisk procedure, and biceps tendon transposition. [1] [4] The open technique is usually performed posteriorly with an incision of the infraspinatous tendon or the development of a plane between the infraspinatous and teres minor tendons. [1] [18] A capsulotomoy is performed through which the labrum is reattached to the glenoid rim with bone tunnels, bioabsorbable tacks, or suture anchors. [1] Complications include infection, neurovascular injury, pain, stiffness, and weakness. Recurrent instability following an open soft-tissue stabilization has been reported to be 24%. [1]
- Arthroscopic procedures for posterior instability secondary to soft-tissue abnormalities include posterior-labral repair, plication, superior shift, thermal shrinkage of the posterinferior aspect of the capsule, subacromial decompression and rotator cuff repair. [1] Patients that report the most successful outcomes from arthroscopy are those with unidirectional instability with capsulolabral lesions. [1] Those that undergo arthroscopic treatment report higher overall outcome scores, less postoperative pain, and shorter hospital stays. [1] [4] Similar outcomes were observed between throwers and nonthrowers following an arthroscopic posterior capsulolabral repair. [19] Arthroscopic stabilization has had good results with 5% overall recurrence rate. [1] [3] [20]
In cases of bony abnormalities, open procedures to correct the bony structures include a posterior glenoplasty, bone-block, or rotational osteotomy of the proximal humerus. [1] [4] A posterior glenoplasty is used to treat patients with glenoid retroversion greater than 15 degrees. [1] [20] A posterior bone-block operation has been used in patients with a deficiency of the posterior wall of the glenoid or with attenuation of the posterior capsule. [1] The bone-block procedure is performed by creating an incision between the posterior and middle deltoids, and infraspinatous muscles, followed by the fixation of an iliac crest bone graft on the posterorinferior quadrant of the glenoid. [20] Typically, a posterior bone-block is performed on patients with recurrent posterior dislocation. [20] These procedures have a high risk of severe complications and are not commonly used. There is a 25% recurrence rate of instability following an open glenoid osteotomy or bone-block procedure. [1]
Physical Therapy Management
Although there are articles describing the following physical therapy treatment and this treatment is commonly accepted as best practice, a systematic review by Gibson et al found little “definitive, empiric evidence to substantiate their effectiveness,” [21](LOE1a) but concludes that conservative physical therapy treatment should be the first line treatment especially for those patients with isolated dislocations. [9] [21](LOE1a) The treatment parameters described are mostly based on biological evidence rather than clinical trials.
Immobilization
Immobilization for three weeks may be indicated for patients under 30 years of age with primary dislocation to help prevent recurrence of dislocation and instability in the joint. [22](LOE4) One week of immobilization was sufficient for patients over the age of 30. Younger patients were more likely to redislocate than older patients within the year follow up period of the study. [22](LOE4) A limitation of this study was that it was not differentiate what direction of dislocation had occurred.
Strengthening
Rehabilitative treatment of PSI includes strengthening of the rotator cuff (supraspinatus, infraspinatus, teres minor, subscapularis) [4] [9] [23](LOE4) most importantly the infraspinatus muscle. [3] [7](LOE1a) [9] [12](LOE1a) Scapular stabilizers [3] [4] [7](LOE1a) [9] [10](LOE1a) and posterior deltoid [7](LOE1a) [24](LOE2b) strengthening is also important. Strengthening exercises engage the muscular stabilizers of the shoulder joint to compensate for the stretched capsule that often occurs with shoulder instability and to promote proprioception of the joint. [3] Isometric, concentric and eccentric strengthening is indicated with focus on correct muscle firing and position before moving to more advanced strengthening of glenohumeral muscles. [9] Resistance can be given through manual techniques, resistive tubing, free weights, or machines. [4] An upper body ergometer may be used to improve dynamic stabilization by demanding coordinated and consistent muscle activity across both arms without moving the arm through painful or unstable motions. [5] (LOE2b)
Biofeedback and EMG
