Definition/Description
Medial Tibial Stress Syndrome (MTSS) or Shin-Splint Syndrome is a clinical pain condition [1] defined as exercise-induced pain along the posteromedial tibial border (distal third) caused by repetitive loading stress during running and jumping[2]and provoked on palpation over a length of ≥5consecutive centimeters. [1][2][3]
The American Medical Association (AMA) defined as ‘Pain and discomfort in the leg from repetitive running on hard surfaces or forcible, excessive use of the foot flexors‘ [4] in The Standard Nomenclature of Athletic Injuries
Another proposed terminology is that described by Bruckner and Kahn, “A more descriptive term that explains the inflammatory traction event in the tibial aspect of the common leg in the runners is the medial periostitis of the tibial traction or simply the tibial periostitis medial”[5]
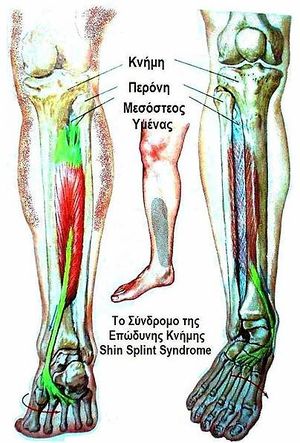
Clinically Relevant Anatomy
The pathophysiology of shin splints is more easily understood after examining the relevant cross-sectional anatomy. There are 4 muscle compartments in the leg:
- Anterior: this compartiment contains the tibialis anterior muscle, the extensor hallucis longus, the extensor digitorum longus and the peroneus tertius.
- The tibialis anterior dorsiflexes the ankle and inverts the foot.
- The extensor hallucis longus extends the great toe
- The extensor digitorum longus extends the other toes and assists in eversion as does the peroneus tertius.
- B) Deep posterior: this contains the flexor digitorum longus, the tibialis posterior and the flexor hallucis longus.
- The tibialis posterior plantar flexes and inverts the foot.
- The others are predominantly toe flexors.
- C) Superficial posterior: this is the gastrocnemius and soleus group; predominatly plantar flexors of the ankle.
- D) Lateral: this compartment contains the peroneus brevis and longus, mainly foot evertors[3]
A dysfunction of tibialis anterior and posterior are commonly implicated, also the area of attachment of these muscles can be the location of pain. [2] Muscle imbalance and inflexibility, especially tightness of the triceps surae (gastrocnemius, soleus, and plantaris muscles), is commonly associated with MTSS . Athletes with muscle weakness of the triceps surae are more prone to muscle fatigue, leading to altered running mechanics, and strain on the tibia. Clinicians should also examine for inflexibility and imbalance of the hamstring and quadriceps muscles. [3]
Epidemiology /Etiology
Shin splint is a common overuse sports injury with incidence rates from 4% to 19% in athletic populations and 4% to 35% of military population.[6]
In runners (sprinters, middle and long distance runners and footballers)[4] has been identified as the most common-related musculoskeletal injury with an incidence rate ranging from 13.6% to 20.0% and a prevalence of 9.5%. Also in dancers it is present in 20% of the population and up to 35% of the new recruits of runners and dancers will develop it[4]
Shin-splints is most common with running and jumping athletes who made training errors, especially when they overload or when they run too fast for their potential. This injury can also be related to changes in the training program, such as an increase in distance, intensity and duration.[3] Running on a hard or uneven surface and bad running shoes (like a poor shock absorbing capacity) could be one of the factors related to the casualty. Biomechanical abnormalities as foot arch abnormalities, hyperpronation of the foot, unequal leg length,..[7] are the most frequently mentioned intrinsic factors.
Women have an increased risk to incur stress fractures, especially with this syndrome. This is due to nutrional, hormonal and biomechanical abnormalities. Individuals who are overweight are more susceptible to getting this syndrome. Therefore it is important that people who are overweight, combine their exercise with a diet or try to lose weight before starting therapy or a training program. These people, along with poor conditioned individuals, should always slowly increase their training level. Cold weather contributes to this symptom, therefore it’s important (even more than usual) to warm up properly.
