Introduction
Pudendal ( Latin pudenda, meaning “external genitals”, derived from pudendum, meaning “parts to be ashamed of”[1].
Neuralgia (Greek neuron, “nerve” + algos, “pain”) is pain in the distribution of a nerve or nerves[2].
It is a chronic neuropathic pelvic pain that is often misdiagnosed and inappropriately treated by many practitioners.It occurs in both men and women, although studies reveal that about two-thirds of those with the disease are women. The primary symptom is pain in the genitals or the anal-rectal area and the immense discomfort is usually worse when sitting. The pain tends to move around in the pelvic area and can occur on one or both sides of the body. Sufferers describe the pain as burning, knife-like or aching, stabbing, pinching, twisting and even numbness[3].
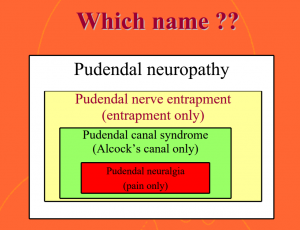
Pudendal neuralgia (PN) : is used interchangeably with “pudendal nerve entrapment”, but a 2009 review study found both that “prevalence of PN is unknown and it seems to be a rare event” and that “there is no evidence to support equating the presence of this syndrome with a diagnosis of pudendal nerve entrapment,” meaning that it is possible to have all the symptoms of pudendal nerve entrapment (otherwise known as pudendal neuralgia) based on the criteria specified at Nantes in 2006, without having an entrapped pudendal nerve[4][5].
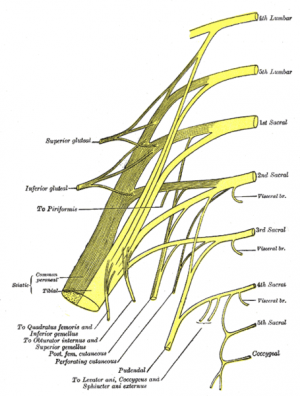
Clinically Relevant Anatomy :
The pudendal nerve is paired, meaning there are two nerves, one on the left and one on the right side of the body.
- Nerve roots – S2-S4
- Sensory – innervates the external genitalia of both sexes and the skin around the anus, anal canal and perineum
- Motor – innervates various pelvic muscles, the external urethral sphincter and the external anal sphincter.
- Autonomic – carries sympathetic nerve fibres to the skin of the S2-S4 dermatomal region.
Pudendal nerve entrapment at different levels (ischial spine, sacrospinous, and sacrotuberous ligament, Alcock’s canal) is a cause of disabling, chronic, and intractable pelvic pain that is eminently variable and complex as it is often associated with multiple, perplexing functional symptoms[7].
Pathophysiology:
The exact mechanism of nerve dysfunction and damage is dependent on its etiology.
It can be unilateral or bilateral.
Causes include compression, stretch, direct trauma, and radiation. Pudendal neuralgia is a functional entrapment where pain occurs during a compression or stretch maneuver. The neuropathy worsens due to repetitive micro-trauma resulting in persistent pain and dysfunctional complaints. The pudendal nerve is compressed during prolong sitting and cycling.
Stretch of the nerve by straining with constipation and childbirth can cause pudendal neuropathy. Fitness exercises, machines, weight lifting with squats, leg presses or karate with kick boxing and rollerblading are all etiologic factors. Youthful sports are a common denominator, possibly related to bony remodeling of the ischial spine. Driving over rough roads or farm fields causes vibration trauma. Falls onto the buttocks can cause pudendal neuralgia[10].
Clinical Presentation :
Clinical characteristics include pelvic pain with sitting which increases throughout the day and decreases with standing or lying down, sexual dysfunction and difficult with urination and/or defecation. To confirm pudendal neuralgia, the Nantes criteria are recommended[11]. The pain sensations are similar to other entrapment neuropathies.
In most cases, patients will describe neuropathic pain – a burning, tingling, or numbing pain – that is worse with sitting, and less severe or absent when standing or lying down.
