Definition/Description
Radiation therapy is when radiation is delivered to a specific area of the body to try and treat a disease, usually cancer. The goal of the radiation is to kill rapidly dividing cancer cells while sparing slower dividing somatic cells. Radiation is usually used in conjunction with surgery or chemotherapy, so this makes it difficult to separate the effects resulting from each of these treatments. [2]
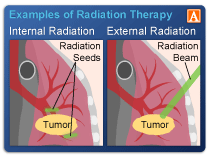
The radiation may be delivered by a machine outside the body (external-beam radiation therapy) or it may come from radioactive material placed in the body (internal radiation therapy, also called brachytherapy).[3]
Type of radiation used depends on:
• Type of cancer
• Size
• Location
• How close the cancer is to normal tissues
• How far the radiation needs to travel
• General health and medical history
• Other types of treatment
• Age and other medical conditions
External-beam radiation therapy: most often delivered in the form of photon beams (x-rays or gamma rays) [3]
3-Dimensional Conformal Radiation Therapy (3D-CRT): most common type
Intensity-Modulated Radiation Therapy (IMRT)
• Dosage is chosen for different areas of the tumor and surrounding tissues
• High-powered computer program calculates the required number of beams and angles
• Goal: increase the dose to areas that need it and reduce exposure to sensitive areas
• Can reduce the risk of some side effects
• Larger volume of normal tissue overall is exposed
Image-Guided Radiation Therapy (IGRT)
• Repeated imaging scans performed during treatment
• Can increase the accuracy and may allow reduction in planned volume of tissue to be treated
• Decreasing total radiation dose to normal tissue
Tomotherapy
• Type of image-guided IMRT
• Hybrid between a CT and an external-beam radiation therapy machine
• Sparing normal tissue from high radiation doses
Stereotactic Radiosurgery
• Can deliver one or more high doses of radiation to a small tumor
• Extremely accurate image-guided tumor targeting and positioning
• High dose of radiation can be delivered without excess damage to normal tissue
Stereotactic Body Radiation Therapy
• Radiation therapy in fewer sessions
• Uses smaller radiation fields and higher
• Treats tumors that lie outside the brain and spinal cord
• Usually given more than one dose
• Can treat only small, isolated tumors; including cancers in the lung and liver
Proton Therapy
• Deposit much of their energy at the end of their path (Bragg peak) and deposit less energy along the way
• Should reduce the exposure of normal tissue
Internal-beam radiation therapy (Brachytherapy): [3]
Interstitial: uses radiation source placed within tumor tissue
Intracavitary: uses a source placed within a surgical cavity or a body cavity
Episcleral: used to treat melanoma inside the eye, uses a source that is attached to the eye
Low-dose: receive continuous low-dose radiation over a period of several days
High-dose: robotic machine attached to delivery tubes placed inside the body, can be given in one or more treatment session, cause less damage to normal tissue
Placement is either permanent or temporary
Permanent
•Surgically sealed within the body and left
• Remaining material does not cause any discomfort or harm
• Low-dose rate
Temporary
• Carrier and the radiation sources are removed after treatment
• Can be either low-dose or high-dose
Systemic Radiation Therapy [3]