The pathophysiology is unclear but there are two hypothesis for discussion: periostitis induced by fascial traction or a local bone stress reaction.[4] Internally a chronic inflammation of the muscular attachment along the posterior medial tibia and bony changes are considered to be the most likely cause of the medial tibial stress syndrome.[8]
Characteristics/Clinical Presentation
The main symptom is dull pain at the distal two third of the posteromedial tibial border. The pain is non-focal but extends over “at least 5 cm” [4] and is often bilateral[9].It also worsens at each moment of contact.[7] A mild edema in this painful area may also be present and tenderness on palpation is typically present following the inducing activity for up to several days.[4]
At first the patient only feels pain at the beginning of the workout, often disappearing while exercising, only to return during the cool-down period. When shin splints get worse the pain can remain during exercise and also could be present for hours of days after cessation of the inducing activity.[4]
The most common complication of shin-splints is a stress fracture, which shows itself by tenderness of the anterior tibia.[3] Neurovascular signs and symptoms are not commonly attributable to MTSS and when present, other pathologies such as chronic exertional compartment syndrome (CECS) or vascular deficiencies should be considered as the source of leg pain.[10][11][7]
Differential Diagnosis
An algorithmic approach has been established for further differentiating exercise-induced leg pain entities[4]:
- Pain at rest with palpable tenderness indicates bone stress injuries (MTSS and stress fractures),
- No pain at rest with palpable tenderness proposes nerve entrapment syndromes
- No pain at rest with no palpable tenderness makes functional popliteal artery entrapment syndrome and chronic exertional compartment syndrome likely
MTSS may overlap with the diagnosis of deep posterior compartment syndrome but the critical point for differentiation is the longer lasting post-exercise pain when compared with deep posterior chronic exertional compartment syndrome.
Compared with stress fractures, the painful area extends over more than 5 cm on the distal two thirds of the medial tibial border.
| KEY POINTS FOR ASSESSMENT AND MANAGEMENT FOR MTSS[4] | |
|---|---|
| HISTORY | Increasing pain during exercise related to the medial tibial border in the middle and lower third
Pain persists for hours or days after cessation of activity |
| PHYSICAL EXAMINATION | Intensive tenderness of the involved medial tibial border
More than 5 cm |
| IMAGING | MRI: Periosteal reaction and edema |
| TREATMENT | Mainly conservative (running retraining, ESWT) |
It is important to differentiate MTSS from:
- Stress Fracture
- Chronic Exertional Compartmental Syndrome
- Sciatica
- Deep Vein Thrombosis (DVT)
- Popliteal Artery Entrapment
- Muscle Strain
- Tumour
- Arterial endofibrosis
- Infection
- Nerve entrapment (common/superficial peroneus and saphenous)
The following are two conditions that are sometimes mistakenly diagnosed as shin splints.
Pain on the anterior (outside) part of the lower leg may be compartment syndrome: Swelling of muscles within a closed compartment which creates pressure. The symptoms of compartment syndrome include leg pain, unusual nerve sensations, and eventually muscle weakness.
Pain in the lower leg could also be a stress fracture (an incomplete crack in the bone), which is a far more serious injury than shin splints. The pain of a stress fracture is focal with tenderness in less than 5 cm. that can be find with a fingerprint as a definite spot of sharp pain. Additionally, stress fractures often feel better in the morning because the bone has rested all night; shin splints often feel worse in the morning because the soft tissue tightens overnight. Shin splints are also at their most painful when patient forcibly try to lift the foot up at the ankle and flex the foot. [10]
Diagnostic Procedures
Making the diagnosis based on history and physical examination is the most logical approach.[1][2]
- A standardised history include questions on the onset and location of the pain:
- If there is exercise-induced pain along the distal 2/3 of the medial tibial border: MTSS diagnosis is suspected
- The athlete is asked of what aggravated and relieved their pain: If pain is provoked during or after physical activity and reduced with relative rest, MTSS diagnosis is suspected
- The athlete is asked about cramping, burning and pressure-like calf pain and/or pins and needles in the foot (their presence could be signs of chronic exertional compartment syndrome, which could be a concurrent injury or the sole explanation for their pain): If no present, MTSS diagnosis is suspected
- Physical examination If MTSS is suspected after the history: the posteromedial tibial border is palpated and the athletes are asked for the presence of recognisable pain (ie, from painful activities).
- If no pain on palpation is present, or the pain is palpated over less than 5 cm: other lower leg injuries (eg, a stress fracture) has to be considered to be present and the athlete is labelled as not having MTSS
- If other symptoms not typical of MTSS are present (severe and visible swelling or erythema along the medial border): other leg injury should be considered
- If recognisable pain is present on palpation over 5 cm or more and no atypical symptoms are present, the diagnosis MTSS is confirmed.
Detmer in 1986 developed a classification system to subdivide MTSS into three types: [11]
- Type I – tibial microfracture, bone stress reaction or cortical fracture
- Type II – periostalgia from chronic avulsion of the periosteum at the perios teal-fascial junction
- Type lll – chronic compartment syndrome.