Initially, pain may be present only with sitting, but with time pain becomes more constant and severely aggravated by sitting. Many of my patients cannot tolerate sitting at all. Interestingly, patients usually report less pain when sitting on a toilet seat, a phenomenon that we believe is associated with pressure being applied to the ischial tuberosities rather than to the pelvic floor muscles. Pain usually gets progressively worse through the day.
Diagnostic Procedures:
Pudendal neuralgia can be very difficult to diagnose, as no specific test exists[12]. Therefore, diagnosis of this condition relies heavily on a proper history and physical examination[13].
Diagnostic criteria defined by Robert Nantes are used widely. Five essential criteria must all be present: pain limited to the territory of innervation of pudendal nerve, pain predominant during sitting, pain does not awaken patient from sleep, no objective sensory defects, positive effect of anesthetic infiltration of the pudendal nerve[14].
Objectively this criteria determines the baseline function of a patient at the beginning of treatment. Once treatment has commenced, the same instrument can be used to determine progress and treatment efficacy.
Physical examination focuses on a simple pudendal neurological evaluation. Pinprick sensation is tested at each branch bilaterally: dorsal nerve (clitoris and glans penis), perineal nerve (posterior labia and posterior scrotum), and inferior anal nerve (posterior perianal skin). Hyperalgesia is more common than hypoalgesia. Normal sensation to pinprick may occur even when quantitative sensory testing is abnormal. Pressure is placed on the nerve at the Alcock canal and medial to the ischial spine attempting to reproduce pain, bladder, or rectal symptoms—the Valleix phenomenon[15].
MRI allows PN to be classified, based on the entrapment site: Type I, in the sciatic notch; Type II, the ischial spine and Sacrosciatic ligament; Type IIIa, the obturator internus muscle; Type IIIb, the obturator internus and piriformis muscles, and Type IV, the distal branches of the pudendal nerve.
Outcome Measures:
- Visual Analogue Scale (VAS).
- McGill Pain Questionnaire(MPQ).
- DN4 (which stands for Douleur Neuropathique 4).
- Brief Pain Inventory – Short Form (BPI-sf).
Management / Interventions:
Medical Management:
3 main types of drugs preferred according to symptoms which needs to be addressed.
- Muscle Relaxants.
- Analgesics.
- Anti-convulsants.
Invasive Interventions: These are performed by experienced practitioners[16].
- Pudendal Nerve Release Surgery. An entrapped pudendal nerve can be approached through 3 different types of surgeries:
- Trans-ischio-rectal (TIR)
- Trans-gluteal (TG)
- Trans-perineal (TP) In some cases, patients may experience post-operative pain. In this situation, physical therapy plays a big role in recovery.
- Botox / Botulinum toxin Type A injections.
- Pulsed radio-frequency treatment of the pudendal nerve, sacral nerve roots or sacroiliac joints.
- Cortisone injections.
- Activated platelet extract injections (PRP platelet-rich plasma).
- Hyaluronic acid injections.
- Neuro-modulation with implantable electrodes.
The selection of candidates for surgery should always include a single diagnostic anesthetic injection of the pudendal nerve, as the fifth of the Nantes criteria is an effective predictor of the success of surgery[17].
Clinical management depends on the cause of distress to the nerve. When the cause is not obvious patients are advised to try the least invasive and least risky therapies initially.[16]
Non-invasive or Conservative Therapy:
Physiotherapy: Long term goal is to be pain free and improve quality of life.[18]
A physical therapy evaluation includes a movement assessment that will identify poor movement patterns that contribute to your symptoms. Often, evaluation also includes a gentle internal assessment of your pelvic muscles. This will give us information about your muscles’ ability to both contract and relax.
Treatment includes :
- explanation of pain mechanisms as it relates to your case,
- correction of body mechanics, position or activity modification,
- internal manual therapy to facilitate healthy muscular contraction and relaxation (if applicable)[19].
Pelvic Floor Relaxation exercises are most preferred strategy used by physiotherapists who specialize in pelvic floor dysfunction and disorders.A research study, completed by Peter Doran and Michel Coppetiers, two physiotherapists in Australia, reported on a protocol for the treatment of the pelvic girdle for pudendal nerve involvement. They had good success with a small group of patients using externally driven techniques to mobilize the sacro-iliac joints, decreasing tension on the sacrotuberous and sacrospinous ligaments. This is a non-invasive approach that should be considered before more aggressive approaches be attempted.[20].