Swallows or receives an injection of a radioactive substance or a radioactive substance bound to a monoclonal antibody
Examples: radioactive iodine, ibritumomab tiuxetan (Zevalin®), combined tositumomab and iodine I 131 tositumomab (Bexxar®), samarium-153-lexidronam (Quadramet®), and strontium-89 chloride (Metastron®)
Prevalence
– Nearly two-thirds of all cancer patients will recieve radiation therapy [5]
– There are no good estimates of how many of these patients will develop complications due to the radiation therapy [2]
Characteristics/Clinical Presentation
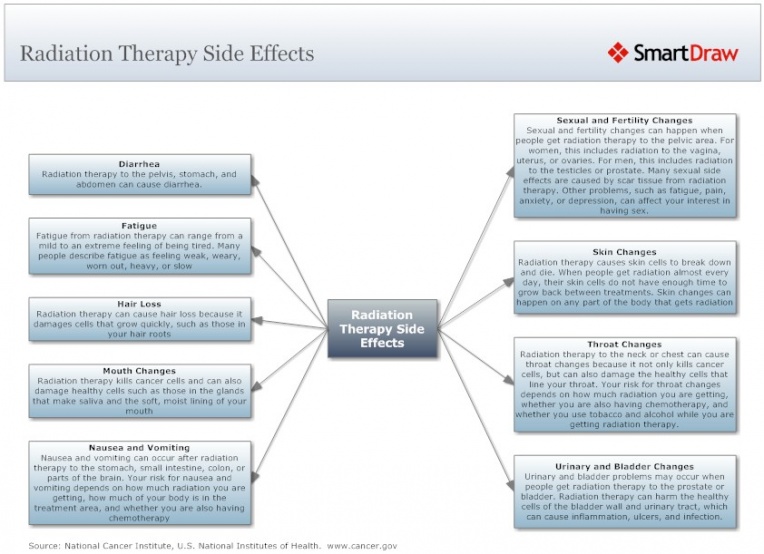
Side Effects[3]
Depend on the area of the body being treated, dose given per day, total dosage, general medical condition and other treatments being given.
Acute (Early)
• Skin irritation
• Damage at regions exposed (salivary glands or hair loss if head or neck treated)
• Urinary problems (lower abdomen treated)
• Fatigue
• Nausea with or without vomiting
• Most disappear after treatment ends (some may be permanent)
Chronic (Late)
• May or may not occur
• Fibrosis (replacement of normal tissue with scar tissue)
• Damage to the bowels
• Memory loss
• Infertility
• Second cancer (rare); highest in those treated for cancer as a child or adolescent
• Some chemotherapy drugs, genetic risk factors, and lifestyle factors can also increase risk of late side effects
Lymphedema[7]
• Swelling that occurs when protein-rich lymph fluid accumulates in the interstitial tissue
• May contain plasma proteins, extravascular blood cells, excess water, and parenchymal products
• Often insidious
• Characteristics
o Non-pitting swelling of either the arm or leg and usually involves the digits
o Early stages: manifest pitting edema until fibrosis develops
o May predispose to recurrent skin infections
• Complaints
o Heaviness or fullness of the limb
o Tight sensation of the skin
o Decreased flexibility
o Ambulation may be affected
• Risk factors
o Undergoing axillary surgery/radiation therapy
o Extent of local surgery
o Local radiation
o Delayed wound healing
o Tumor causing lymphatic obstruction
o Scarring of the left or right subclavian lymphatic ducts
• Grades
o Grade 1: 5-10% interlimb discrepancy in volume or circumference, pitting edema
o Grade 2: >10-30% interlimb discrepancy in volume or circumference, obliteration of skin folds, readily apparent deviation from normal contour
o Grade 3: >30% interlimb discrepancy in volume; lymphorrhea; gross deviation from normal contour interfering with activities of daily living
o Grade 4: progression to malignancy, amputation indicated, disabling
Radiation Fibrosis Syndrome[2]
– Progressive fibrotic tissue sclerosis resulting from radiation treatment
– It affects many different types of tissue including skin, muscle, ligaments, tendons, nerves, heart, lung, gastrointestinal and genitourinary tract, and bone; in order for a structure to be considered affected by this syndrome, it must be within the radiation field or have tendons, neurovascular innervation or lymphatic flow that travels in the field.
– The pathophysiology behind the sclerosis, fibrosis and atrophy is not well understood. Some believe there is a link between vascular endothelial damage and the progression of the fibrosis. When endothelial cells are damaged by radiation they can no longer get rid of the surrounding thrombin causing a profibrogenic effect on smooth muscle cells, fibroblasts, myofibroblasts and other cells.