Imaging studies are not necessary to diagnose shin-splints, but when a conservative treatment fails, it could be useful to undertake an echo. If the injury has evolved into a stress fracture, an x-ray scan can show black lines. A triple-phase bone scan can show the difference between a stress fracture and a medial tibial stress syndrome.[7] The MRI can also exclude tumors/edemas.[7]
It is important that clinicians be aware that about 1/3 (32%) of the athletes with MTSS have co-existing lower leg injuries[4]
Outcome Measures
The MTSS score should be used as a primary outcome measure in MTSS because is valid, reliable and responsive. It measures:[1]
- Pain at rest
- Pain while performing activities of daily living
- Limitations in sporting activities
- Pain while performing sporting activities.
The MTSS score specifically measures pain along the shin and limitations due to shin pain.
Examination
Examination demonstrates an intensive tenderness on palpation along the medial tibial border, the anterior tibia, however, is usually nontender. Neurovascular symptoms are usually absent. Different from stress fracture, the pain is not focused to a specific point but covers a variable distance of several centimeters in the distal medial and proximal distal third of the tibia.[4] In the painful area, there is no real muscle origin, but the deep crural fascia is attached to the medial tibial border. From clinical experience, a painful transverse band can frequently be palpated which most probably corresponds to the soleal aponeurosis .Therefore, MTSS is currently hypothesized to originate from tibial bone overload and not from adjacent soft tissue stress[4]
Physicians should carefully evaluate for possible knee abnormalities (especially genu varus or valgus), tibial torsion, femoral anteversion, foot arch abnormalities, or a leg-length discrepancy. Ankle movements and subtalar motion should also be evaluated. Clinicians should also examine for inflexibility and imbalance of the hamstring and quadriceps muscles and weakness of “core muscles”. Core and pelvic muscle stability may be assessed by evaluating patient’s ability to maintain a controlled, level pelvis during a pelvic bridge from the supine position, or a standing single-leg knee bend.
Examining patient’s shoes may reveal generally worn-out shoes or patterns consistent with a leg-length discrepancy or other biomechanical abnormalities.
Abnormal gait patterns should be evaluated with the patient walking and running on a treadmill. [11][12][13][14][15][3][16][17][18][19][20][21][22]
Medical Management
Treatment is predominantly conservative and there is no treatment proven to be effective for athletes. Therefore, temporary reduction or even cessation of the provoking activity is most frequently the initial response of the athlete and trainer alike to reduce the symptoms.[4]
Treatment options include ultrasound, extracorporeal shockwave therapy, and steroid injections. Schulze et al looked at various treatment options from application of local and systemic anti-inflammatory medicaments to physiotherapy with ultrasound, phonophoresis, and local friction. However, they concluded none of these methods has proven to be superior to the others. [23]
Surgical treatment is rarely needed. It is indicated in the athlete who has failed one year’s conservative treatment or in whom the condition is recurrent (two or more times). The surgical procedure consists in a deep posterior fascia release, to relieve tension or pressure commonly to treat the resulting loss of circulation, The described technique is an open procedure with fasciotomy by doing one or more incisions, of the deep posterior compartment, release of the ‘soleus bridge’, and resection of a periosteal strip from the involved medial tibia.[4]
35% and 34% had an excellent and good result while 22% and 9% were fair and poor respectively and only “41% of the athletes fully returned to their presymptom sports activity”[4]
Postoperatively patients must follow a graded rehabilitation program similar to that used in non-operative treatment. [24][25]
Physical Therapy Management
Patient education and a graded loading exposure program seem the most logical treatments.[1] Conservative therapy should initially aim to correct functional, gait, and biomechanical overload factors.[4]Recently ‘running retraining’ has been advocated as a promising treatment strategy and graded running programme has been suggested as a gradual tissue-loading intervention.[4]
Prevention of MTSS was investigated in few studies and shock-absorbing insoles, pronation control insoles, and graduated running programs were advocated.[4]
Overstress avoidance is the main preventive measure of MTSS or shin-splints. The main goals of shin-splints treatment are pain relieve and return to pain‑free activities.[26]
For the treatment of shin-splints it’s important to screen the risk factors, this makes it easier to make a diagnosis and to prevent this disease. In the next table you can find them.[27] (Level of Evidence: 1a)
| Intrinsic factors | Extrinsic factors |
| Age Sex Height Weight Body fat Femoral neck anteversion Genu valgus Pes clavus Hyperpronation Joint laxity Aerobic endurance/conditioning Fatigue Strength of and balance between flexors and extensors Flexibility of muscles/joints Sporting skill/coordination Physiological factors |
Sports-related factors Type of sport Exposure (e.g., running on one side of the road) Nature of event (e.g., running on hills) Equipment Shoe/surface interface Venue/supervision Playing surface Safety measures Weather conditions Temperature |
Control of risk factors could be a relevant strategy to initially avoid and treat MTSS: MIO2
- Female gender
- Previous history of MTSS
- Fewer years of running experience
- Orthotic use
- Increased body mass index
- Pronated foot posture (increased navicular drop)
- Increased ankle plantarflexion
- Increased hip external rotation
The role of hip internal rotation motion is unclear. Differences between hip muscle performance in MTSS and control subjects might be the effect rather than the cause MIO2
Acute phase
2-6 weeks of rest combined with medication is recommended to improve the symptoms and for a quick and safe return after a period of rest. NSAIDs and Acetaminophen are often used for analgesia. Also cryotherapy with Ice-packs and eventually analgesic gels can be used after exercise for a period of 20 minutes.
