Progressive Supranuclear Palsy (PSP) is a rare degenerative brain disorder that affects movement, control of walking and balance, vision, speech, and cognition. PSP is a type of parkinsonism[1]. The term parkinsonism encompases movement disorders that are characterized by tremor, bradykinesia, rigidity, and postural instability[2]. The most common type of parkinsonism is Parkinson’s disease (80%). Another, much less common cause of Parkinsonism is Progressive Supranuclear Palsy[1]. The disorders name refers to the disease worsening (progressive) and causing weakness (palsy) by damaging the brain above nerve cell clusters called nuclei (supranuclear). These nuclei predominantly control eye movement[1].
The cause of Progressive Supranuclear Palsy (PSP) is not known. The signs and symptoms that appear with PSP are caused by the deterioration of brain cells in the brainstem, cerebral cortex, cerebellum and basal ganglia. These areas are important for the control of body movements (midbrain) and thinking (frontal lobe)[3].
This deterioration is due to the abnormal amount of protein called tau[4]. There are many theories about the causes of PSP, however research is focused on genes that may predispose an individual to developing the disease, as well as ways to prevent clumping of tau in treating the disorder[1]. The cells no longer work properly and die; this is the trademark of the condition. The most affected area in the brain is the substantia nigra. The larger the impact to the substantia nigra, the greater the visible signs and symptoms of the palsy[3].
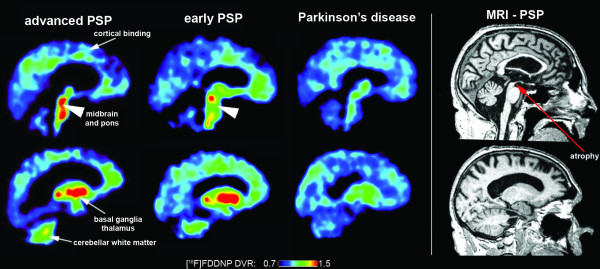
Tau ligand binding patterns in progressive supranuclear palsy
Despite being an uncommon neurological disease, PSP is the most common of the degenerative forms of atypical parkinsonism[4]. PSP is more common in men than women, with signs and symptoms of this disorder usually becoming apparent in mid-to late adulthood. Age of onset is typically in the 60’s[5]. After the onset of the disease, the symptoms continue to worsen and cannot be cured.
Most people with PSP survive 5 to 9 years after the first signs and symptoms appear[6]. It is uncommon for people to live for over a decade after the disease appears. Estimates vary, however it has been confirmed by research that PSP has a worldwide prevalence of 3 to 6.4 per 100, 000 of the population. Many cases (4 – 5 in 100, 000) remain undiagnosed[6].
The most early signs of PSP are related to balance[7]. A loss of balance, sometimes resulting in backward falls, is often seen as the disease progresses[1]. Moreover, as the disease continues to progress people have an increased difficulty with movement. Many movements become slow and clumsy, with more pronounced gait difficulties[7]. With walking, each step becomes slow and deliberate with broad-based steps[1]. Eventually, most PSP patients require wheelchair assistance due to balence issues[7].
Another characteristic feature of PSP is visual problems[7]. Abnormal eye movements develop several years after other movement dysfunctions and often present as an inability to move the eyes up and down. In addition, difficulty opening and closing the eyelids, infrequent blinking, and retraction of the eyelids can also be seen. All of these abnormalities with the eyes can lead to blurry vision, double vision, light sensitivity and a staring gaze. In very advanced stages the eyes may not move at all[1].
Additional symptoms of PSP may include difficulties with swallowing (dysphagia) and speech (dysarthria)[1]. As the dysphagia becomes more severe, aspiration pneumonia becomes a concern.
In addition, most PSP patients also develop personality, behaviour and cognitive changes[7]. Personality changes are often presented as apathy (loss of interest and enthusiasm). Cognitive changes present as difficulties with cognition, attention, planning and problem solving[3].