– Problems may not present for several months or years after treatment
– Usually has a slow, insidious onset and is not reversible
Risk Factors:
– Hodgkin lymphoma
– Age
– Overall health
– Degenerative spine disease
– Exposure to chemotherapy treatment
– Location of radiation
Head and neck cancer, because high doses are needed and there are many vital tissues in that radiation field
– Size of radiation field
– Type of radiation and time since radiation was administered
– Neuropathic pain due to RFS is more likely to occur in those with pre-existing medical disorders involving the nervous system such as diabetes, spinal degeneration and cervical radiculopathy
Structures Affected:
Nerve
– Peripheral Nervous System (PNS): Pain, sensory loss and weakness caused by external compressive fibrosis of soft tissue and ischemia from fibrosis.
– Central Nervous System (CNS): Autonomic Nervous System can be affect resulting in orthostatic hypotension, bowel and bladder changes, and sexual dysfunction
– Neuropathic pain involving both the PNS and CNS is common. It is due to damage of neural structures within the field of radiation.
– Sensory loss is also common including loss of light touch, pain, temperature, vibration and position sensation
– Weakness due to damage of neural structures, including plexopathy and mononeuropathies.
Muscle
– Painful spasms are common due to myopathies, weakened and fatigability of muscles and ectopic activity of the motor nerve
– Localized muscle pain due to sensitization of local pain neurons
Tendon and Ligaments
– Progressive fibrosis and sclerosis causing decreased elasticity, shortening and contractures
– Effects do not always have to be direct. Radiation to the upper leg can cause ankle contractures because the muscles, tendons and vascular structures of the ankle run of the length of the leg.
Bone
– Decreased bone density
– Osteoradionecrosis of the mandible and fractures of the pelvis, hip, long bones and ribs are common
– Radiation in children may cause long bones and the spine to mature abnormally if the growth plate is affected
Common Clinical Syndromes Associated with RFS:
Neck Extensor Weakness – sever atrophy of the cervicothoracic paraspinal and shoulder girdle musculature resulting from damage to the motor nerve and/or the muscle itself
Shoulder Pain and Dysfunction – damage to the cervical nerve roots, brachial plexus, rotator cuff (RTC) muscles, rhomboids and peripheral nerves innervating these muscles all contributes to this dysfunction. May result in RTC tendonitis and adhesive capsulitis
Cervical Dystonia – usually involving the SCM, scalenes, and trapezius. If severe it can affect swallowing, phonation and activities of daily living.
Trismus – impaired mouth opening can result from the invasion of the tumor into the masseter and pterygois muscles, the innervation of these muscles, or the TMJ. It can affect chewing, swallowing, oral hygiene and pulmonary function.
Associated Co-morbidities
Lymphedema[8]
-Cardiac insufficiency
-Venous insufficiency
-Arthritis
-Fungal infection
-Cellulitis
-Psychosocial complications
-Lymphatic cysts
Other Co-morbidities [9]
These co-morbidities can have an effect on how radiation is tolerated:
– Diabetes
– Heart Disease
– Arthritis
Medications
Radioactive iodine
Ibritumomab tiuxetan (Zevalin®)
Combined tositumomab and iodine I 131 tositumomab (Bexxar®)
Samarium-153-lexidronam (Quadramet®)
Strontium-89 chloride (Metastron®)
Amifostine is the only drug approved by the FDA to protect normal tissues (radioprotector)[3]
– It can be used to reduce the frequency and/or severity of radiation induced esophagitis[5]
Diagnostic Tests/Lab Tests/Lab Values
Lymphedema[7]
• Clinical assessment
• Lymphoscintigraphy: imaging of the lymphatic system
• Magnetic Resonance Imaging: complement lymphoscintigraphy, provide detail about anatomy and nodes
• Circumferential upper-extremity measurement: most widely used to diagnose upper extremity lymphedema
Radiation Fibrosis Syndrome
Diagnostic criteria is dependent on area of radiation and what structures are affected.