There are a number of physical therapy modalities to use in the acute phase but there is no proof that these therapies such as ultrasound, soft tissue mobilization, electrical stimulation[12] would be effective.[3] A corticoid injection is contraindicated because this can give a worse sense of health. Because the healthy tissue is also treated. A corticoid injection is given to reduce the pain, but only in connection with rest.[7]
Prolonged rest is not ideal for an athlete
Subacute phase
The treatment should aim to modify training conditions and to address eventual biomechanical abnormalities. Change of training conditions could be decreased running distance, intensity and frequency and intensity by 50%. It is advised to avoid hills and uneven surfaces.
During the rehabilitation period the patient can do low impact and cross-training exercises (like running on a hydro-gym machine).). After a few weeks athletes may slowly increase training intensity and duration and add sport-specific activities, and hill running to their rehabilitation program as long as they remain pain-free.
A stretching and strengthening (eccentric) calf exercise program can be introduced to prevent muscle fatigue. [17][28][29] (Level of Evidence: 3a) (Level of Evidence: 3a) (Level of Evidence: 5). Patients may also benefit from strengthening core hip muscles. Developing core stability with strong abdominal, gluteal, and hip muscles can improve running mechanics and prevent lower-extremity overuse injuries. [29]
Proprioceptive balance training is crucial in neuromuscular education. This can be done with a one-legged stand or balance board. Improved proprioception will increase the efficiency of joint and postural-stabilizing muscles and help the body react to running surface incongruities, also key in preventing re-injury.[29]
Choossing good shoes with good shock absorption can help to prevent a new or re-injury. Therefore it is important to change the athlete’s shoes every 250-500 miles, a distance at which most shoes lose up to 40% of their shock-absorbing capabilities.
In case of biomechanical problems of the foot may individuals benefit from orthotics. An over-the-counter orthosis (flexible or semi-rigid) can help with excessive foot pronation and pes planus. A cast or a pneumatic brace can be necessary in severe cases.[3]
Manual therapy can be used to control several biomechanical abnormalities of the spine, sacro-illiacal joint and various muscle imbalances. They are often used to prevent relapsing to the old injury.
There is also acupuncture, ultrasound therapy injections and extracorporeal shock-wave therapy but their efficiency is not yet proved.
Clinical Bottom Line
‘Shin splints’ is a vague term that implicates pain and discomfort in the lower leg, caused by repetitive loading stress. There can be all sorts of causes to this pathology according to different researches. Therefore, a good knowledge of the anatomy is always important, but it’s also important you know the other disorders of the lower leg to rule out other possibilities, which makes it easier to understand what’s going wrong. Also a detailed screening of known’s risk factors, intrinsic as well as extrinsic, to recognize factors that could add to the cause of the condition and address these problems.
References
- ↑ 1.01.11.21.31.4 Winters, M. Medial tibial stress syndrome: diagnosis, treatment and outcome assessment (PhD Academy Award). Br J Sports Med. 2018
- ↑ 2.02.12.22.3 Thacker, S. B., Gilchrist, J., Stroup, D. F., & Kimsey, C. D. The prevention of shin splints in sports: a systematic review of literature. Medicine & Science in Sports & Exercise. 2002; 34(1): 32-40.
