Definition/Description
Rhizomelic chondrodysplasia punctata (RCDP) is a rare disorder found in infants from genetic origin. It is caused by deficient activity of peroxisomal enzymes. In patients with RCDP, their bodies cannot synthesize plasmalogens due to a deficiency of acyl-CoA. Another biochemical characteristic of RCDP is high levels of phytanic acid in the body. The severity of the decreased plasmalogens corresponds with the severity of the disease and abnormalities seen on MRI of the brain. Also, the patients with the milder phenotype have significantly higher levels of plasmalogens in erythrocytes.[1]
There are 3 genetic subtypes. Type 1 consists of individuals with homozygous or compound heterozygous mutations in the PEX7 gene. This is the largest group. Type 2 is secondary to mutations in the GNPAT gene. Type 3 forms by mutations in the AGPS gene. Life expectancy is considerably reduced.[1][2]
Prevalence
Estimated 1 in 100,000; RCDP 1 is most common subtype. [1]
Characteristics/Clinical Presentation
These patients present with severe and symmetrical shortening of the proximal long bones (rhizomelia), calcifications in cartilage with epiphyseal and metaphyseal abnormalities, bilateral cataracts, spasticity, and severe growth and psychomotor delays. Also it is common to see congenital contractures, and dysmorphic facial characteristics. Often born with birth weight, length, and head circumference lower than normal. [1][2][3]
Associated Co-morbidities
- Epilepsy
- Bilateral cortical cataracts
- Congenital heart defects
- Pulmonary hypoplasia
- Recurrent respiratory tract infections
- Contractures
- Cerebral and cerebellar atrophy with enlargement of the ventricles and CSF spaces
- Ureteropelvic junction obstruction
- G-tubes common due to aspiration and inadequate nutrition[1][3][4]
Medications
- Due to the severity of respiratory problems individuals with RCDP require the influenza vaccine and RSV monoclonal antibody.
- There has been no systematic study for oral plasmalogen supplementation to determine clinical benefits. [3]
Diagnostic Tests/Lab Tests/Lab Values
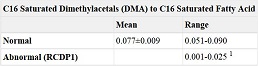
Diagnosis is based on biochemical or molecular genetic testing. Diagnostic tests for RCDP include biochemical and molecular genetic tests as well as based on clinical findings. Biochemical testing pertains to looking at peroxisome function and includes a deficit in red blood cell concentration of plasmalogens (Table 1) and increased phytanic acid (Table 2) and normal very long chain fatty acid concentration in the plasma. The combination of these three findings have shown to predict a defect in the PEX7 receptor.[3]
Table 1.
Values for Red Blood Cell Plasmalogens. [3]
Table 2.
Plasma Concentration of Phytanic Acid. [3]
Molecular genetic testing is also conducted looking for the sequence that encodes for the gene PEX7. This is the only known variant causing RCDP1. Similarly for all other types, the genetic codes are identified for those mutant genes.
These findings, in combination with the specific clinical presentation, leads to the diagnosis of rhizomelic chondrodysplasia punctata.[3]
Etiology/Causes
Genetic mutations of three genes mentioned above, which leads to peroxisome biogenesis disorders.
Systemic Involvement
Multiple systems are affected by this disorder.[1][3]
- The skeletal system is affected by the proximal shortening of the long bones, contractures, stiff and painful joints, and the calcifications in the cartilage at multiple joints.
- The vestibular system is affected by cataracts that are sometimes congenital and sometimes develop within the first few years.
- The nervous system is affected by seizures, delayed development, and spasticity
- The muscular system is also affected by spasticity, contractures, calcifications, and the proximal shortening of the long bones.
- The respiratory system is often later affected and respiratory complications are the most common cause of death patients with RCDP. Recurrent respiratory tract infections are common due to neurological causes, aspiration, immobility, and a small chest with limited excursion.
- The urinary system can also be affected due to the ureteropelvic junction obstruction, which occurs when the junction of the kidney and the ureter is blocked.
Medical Management (current best evidence)
- Management is mostly used as supportive and not corrective because of the poor outcome associated with the diagnosis of RCDP. Management is also limited because of the severe handicaps present from birth throughout the lifespan.
- Some orthopedic procedures have improved function for some individuals with RCDP.
- Cataract extraction may be able to allow patient to maintain some use of vision.
- Gastrostomy tubes are commonly placed for feeding to prevent recurrent aspiration
- Supplemental Oxygen is also commonly necessary
- Genetic counseling to help families of patients with RCDP
- Dietary restriction of phytanic acid may be helpful over time for these individuals
- Possible oral supplementation of DHA (docosahexaenoic acid)[3]
Physical Therapy Management (current best evidence)
Evidence is limited in physical therapy treatment of Rhizomelic Chondrodysplasia Punctata due to its rarity and individuals short life span.
But, physical therapy treatment is recommended for those with RCDP. The main goals for physical therapy are to prevent secondary impairments of RCDP.[3]
- Improve contractures related to RCDP
- Prevention of respiratory complications
- Management of spasticity
- Provide cognitive stimulation
- Can also be a referral source for orthopedic procedures and family support
- Can help to improve quality of life
Differential Diagnosis
There are few disorders that have similar physical manifestations to RCDP.
X-linked recessive chondrodysplasia punctata is similar by having underdevelopment in the distal phalanges but there’s no other signs of limb shortening and no cataracts, unlike RCDP. Differentially diagnosing this x-linked disorder from RCDP is confirmed through genetic testing. It is related to defects in the arylsofatase E (ARSE) gene.
X-linked dominant chondrodysplasia punctata, also known as Condradi-Hünermann syndrome, presents with similar, but asymmetric, limb shortening and sectorial cataracts. The diagnosis for this syndrome as opposed to RCDP is done by looking at the concentration of sterols in the plasma. Through this a diagnosis of Condradi-Hünermann syndrome shows an accumulation of the precursors 8(9)-cholesterol and 8-dehydrocholesterol.
There also the tibia-metacarpal and humero-metacarpal types of chodrodysplasia punctata. These are inherited autosomal-dominantly but it is still unknown through which gene mutation. These individuals have shortening in their metacarpal bones and shortening of long bones- dependent on which disease. Unlike RCDP, these individuals do not have cataracts or skin changes.[3]
Case Reports/ Case Studies
1. Karabayır N, Keskindemirci G, Adal E, Korkmaz O. A Case of Rhizomelic Chondrodysplasia Punctata in Newborn. Case Reports In Medicine [serial online]. January 2014;:1-3. Available from: Academic Search Complete, Ipswich, MA. Accessed April 9, 2016.
Resources
References