Etiology/Cause[5]
Risk Factors:
Dependent on organ radiated, individual tolerance, tumor type, volume radiated and fraction size/dosage.
Neurotoxicity
– High total dose and fractionation dose
– Large volume radiated
– Increased edema
– Age 60 years
– Concurrent chemotherapy
– Underlying diseases affecting the vascular structures (Diabetes, HTN)
– Stereotactic radiation surgery and brachytherapy (internal radiation)
Dermatitis
– Total dose/volume and fractionation dose
– Surface area exposed
Acute Enterocolitis
– Large volume
– High total dose and fractionation dose
– Concurrent chemotherapy
Chronic Entercolitis
– Older age
– Postoperative radiation
– Presence of collagen vascular disease
– Concurrent chemotherapy
– Poor radiation technique
Pulmonary
– Older age
– Lower performance status
– Lower pulmonary baseline function
– Large volume treated
Systemic Involvement [5]
Gastrointestinal
Radiation Esophagitis: often involved in radiation treatment for lung cancer especially when a chemosensitizer is also used. Symptoms usually resolve in 1 to 3 weeks after radiation is finished.
Symptoms: abnormal peristalsis, odynophagia (pain with swallowing) and dysphagia
Radiation Enterocolitis: often results in fibrosis leading to strictures in the intestines, bowel obstruction, fistulas with abscess formation, ulceration with bleeding and malabsorption
Acute Radiation Enteritis – decreases the surface area of absorption leading to decreased nutritional uptake and possible dehydration and malnutrition. Symptoms: diarrhea, abdominal cramping, and nausea
Chronic Radiation Enteritis – symptoms don’t occur for 6 months to 25 years after treatment and usually require more serious treatment
Other symptoms may include dry mouth, anorexia, and stomatitis (inflammation of mouth mucosa)
Pulmonary
Radiation Lung Disease
Radiation Pneumonitis (acute): interstitial inflammation creating a decrease in the amount of gas exchanged in the lungs. It can occur 1 to 6 months after radiation and usually resolves in 6 to 12 months. Symptoms: dry cough with dyspnea on exertion or can turn into a severe cough with dyspnea at rest
Radiation fibrosis (chronic): progressive and occurs months after radiation treatment
Other problems may include bronchopleural fistulas, pneumothorax, hemoptysis and bronchial stenosis
Cardiovascular
Radiation Heart Disease – may result in pericarditis, coronary heart disease, myocardial disease and aortic-valve disease
Musculoskeletal
Connective Tissue Involvement – late changes such as fibrosis, atrophy and contraction is common especially in collagen
– In bones and limbs it can cause weakness, limb-length discrepancies and scoliosis
– It can result in edema and decreased range of motion
– It can cause pelvic adhesions that result in painful motion and sometimes plexopathy
– In the circulatory and lymphatic system it can cause loss of elasticity on contractility of vessels. Even though the actual lymph vessels may maintain their shape, fibrosis in the surrounding tissue can inhibit growth of the vessels into tissues that need to be healed.
Nervous System
Acute symptoms: occur during treatment and include debilitating fatigue; cranial radiation may result in short-term memory loss, changes in behavior and cognition, decreased appetite, dry skin, hearing loss, hair loss and decreased salivation
Subacute symptoms: occur 1 to 4 months after treatment and are not as common. Radiation to the cervical spine may result in subacute myelopathy (Lhermitte’s sign). Radiation to the brainstem may result in ataxia, nystagmus and dysarthria
Chronic symptoms: occur months to years after therapy and can include damage to the cerebral vasculature leading to coronary artery disease, transient ischemic attacks, stroke or myocardial infarction.
Radionecrosis – results from whole-brain radiotherapy. Secondary tumors may develop and the hypothalamic system may be affected. Symptoms: headache, changes in cognition and personality, focal neurological deficits and seizures.
Myelopathy – results from radiation of the spinal cord. May present as Brown-Sequard syndrome or motor neuron syndrome.