- ↑ 3.03.13.23.33.43.53.63.7 Galbraith, R. M., & Lavallee, M. E. ↑ 4.004.014.024.034.044.054.064.074.084.094.104.114.124.134.144.154.164.17 Lohrer, H., Malliaropoulos, N., Korakakis, V., & Padhiar, N. Exercise-induced leg pain in athletes: diagnostic, assessment, and management strategies. The Physician and sports medicine. 2018
- ↑ Pietrzak, M. ↑ Winters, M., Bakker, E. W. P., Moen, M. H., Barten, C. C., Teeuwen, R., & Weir, A. Medial tibial stress syndrome can be diagnosed reliably using history and physical examination. Br J Sports Med.2018; 52(19): 1267-1272.
- ↑ 7.07.17.27.37.4 Broos P. Sportletsels : aan het locomotorisch apparaat. Leuven: Garant, 1991. (Level of Evidence: 5)
- ↑ Peterson L, Renström P. Sports Injuries: Their Prevention and Treatment. London: Dunitz. 2001
- ↑ Reid DC. Sports Injury Assessment and Rehabilitation. New York: Churchill Livingstone. 1992
- ↑ 10.010.1 The runner´s world editors. Everything you need to know about shin splints. Available from:↑ 11.011.111.2 Moen, M. H., Tol, J. L., Weir, A., Steunebrink, M., & De Winter, T. C. Medial tibial stress syndrome. Sports medicine. 2009; 39(7): 523-546. (Level of evidence 3A)
- ↑ 12.012.1 Beck B. ↑ Kortebein PM, Kaufman KR, Basford JR, Stuart MJ. Medial tibial stress syndrome. Med Sci Sports Exerc 2000;32(3 Suppl):S27-33.(Level of evidence 1A)
- ↑ Wilder R, Seth S. Overuse injuries: tendinopathies, stress fractures, compartment syndrome, and shin splints. Clin Sports Med. 2004;23(1):55-81. (Level of evidence 4)
- ↑ Fredericson M. Common injuries in runners. Diagnosis, rehabilitation and prevention. Sports Med. 1996;21:49–72. (Level of evidence 4)
- ↑ Strakowski J, Jamil T. Management of common running injuries. Phys Med Rehabil Clin N Am. 2006;17(3):537–552.(Level of evidence 2A)
- ↑ 17.017.1 Dugan S, Weber K. Stress fracture and rehabilitation. Phys Med Rehabil Clin N Am. 2007;18(3):401–416. (Level of evidence 3A)
- ↑ Sommer H, Vallentyne S. Effect of foot posture on the incidence of medial tibial stress syndrome. Med Sci Sports Exerc. 1995;27:800–804. (Level of evidence 3A)
- ↑ Niemuth P, Johnson R, Myers M, Thieman T. Hip muscle weakness and overuse injuries in recreational runners. Clin J Sport Med. 2005;15(1):14–21. (Level of evidence 1A)
- ↑ Greenman P. Principles of manual medicine. Philadelphia, PA: Lippincott Williams & Wilkins. 2003;3(11):337–403, 489. . (Level of evidence 1A)
- ↑ Howell J. ↑ Karageanes S. Principles of manual sports medicine. Philadelphia, PA: Lippincott, Williams and Wilkins. 2005: 467–468. Level of evidence 1A)
- ↑ Moen, M. H., Holtslag, L., Bakker, E., Barten, C., Weir, A., Tol, J. L., & Backx, F. T↑ Yates B, Allen MJ, Barnes MR. Outcome of surgical treatment of medial tibial stress syndrome. J Bone Joint Surg Am. 2003;85-A(10):1974-80. (Level of evidence 4)
- ↑ Holen KJ, Engebretsen L, Grontvedt T, Rossvoll I, Hammer S, Stoltz V. Surgical treatment of medial tibial stress syndrome (shin splint) by fasciotomy of the superficial posterior compartment of the leg. Scand J Med Sci Sports. 1995;5(1):40-3. (Level of evidence 1A)
- ↑ Alfayez, S. M., Ahmed, M. L., & Alomar, A. Z. A review article of medial tibial stress syndrome. Journal of Musculoskeletal Surgery and Research. 2017; 1(1): 2. (Level of Evidence: 4)
- ↑ Winkelmann, Z. K., Anderson, D., Games, K. E., & Eberman, L. E. ↑ Couture C, Karlson K. Tibial stress injuries: decisive diagnosis and treatment of ‘shin splints’. Phys Sportsmed. 2002;30(6):29–36.(Level of Evidence: 3a)
- ↑ 29.029.129.2 DeLee J, Drez D, Miller M. DeLee and Drez’s orthopaedic sports medicine principles and practice. Philadelphia, PA: Saunders. 2003:2155–2159.(Level of Evidence: 5)