Definition
Glenohumeral subluxation is defined as a partial or incomplete dislocation that usually stems from changes in the mechanical integrity of the joint. In a subluxation, the humeral head slips out of the glenoid cavity as a result of weakness in the rotator cuff or a blow to the shoulder area. A subluxation can occur in one of three types: anterior (forward), posterior (backward), and inferior (downward). The difference with a shoulder dislocation is the fact that the humeral head pops back into its socket.
Clinically relevant anatomy
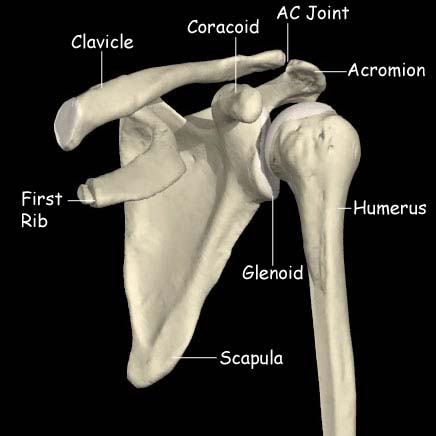
The shoulder joint (or glenohumeral joint) permits the greatest range of motion of any joint. Because it is also the most frequently dislocated joint, it provides an excellent demonstration of the principle that stability must be sacrificed to obtain mobility. It consists of 3 bone structures: humerus, scapula and clavicle. These bones make a total of 3 synovial joints: gleno-humeral , sterno-clavicular and acromio-clavicular joint. Besides these you also find the subacromial “joint” and the scapular-thoracal “joint”. The size of the glenoid cavity is increased by a fibrous cartilaginous glenoid labrum, which continues beyond the bony rim and deepens the socket. The bones of the pectoral girdle provide some stability to the superior surface, because the acromion and coracoid process project laterally superior to the head of the humerus. But most of the stability is provided by the surrounding skeletal muscles, with help from their associated tendons and various ligaments. The major ligaments that help stabilise the shoulder joint are the glenohumeral, coracohumeral, coracoacromial and the acromiohumeral ligaments. The acromioclavicular ligament reinforces the capsule of the acromioclavicular joint and supports the superior surface of the shoulder. The largest ligament is the Glenohumeral ligament, and this is commonly damaged or overstretched in shoulder joint subluxation. [1]. The muscles that move the humerus stabilise the shoulder more than all the ligaments and capsular fibres combined. Muscles originating on the trunk, pectoral girdle and humerus cover the anterior, superior and posterior surfaces of the capsule. The tendons of the supraspinatus, infraspinatus, teres minor and subscapularis reinforce the joint capsule and limit the range of motion. These muscles, known as the rotator cuff, are the primary mechanism for supporting the shoulder joint and limiting its ROM.
Video
Epidemiology
Studies show that there is no relationship between shoulder pain, shoulder subluxation and gender. It equally occurs within men and women.
Shoulder subluxations frequently occur in people with hemiplegic stroke or with a paralysed upper limb. The reported incidence varies greatly, from 17% to 81% [2] [3]
Traumatic subluxations of the shoulder can occur in many sports, including football, rugby, wrestling and boxing.
Characteristics/clinical presentation
The main problem with shoulder subluxation is the instability of the gleno-humeral joint. The anatomy of this joint permits a large range of movement, but it sacrifices stability. Research by Basmajian determined that the musculus supraspinatus and in minor ways also the posterior fibres of the deltoid muscle play a key role in maintaining glenohumeralalignment. Chaco and Wolf, did confirm this in their study, which said that the supra spinatus is very important in preventing the downward subluxation of the humerus. Subluxation occurs with the shoulder in abduction and externally rotation.Other research shows that the most important ligamental structure to maintain correct shoulder position and also to prevent shoulder subluxation is the inferior glenohumeral ligament.This ligament is most important during external rotation and abduction during the cocking face of the throwing motion.
Shoulder subluxation can lead to soft tissue damage as traction damage can occur due to gravitational pull forces and poor protection is offered by a weak shoulder. It is usually quite painful, and there might be a partial numbness of the shoulder, arm and hand.
Differential Diagnosis
Acromioclaviculair joint injury
Biceps tendinopathy
Bicep tendinopathy, is an inflammatory process of the long head of the biceps tendon and is a common cause of shoulder pain due to its position and function.
Clavicular injuries
Although clavicle fractures are common and usually heal regardless of the selected treatment, complications are possible, warranting careful attention to these injuries. Multiple attempts have been made to devise a classification scheme for clavicle fractures. The most common system is the following one, created by Allman, in which the clavicle injuries is divided into thirds:
• Group I fractures: Middle third injuries
• Group II fractures: Distal third injuries
• Group III fractures: Medial (proximal) third injuries
Rotator cuff injury
Shoulder dislocation
Swimmer’s shoulder
Swimmer’s shoulder is the term used to describe the problem of shoulder pain in the competitive swimmer. Swimming is an unusual sport in that the shoulders and upper extremities are used for locomotion, while at the same time requiring above average shoulder flexibility and range of motion (ROM) for maximal efficiency. This is often associated with an undesirable increase in joint laxity. Symptoms: Functional testing: Radiographic measurements are considered to be the most accurate way of evaluating the degree of subluxation[5] Examination
First the examinor should ask the patient about the history of the reason he subluxated his arm. Than he can perform an inspection, when he does he should make sure that he can have a visual on both shoulders at the same time to see the different. In this test the examiner stabilises the scapula and moves the humeral head to posterior and anterior. With this test the examiner can feel if the humeral head is going to subluxate.
The patients arm is placed in 90 degrees of adduction and 30 degrees of forward flexion. With his other hand the examiner grasps the midhumerus and provides posteriorly directed force. This test is used to measure the posterior laxity of the shoulder.
This test is similar to the Load and shift test but the second hand is placed in the axilla to feel for translation of the humeral head or to feel if the humeral head subluxates over the rim.
Traditionally supportive devices, in the form of slings or braces, have been used to manage shoulder subluxation following CVA; the aim being to support the weight of the arm thus preventing/minimising the inferior pull on the humerus and reducing the stretch on the joint capsule. A Cochrane Review [6] in 2009 concluded that there is insufficient evidence to conclude whether supportive devices are of benefit.
In a Cochrane Review [7] Functional Electrical Stimulation was found to bring about improvement in pain-free range of passive humeral lateral rotation and to reduce the severity of glenohumeral subluxation; however there was no significant effect on upper limb motor recovery. -Prevention of reccurance: Clavicular joint
Late stages of rehabilitation of rotator cuff injury include progressive resistive strengthening, proprioception and sport-specific exercises.
Diagnostic Procedures
Patients with shoulder subluxations commonly present with:
The subluxation test is positive = resistance is given, when patient brings arm in throwing stance, in internal rotation direction.
Pain in the ventral capsule indicates a frontal capsule lesion.
Pressure during resistance test on the dorsal part of the humerus can provoke ventral gliding. The result is sudden pain in the shoulder and in a number of cases there is a subluxation to the front. This test can be conducted in different degrees of abduction and with or without the support of the upper arm.
Outcome Measures
After this you could use different tests to test whether the patient had a subluxation of the shoulder:
Physical Therapy Management
In the hemiplegic patient
Sling/support:
Electrical Stimulation:
Advice/Management:
In the non-hemplegic patient
Strengthening exercises to re-establish the strength of the rotator cuff muscles is recommended.
Initial physical therapy interventions may include:
References