Plexopathy – results from damage to the brachial and lumbar plexuses. Symptoms may include paresthesias, motor deficits, lymphedema and pain.
Integumentary
Radiation Dermatitis – common since it is involved in most radiation therapy
Acute
Grade 1: resembles a sunburn. Hair follicles and sebaceous glands are damaged and may result in hair loss, pruritis, desquamation, dyspigmentation and scaling due to damage of the hair follicles
Grade 2: persistent erythema or patchy moist desquamation in creases of the skin that is usually painful with some edema
Grade 3: moist desquamation with pitting edema not confined to skin creases
Grade 4: skin necrosis or ulceration of dermis with bleeding
Consequential-late: acute changes that are persistent
Chronic: develop months to years after radiation treatment; may include skin scarring, contractures (atrophic skin susceptible to tearing and ulceration), and secondary malignancies
Other problems may include destruction of nails, delayed wound healing and epidermolysis (loose skin)
Medical Management (current best evidence)
Clinical trials to learn how to use radiation therapy more safely and effectively are being conducted by doctors and scientists. [3]
Working on improving image-guided radiation. [3]
Research is also being done on radiosensitizers and radioprotectors. [3]
The use of carbon ion beams is still being investigated and remain experimental. This type of therapy are not currently available in the US. [3]
Treatment of Common Clinical Syndromes associated with RFS[2]
These treatments are usually used in conjunction with physical therapy or after conservative/rehabilitative treatments have failed
Neck Extensor Weakness – cervical orthotics, nerve stabilizing medications such as pregabalin, gabapentin or duloxetine, and local anesthetic injection into tender points
Shoulder Pain and Dystonia – anti-inflammatory and/or nerve stabilizing medications and subacromial injection with steroids and anesthetic
Cervical Dystonia – nerve stabilizing medications, opiods and botulinum toxin injections
Trismus – forced mouth opening under general anesthetic for short-term effects, surgical coronoidectomy, botulinum toxin injection and jaw opening devices
Physical Therapy Management (current best evidence)
Physical therapists should always wash their hands before treating a patient who has undergone radiation therapy to protect that client from possible infection.[5]
Skin Care[5] – Avoid use of alcohol/drying agents, lotion, gel, or oil. Creams and gels can increase the dosage received on the skin and increase the likelihood of side effects
– Do not wash away markings of the targeted area
– Position the patient so they are not lying on the targeted area
– Avoid exposing the patient to sources of heat, including direct sunlight and modalities
– Monitor wound healing
Musculoskeletal [5]
– If adhesions are present in the hip after radiation of the pelvis, be sure to incorporate range of motion activities; early intervention is important to prevent contractures and restrictive scarring.
– Post-radiated tissue can tear when stretching so it is important to observe for blanching of the skin during stretching and not to stretch beyond that point. Stretching should be continued 18 to 24 months after radiation therapy has been discontinued.
Nervous System [5]
– Anyone with neurological signs or symptoms of an unknown cause should be asked about a previous history or cancer and radiation therapy
Infection[5] – Therapists should observe carefully for signs of infection in patients who have undergone radiation treatment. The first and only sign may be a fever because the patient may be immunosuppressed and their body cannot create a normal inflammatory response. Exercise [5] – A successful protocol should include patient education, exercise evaluation and an individualized exercise prescription. – Therapists must monitor vital signs in patients who have undergone radiation treatment because radiation and chemotherapy can leave the lungs and heart tissue permanently scarred.
– Patients should be taught to monitor their own vitals including heart rate, respiration rate and rate of perceived exertion (should not exceed 15 to 17) and taught to detect signs of complications such as dyspnea, pallor, excessive perspiration, or fatigue while exercising. Patients should be told not to exercise within 2 hours of chemotherapy or radiation therapy because it increases the circulation and may increase the effects of the treatment.
– Studies have shown low to moderate intensity aerobic exercise during the same weeks of radiation treatment can help improve physical function and lower subjective levels of fatigue, anxiety, depression and sleep disturbances.
