Background
Dementia is a broad term used to describe a group of symptoms associated with ongoing decline of the brain’s abilities. Symptoms include impairments of[1]:
- Memory
- Intellect
- Language
- Insight
- Social skills
While Alzheimer’s disease is the most common cause, possibly accounting for 60-70% of all cases[2].
Dementia mainly affects people over the age of 65 and its incidence increases with age[3]. Around the world, 50 million people are believed to have dementia with millions of new cases each year[2]. Dementia affects a large percentage of the UK population. There are currently around 750,000 people in the UK living with dementia, and this is expected to rise to 1.4million by 2039[4].
To maintain quality of life of people with dementia (PWD), it is essential to maintain their independence as long as possible. However, due to the progressive deteriorating nature of dementia this can become increasingly difficult.
Estimates of the proportion of people with dementia who live in care facilities range from 19%[5] to 49%[6] meaning there are many informal carers e.g. family members and friends assuming the role of primary carer for their loved ones. Research suggests that carers of people with dementia often display poor health as compared to their age matched peers[7] and therefore require as much assistance as possible to be able to support PWD, while maintaining their own well being.
Noticing Danger Signs
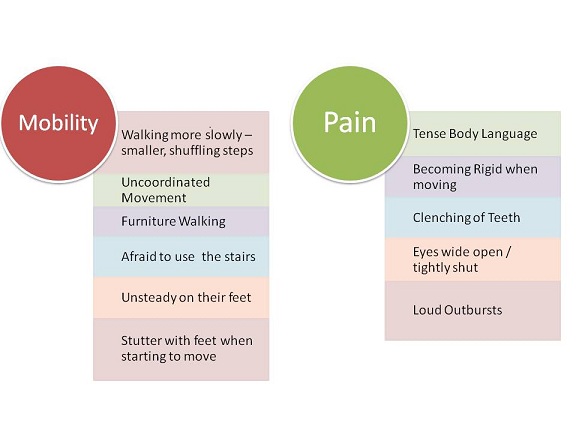
As dementia progresses, a person may start behaving differently, being less physically active or begin struggling to communicate with other people. There are several ‘Dementia Danger Signs’ that you should be aware of, these are listed below. If any of these are present, it is important to use methods to help these individuals to maintain their mobility and function.
As the disease progresses problems with mobility will increase[8]. Some people with dementia eventually become confined to a bed or chair. Physiotherapist can help if danger signs are present regarding mobility and difficulty completing daily activities giving advice on how to help the person to move without injuring themselves is invaluable and can ensure the safety of the client and the carer..
Most dementias will at some point in their course affect areas of the brain that are responsible for a person’s movement and balance. By exercising and keeping active, PWD keep their joints, muscles and heart in good shape and build a reserve. Exercise and participating in activities also provide an opportunity for PSE to engage with their surroundings.
Advise the caregiver for a PWD, how to encourage activity safely. The folloing is very useful advice: A physiotherapist provides assistance and support to the PWD by tailoring a unique programme for them. This includes[3]:
Chronic pain is significant among older adults, particularly those with dementia. Between 43% and 71% of people suffering with dementia are in pain[9]. Yet pain is under diagnosed and under treated in this population[10].
Some dementia patients have trouble communicating their pain experience to their carers or family members because of dementia. In severe cases of dementia, this can leave pain levels being under treated as many believe that pain is a normal and expected part of getting old and that PWD can’t feel pain. However, these are both untrue and pain can be treated with dementia patients through a good working relationship between both the carer/family and the physiotherapist and GP.
For help in looking out for signs of pain in PWD see the What a Physiotherapist Can Do
It is important to know that pain can affect an individuals motivation to do any exercise or activities. If pain becomes a problem with your loved one, your physiotherapist can provide information to help recognise pain and put in place strategies to help lessen pain levels and improve the quality of life of the patient.
The Coloured Analogue Scale[11] is a scale often used by both physiotherapists and carers to measure the amount of pain that the patient is feeling. The scale goes from 0-10 and the colour changes as the amount of pain changes. The patient is asked to use a sliding bar to tell the carer or physiotherapist what level of pain they are feeling. However it has to be used with caution as the reliability of the scale decreases as the disease progresses. As the patient goes from having mild to severe dementia the scale has been shown by scientific research not to give as true a reflection of how much pain the PWD is feeling[12].
For PWD who are non-verbal, the Dangers at Home
Individuals with dementia are up to eight times more likely to fall compared to those with no cognitive impairment[13]. Many of these falls can result in hospital admissions. The home can be full of potential tripping hazards for a person with dementia. To prevent falls, try to ensure the home environment is free of obstacles. Some methods to help with this are;
If more assistance with is required in the home environment or the client needs a home assessment then it may be necessary to seek the involvement of an Occupational Therapist (OT).
It is important that a caregiver is encouraged to look after their own needs. Here are a few recommendations you can share to help them cope with the demanding role of looking after someone with dementia.
References
Keeping Active
How Can Physiotherapy Help?
Recognising Pain
How Can a Physotherapist Help?
Caring For The Carer
Where to Get Help
Ola!
Como podemos ajudar?