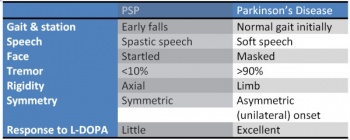
There are no known laboratory tests or imaging techniques that can specifically diagnose PSP at this time[4]. A diagnosis is generally made using the patient history in combination with both physical and neurological scans. Often times an MRI will demonstrate changes in activity in affected cortical areas, as well as shrinkage and plaque development due to neuronal loss in the basal ganglia, cerebellum and brainstem[8]. Symptoms of PSP often mimic other diseases and movement disorders, with the development of cardinal signs varying widely in developmental timing and severity between cases. The disease is characterized by gait disorders, postural instability and rigidity, ophthalmoplegia, dysphagia and dysarthria, and frontal cognitive disorders[8]. Gait instability and resultant falls are often the earliest sign, and are considered key to early diagnosis. This is followed by visual disorders often ranging from diplopia, blurred vision, light sensitivity, inability to look up/down and burning sensations, slurring of speech and lastly cognitive slowness, memory issues, changes in personality or mood[8][4].
There is little known long term benefit to drug agents in this disease, despite it’s parkinsonian presentation[4]. Occasionally, bradykinesia and stiffness of gait can be altered transiently with levodopa, and botulinum toxin often can decrease involuntary eye closing and results in no long term effects. Non-drug treatments for PSP can include assistive walking devices for prevention of falls (often include counterweights for extensor postures). Often people are prescribed prism glasses which treat the patient’s decreased ability to look down, allowing better visual input for balance and walking[4]. There is some evidence of exercise through physiotherapy for the maintenance of strength, coordination and balance in these patients[9].
PSP is often misdiagnosed as it is quite rare. The diagnostic criteria includes vague statements and often is decided upon when all other options are ruled out[4]. The signs and symptoms also mimic many other common disorders, such as Parkinson’s Disease, due to the unsteadiness of gait. The common memory problems and personality changes often lead to physicians mistakenly diagnosis PSP as depression or dementia. More common differential diagnosis may include[10]:
Since there is no medication available to treat this condition[4], patients are often referred to physiotherapy in order to manage their symptoms. Most physiotherapy interventions for PSP include an exercise regimen that consist of[9]:
- Aerobic exercises
- Transfer/balance training
- Gait training
- Weighted tool can be used to prevent backwards falls
- Flexibility training[6]
- Intensive routines
- Goal oriented tasks
- Visual tracking
- Prism lenses sometimes used to further train gaze[6]
- Motor-cognitive exercises
An exercise program following these guidelines is recommended for about 1-2 hours a day, 5 days a week, in order to show any significant improvements[9].
References
- ↑ 1.01.11.21.31.41.51.61.7 Parkinson Canada. Progressive Supranuclear Palsy. ↑ International Parkinson Movement Disorder Society. Parkinson’s Disease & Parkinsonism. ↑ 3.03.13.2 Webmd. Parkinson’s Disease and Progressive Supranuclear Palsy. ↑ 4.04.14.24.34.44.54.64.7 National Institute of Neurological Disorders and Stroke. Progressive Supranuclear Palsy Fact Sheet. ↑ Parkinson’s Association of Ireland. Progressive Supranuclear Palsy – PSP (and Cortico Basal Degeneration – CBD) ↑ 6.06.16.26.3 Johns Hopkins Medicine. Progressive Supranuclear Palsy. ↑ 7.07.17.27.37.4 US National Library of Medicine. Progressive Supranuclear Palsy. ↑ 8.08.18.2 Agid, Y., Duyckaerts, C., Hauw, JJ., Verny, M. The significance of cortical pathology in progressive supranucleur palsy [abstract]. PubMed 1996; 1123-36.
- ↑ 9.09.19.29.39.4 Clerici I, Ferrazzoli D, Maestri R, Bossio F, Zivi I, Canesi M, Pezzoli G, Frazzitta G. Rehabilitation in progressive supranuclear palsy: Effectiveness of two multidisciplinary treatments. PloS one. 2017 Feb 3;12(2):e0170927.
- ↑ 10.010.1 Progressive Supranuclear Palsy Differential Diagnoses. ↑ 11.011.111.2 Hall DA, Forjaz MJ, Golbe LI, Litvan I, Payan CA, Goetz CG, Leentjens AF, Martinez‐Martin P, Traon AP, Sampaio C, Post B. Scales to Assess Clinical Features of Progressive Supranuclear Palsy: MDS Task Force Report. Movement Disorders Clinical Practice. 2015 Jun 1;2(2):127-34.