Lymphedema [7]
• Exercise has a different effect on the body at lower doses than it does at higher doses
• Extreme exercise would promote inflammation and injury and should be avoided
• Slowly, progressive, carefully controlled increases in stress on a limb may actually provide protection
• Individuals at risk and with lymphedema should be evaluated by a certified lymphedema therapist
Management of Syndromes Associated with Radiation Fibrosis Syndrome[2]
Physical Therapy is usually the first line of treatment for the dysfunctions listed below.
Neck Extensor Weakness – emphasize postural retraining through core strengthening, flexibility of the shoulder musculature, and strengthening the cervicothoracic and rotator cuff muscles. This will help reduce energy demands and pain. It is also important to develop a long-term home exercise program.
Shoulder Pain and Dystonia – treated through conservative measures because shoulder surgery should be avoided in patients with RFS because damage of the neruomuscular structures often results in poor surgical outcomes. Work on core strength and posture, neck extensor and rotator cuff strength and stretching of pectoral girdle musculature in order to try to restore normal anatomical alignment of the shoulders. There is a potential long-term benefit if the patient consistently follows a home exercise program.
Cervical Dystonia – the goal is to restore and maintain neck range of motion and a long-term home exercise program should be utilized.
Trismus – Literature is limited but a variety of jaw-opening devices are available to help treat trismus.
Differential Diagnosis
Lymphedema
| Disorder | Definition | Signs and Symptoms |
| Deep Vein Thrombosis[10] | -Blood clot in the leg. | -Tenderness -Leg pain -Swelling (Difference of 1.4 cm in men and 1.2 cm in women) -Warmth -Subcutaneous venous distension -Discoloration |
| Hypoalbuminemia[11][12] | -Low level of albumin (serum-binding protein). -Common problem among persons with acute and chronic medical conditions |
-Swelling -Loss of appetite -Muscle weakness, fatigue, cramps -Pleural effusion -Ascites |
| Renal Failure[13] | -Failing of the kidneys. | -Decreased urine output -Fluid retention, swelling -Fatigue -Confusion -Nausea |
| Lipedema[5] | -Symmetrical swelling of both legs, extending from the hips to the ankles caused by deposits of subcutaneous adipose tissue. | -Fatty bulges in the medial proximal thigh and the medial distal thigh just above the knee -Feet not affected -Pitting edema relieved by prolonged elevation |
| Baker Cyst[5] | -Subtype of ganglion that often communicates with a joint space. -Most often palpated behind the knee. | -Rupture of the cyst or hemorrhage from the joint into the cyst causes severe pain -Swelling below the lesion. |
| Idiopathic Edema[14] | -Syndrome of real or perceived excessive weight gain. | -Bloating and swelling -Decreased blood volume -Edema around the eyes |
| Congestive Heart Failure[10] |
-Physiologic state in which the heart is unable to pump enough blood to meet the metabolic needs of the body at rest or during exercise. -Also called cardiac decompensation or cardiac insufficiency. |
Left Ventricular Failure Right Ventricular Heart Failure Diastolic Heart Failure -Orthopnea |
| Neurofibromatosis[5] | -Involves the nervous system, muscles, bones, and skin. | -Characterized by multiple soft tumors over the entire body associated with areas of pigmentation. |
| Erysipelas[5] | -Type of cellulitis that may cause an acute infection of the skin with sharply defined borders. | -Accompanied by fever and chills -Very red skin -Shiny skin -Swelling -Warmth -Red streaks extending from the patch indicate lymph vessels involved -Develops over a few hours -Blisters may form after 2-3 days |
| Filariasis[5] | -Parasitic infection carried by mosquitoes. Most damaged occurs after the larva injected has died (approximately 5-10 years later). | -Severe local inflammatory reactions leading to severe fibrosis and scarring -Massive swelling response |
| Thrombophlebitis[15] | Blood clot causing swelling in one or more veins, typically in legs. | -Warmth -Tenderness -Swelling -Pain -Redness |
Radiation Fibrosis Syndrome[2]
When it involves localized muscle pain patients can be misdiagnosed with fibromyalgia or a rheumatic disorder.