Patient Self-Managment: Patient should use a cushion( Doughnut or C-Shaped) that supports the ischial tuberosities to elevate the pelvic floor off the seat. This support decreases the pressure applied to the pelvic floor muscles and pudendal nerve. Avoidance of postures or movement which triggers pain.
Exercises :which relax tensed pudendal nerve and will provide temporary relief are:
- Wide leg bridges.
- Standing backward leg lifts.
- Side lying hip abduction and extension.
- Hip extension in quadruped position.
- Cobra pose.
- Arch Backs.
Efficacy of specific exercises or yoga asanas in dealing with chronic pudendal neuralgia is an unexplored area which demands research.
Differential Diagnosis
- In Males: Abacterial chronic prostatitis, prostatodynia, idiopathic proctalgia.
Prognosis
PN greatly affects quality of life, but has no effect on life expectancy. Many sufferers report on medical forums and community support groups to have suffered depression and unrelenting discomfort due to PN which gradually reduced upon right diagnosis and treatment.
Summary
Pudendal neuralgia is a painful neuropathic condition involving the dermatome of the pudendal nerve. It should be suspected in patients complaining of burning pain in the clitoris/penis, vulva/scrotum, perineum, and rectum. Pain is more severe with sitting, and relieved or improved by standing. Onset is usually immediately after vaginal surgery, pelvic trauma, or childbirth. The Nantes criteria are used for the diagnosis of pudendal neuralgia. CT guided pudendal nerve blocks are more precise than transvaginal injections for diagnosis. Initial therapies include minimizing activities that worsen the pain and pain medications. Physical therapy and Botox injections are used in patients identified with pelvic floor tension myalgia. When conservative treatments fail, surgical decompression or pain blocking methods are performed. Knowledge and best practice in this field are changing rapidly; therefore changes in diagnosis and treatment protocols are expected[21].
References
- ↑ Harper, Douglas. ↑ ↑ Beco J, Matthews V. ↑ Stav K, Dwyer PL, Roberts L. ↑ Thoumas D, Leroi AM, Mauillon J, Muller JM, Benozio M, Denis P, Freger P. Pudendal neuralgia: CT-guided pudendal nerve block technique. Abdominal imaging. 1999 May 1;24(3):309-12.
- ↑ Relevant Anatomy Of Pudendal Nerve And Etiological Factors of Pudendal Neuropathies, ↑ Calabrò RS, Gervasi G, Marino S, Mondo PN, Bramanti P. ↑ Master’s Degree Project of Courtney McKenna from the Department of Art as Applied to Medicine, Johns Hopkins University_ © 2012 Courtney McKenna Available from ↑ Pudendal Nerve Palsy Bicyclist Injury by Dr. Nabil Ebraheim. Available from:↑ ↑ Pérez-López FR, Hita-Contreras F. ↑ Labat JJ, Riant T, Robert R, Amarenco G, Lefaucheur JP, Rigaud J. Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurourology and urodynamics. 2008 Apr 1;27(4):306-10.
- ↑ ↑ ↑ Antolak SJ. ↑ 16.016.1 Benson JT, Griffis K. Pudendal neuralgia, a severe pain syndrome. American journal of obstetrics and gynecology. 2005 May 1;192(5):1663-8.
- ↑ Charlotte W, Sebastian D, Viviane T, Luc B. ↑ Rosenbaum TY, Owens A. Continuing medical education: the role of pelvic floor physical therapy in the treatment of pelvic and genital pain-related sexual dysfunction (CME). The Journal of Sexual Medicine. 2008 Mar 1;5(3):513-23.
- ↑ Pudendal Neuralgia-entropy-physio.com [ ↑ ↑ function gtElInit() { var lib = new google.translate.TranslateService(); lib.setCheckVisibility(false); lib.translatePage('en', 'pt', function (progress, done, error) { if (progress == 100 || done || error) { document.getElementById("gt-dt-spinner").style.display = "none"; } }); }
Ola!
Como podemos ajudar?