Simply strengthening the rotator cuff muscles may not be enough because of the underlying lack of muscle firing synergy and abnormal recruitment pattern of muscles commonly seen in posterior instability patients. [3] [4] These deficits have been documented through EMG studies. [7](LOE1a) [10](LOE1a) [24] To help focus muscular activity on dynamic stabilizers biofeedback can be useful. [7](LOE1a) [10](LOE1a) [13](LOE5) [21](LOE1a) A case study and case series using EMG biofeedback on the posterior deltoid for neuromuscular reeducation was shown to help the patient activate the posterior deltoid to prevent voluntary dislocations. [24](LOE2b) [25](LOE1a)
Neuromuscular reeducation
Neuromuscular reeducation is an important part of activating scapular and glenohumeral muscles during functional movements. Strengthening should progress to include full range and diagonal and spiral patterns including PNF patterns. [9] Further study is needed to determine if UBE training will normalize muscle activation patterns. [5](LOE2b)
Activity modification
Avoiding activities that encourage instability or symptoms such as the forward flexed, adducted, internally rotated position is recommended. [7](LOE1a) Often the instability is only present during sport and activity modification is not realistic unless the person is willing to retire from sport. [7](LOE1a) [23](LOE4)
Effectiveness
Physical therapy usually cannot eliminate the instability but reports of 70% [7](LOE1a) to 80% [10](LOE1a) [26](LOE2b) of patients note improvement and an ability to return to sport after a physical therapy program. [7](LOE1a) [26](LOE2b) 68% of patients in a retrospective study were satisfied with their results from a rehabilitative strengthening program. [23] (LOE4)The effectiveness of physical therapy depends on the type of instability and the demands the patient places on their shoulder. After an extended period of 12 weeks [9] [21](LOE1a) to 6 months [1] [13] of rehabilitation without improvement and persistent disability, surgery should be considered, as long as the instability can be attributed to an anatomical problem. [7](LOE1a) [23](LOE4)
Bottom Line Physical Therapy
A physical therapy program should include general strengthening with a UBE then start with scapular stabilizing muscles including the middle trap, lower trap, rhomboids, posterior delts, and serratus anterior exercises. These muscles should be activated with minimal arm movement at first emphasizing muscle activation control starting in supine and progressing to sidelying and standing. The posterior delt specifically has been shown to respond to EMG training and this should be utilized as appropriate. [24](LOE2b) [25](LOE1a) As the patient progresses the weight of the arm can be used as an effective lever for increasing the difficulty of the exercise; weights can also be added. The next progression is PNF patterns and functional movement on a stable scapula including shoulder diagonals, flexion, and extension. Rotator cuff strengthening is then added on the stable base of the scapla, focusing on ER starting with shoulder by the side isometrics, closed chain activities and progressing to sport specific ROM with increasing resistance and elevation of the shoulder.
Post-surgical Physical Therapy
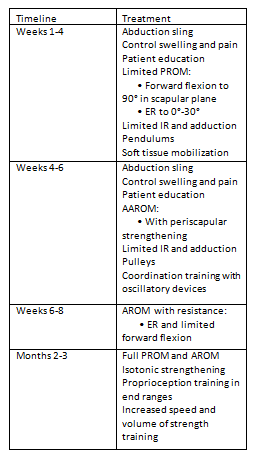
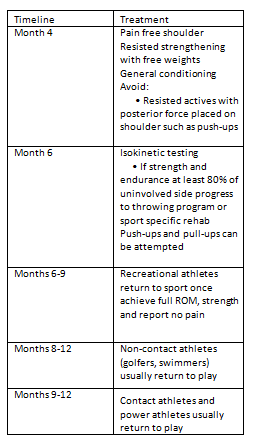
Post-surgical rehabilitation does not differ significantly from conservative treatment without surgery. The goals of treatment are the same and treatment includes ROM, neuromuscular reeducation/function, and strengthening.
Strengthening
Again, the rotator cuff and periscapular muscles are important dynamic stabilizers of the joint and much of the rehabilitation is focused on these muscles. [7](LOE1a) [27] Gentle isometric contraction is suggested as the first active muscle contraction progressing to AROM and resisted exercises. [27]
Range of Motion
The need to restore normal ROM is an important outcome for the success of posterior shoulder instability post-surgical rehabilitation. The anatomy of the repair, tissue involved, patient motivation, and complications are factors that play a large role in the success and progression of a rehabilitation program. [27]
Neuromuscular Function
Supporting musculature of the scapula need to function properly to decrease the stress on the static stabilizers of the joint such as ligamentous and capsular structures that may have been compromised with surgery. [27] This includes strength, muscle firing timing, endurance, and coordination. [27] Rhythmic stabilization can be used to promote proper muscle firing and enhance stability. [27] EMG biofeedback has also been used successfully post surgically to reeducate muscle patterns, specifically the posterior deltoid. [25](LOE1a)
Treatment Timeline for post-surgical rehabilitation
Table 1. Treatment timeline [4] [7](LOE1a) [13][27]