Radiation Pneumonitis[5]
Can resemble an underlying lung disease such as COPD.
Radiation-Induced Brachial Plexopathy[16]
Can resemble other neurological problems and must be differentiated from brachial neuritis, carpal tunnel syndrome, cervical disc disease, cervical myofascial pain, and brachial plexopathy caused by trauma or a secondary tumor.
Case Reports/ Case Studies
Nozu T, Yoshida Y, Ohira M, Okumura T. Severe hyponatremia in association with I(131) therapy in a patient with metastatic thyroid cancer. Intern Med. 2011;50(19):2169-74. DOI: 10.2169/internalmedicine.50.5740
Abstract
Hyponatremia is a common clinical problem that results from various causes. Hypothyroidism is known to be one of the causes of this disorder. We report a case of metastatic thyroid cancer presenting with severe hyponatremia in association with hypothyroidism induced by pretreatment of I(131) therapy, such as a low-iodine diet and withdrawal of thyroid hormone. Serum arginine vasopressin (AVP) was elevated and urine osmolality was higher than that of serum. Saline infusion and thyroid hormone replacement normalized serum sodium and AVP. Inappropriate secretion of AVP in hypothyroid state was thought to be one of the causes of this hyponatremia.
Sonawane S, Gadgil N, Margam S. Therapy related myelodysplastic syndrome: a case report and review of literature. Indian J Pathol Microbiol. 2011 Apr-Jun;54(2):371-3. doi: 10.4103/0377-4929.81643.
Abstract
Therapy related myeloid neoplasm is directly related to previous cytotoxic chemotherapy or radiation therapy. We present a 47-year-old lady who developed therapy related myelodysplastic syndrome (MDS) 2.5 years after she received four cycles of chemotherapy and local radiation therapy for carcinoma breast. She presented with bicytopenia with trilineage dyspoiesis in the peripheral blood, bone marrow aspirate and biopsy. Fluorescent in-situ hybridization studies did not reveal any of the common abnormalities associated with MDS. A diagnosis of therapy related MDS was rendered. Different studies have shown that patients treated with alkylating agents and ionizing radiation present as MDS with a latent period of 3-10 years. Our patient developed MDS within 2.5 years of starting chemotherapy and radiotherapy and did not reveal any of the conventional cytogenetic abnormalities. It highlights the importance of simple tests like a complete blood count and peripheral blood smear examination in follow-up of the patients treated with chemotherapy.
Fibrosis After Proton Beam Therapy for Non-small Cell Lung Cancer. Jpn J Clin Oncol.2012 Oct;42(10):965-9. Accessed April 10, 2013.
Abstract
There have been no reports describing acute exacerbations of idiopathic pulmonary fibrosis after particle radiotherapy for non-small cell lung cancer. The present study describes the case of a 76-year-old Japanese man with squamous cell carcinoma of the lung that relapsed in the left upper lobe 1 year after right upper lobectomy. He had been treated with oral prednisolone 20 mg/day every 2 days for idiopathic pulmonary fibrosis, and the relapsed lung cancer was treated by proton beam therapy, which was expected to cause the least adverse effects on the idiopathic pulmonary fibrosis. Fifteen days after the initiation of proton beam therapy, the idiopathic pulmonary fibrosis exacerbated, centered on the left upper lobe, for which intensive steroid therapy was given. About 3 months later, the acute exacerbation of idiopathic pulmonary fibrosis had improved, and the relapsed lung cancer became undetectable. Clinicians should be aware that an acute exacerbation of idiopathic pulmonary fibrosis may occur even in proton beam therapy, although proton beam therapy appears to be an effective treatment option for patients with idiopathic pulmonary fibrosis.
Resources
Radiation Therapy and You: Support for People with Cancer
http://www.cancer.gov/cancertopics/coping/radiation-therapy-and-you/page1
American Cancer Society
Radiation Side Effects Worksheet
http://www.cancer.org/acs/groups/content/@nho/documents/document/acsq-009503.pdf
Recent Related Research (from Pubmed)
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1FOSZGBm2W2xub: There was a problem during the HTTP request: 422 Unprocessable Entity
References
- ↑ Picture: http://photos2.demandstudios.com/DM-Resize/photos.demandstudios.com/60/210/fotolia_3929119_XS.jpg?h=10000&w=400&keep_ratio=1
- ↑ 2.02.12.22.32.42.5 Stubblefield MD. Radiation Fibrosis Syndrome: Neuromuscular and Musculoskeletal Complications in Cancer Survivors. PM R. 2011;3:1041-1054.
- ↑ 3.03.13.23.33.43.53.63.73.83.9 National Cancer Institute. Radiation Therapy for Cancer. National Institutes of Health. http://www.cancer.gov/cancertopics/factsheet/Therapy/radiation. Reviewed May 30, 2010. Accessed April 3, 2013.
- ↑ Picture: http://www.asbestos.net/diseases/cancer/asbestos-cancer-treatment
- ↑ 5.005.015.025.035.045.055.065.075.085.095.105.115.125.135.145.15 Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis. Missouri: Saunders, 2009.
- ↑ Picture: http://wc1.smartdraw.com/examples/content/examples/10_healthcare/cancer_illustrations/radiation_therapy_side_effects_during_cancer_treatment_l.jpg
- ↑ 7.07.17.2 National Cancer Institute. Lymphedema. National Institutes of Health. http://www.cancer.gov/cancertopics/pdq/supportivecare/lymphedema/healthprofessional/page1. Reviewed May 30, 2011. Accessed April 3, 2013.
- ↑ Zuther, J. (2010, June 3). Complications of Lympedema. Retrieved April 22, 2012, from Livestrong website: http://www.livestrong.com/article/138346-complications-lymphedema/
- ↑ Stubblefield MD. Radiation Fibrosis Syndrome: What It Is And How To Treat It [Internet]. Houston, Texas: Cancer Forward The Foundation for Cancer Survivors; 2010. Available from: http://www.cancerforward.org/survivor-resources/experts-speak/Michael-D-Stubblefield-MD/radiation-fibrosis-syndrome-what-it-is-and-how-to-treat-it.
- ↑ 10.010.1 Goodman C and Snyder T. Differential Diagnosis for Physical Therapy: SCREENING FOR REFERRAL. 5th edition. Missouri: Elsevier Saunders; 2013.
- ↑ Shifko R. Livestrong (Internet). Demand Media, Inc; 2010, September 24 (Cited 2013, April 22). Available from: http://www.livestrong.com/article/257967-side-effects-of-hypoalbuminemia/
- ↑ Peralta R and Rubery B. Medscape Reference (Internet). WebMD LLC; Update 2012, July 30 (Cited 2013, April 22). Available from: http://emedicine.medscape.com/article/166724-clinical#a0217
- ↑ Mayo Clinic. Mayo Foundation for Medical Education and Research (Internet); 1998 (Updated 2012, August 10; Cited 2013 April 22). Available from: http://www.mayoclinic.com/health/kidney-failure/DS00280/DSECTION=symptoms
- ↑ Cunha J. MedicineNet (Internet). 1996 (Cited 2013, April 22). Available from: http://www.medicinenet.com/edema/page6.htm
- ↑ Mayo Clinic. Mayo Foundation for Medical Education and Research (Internet); 1998 (Cited 2013 April 22). Available from: http://www.mayoclinic.com/health/thrombophlebitis/DS00223/DSECTION=symptoms
- ↑ Stephenson RO. Radiation-Induced Brachial Plexopathy Differential Diagnosis [Internet]. Medscape; Updated Mar 26, 2013. Available from: http://emedicine.medscape.com/article/316497-differential.