Introduction
According to the World Health Organisation a Stroke is defined as an accident to the brain with “rapidly developing clinical signs of focal or global disturbance to cerebral function, with symptoms lasting 24 hours or longer, or leading to death, with no apparent cause other than of vascular origin and includes cerebral infarction, intracerebral hemorrhage, and subarachnoid hemorrhage”.
Epidemiology/Etiology
According to the World Health Organization (WHO), 15 million people suffer stroke worldwide each year. Of these, 5 million die and another 5 million are left permanently disabled.[1] The [2]
Read more about Epidemiology, Incidence and Global Burden of Stroke
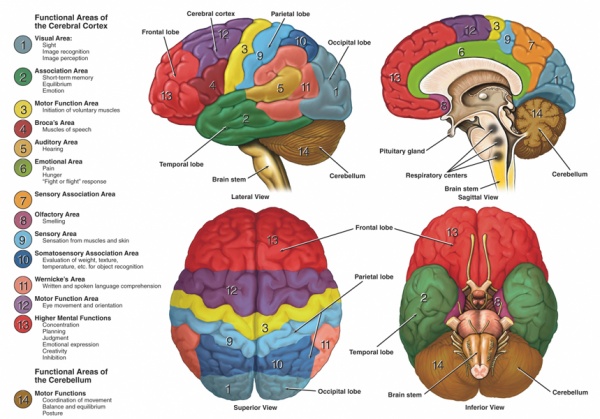
Clinically Relevant Anatomy
At the base of the brain, the carotid and vertebrobasilar arteries form a circle of communicating arteries known as the Circle of Willis. From this circle, other arteries—the anterior cerebral artery (ACA), the middle cerebral artery (MCA) and posterior cerebral artery (PCA)—arise and travel to all parts of the brain.
The image below clearly shows the function areas of the cerebral cortex that can be affected following insufficiency of the blood supply.
Mechanism of Injury / Pathological Process
A stroke occurs when there is interruption of the blood supply to a particular area of the brain, ultimately leading to cell injury and cell death.
Strokes can be classified in two ways:
Ischaemic
Ischaemic strokes are the most common, accounting for up to 80% of strokes, and occur when there is an occlusion of a blood vessel impairing the flow of blood to the brain.
Ischaemic Strokes are divided into:
- Thrombotic – Where a blood clot forms in a main brain artery or within the small blood vessels deep inside the brain. The clot usually forms around atherosclerotic plaques.
- Embolic – A blood clot, air bubble or fat globule forms within a blood vessel elsewhere in the body and is carried to the brain.
- Systemic Hypoperfusion – A general decrease in blood supply, eg. in shock.
- Venous Thrombosis
Haemorrhagic
Haemorrhagic Strokes occur when a blood vessel in the brain ruptures and bleeds.
- Intracerebral Haemorrhagic Stroke — there is bleeding from a blood vessel within the brain. High blood pressure is the main cause of intracerebral haemorrhagic stroke.
- Subarachnoid Haemorrhagic Stroke — there is bleeding from a blood vessel between the surface of the brain and the arachnoid tissues that cover the brain.
Nb. Some experts do not classify Subarachnoid Haemorrhage as Stroke because subarachnoid haemorrhages present differently from Ischaemic Strokes and Intracerebral Haemorrhagic Strokes.
Clinical Presentation
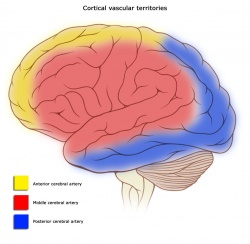
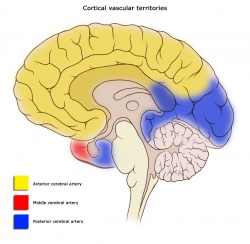
Cortical Areas and their vascular supply:
Location of Infarct & Deficits Produced:
Left MCA Superficial Division
Right face and arm upper-motor weakness due to damage to motor cortex, nonfluent (Broca’s) aphasia due to damage to Broca’s area. There may also be right face and arm cortical type sensory loss if the infarct involves the sensory cortex. Other deficits include a fluent (Wernicke’s) aphasia due to damage to Wernicke’s area. [Aphasia: a disturbance of the comprehension and expression of language]
Right MCA Superficial Division
Left face and arm upper-motor weakness due to damage to motor cortex. Left hemineglect (variable) due to damage to non-dominant association areas. There may also be left face and arm cortical type sensory loss if the infarct involves the sensory cortex.
Left MCA Lenticulostriate Branches
Right pure upper-motor hemiparesis due to damage to the basal ganglia (globus pallidus and striatum) and the genu of the internal capsule on the left side. Larger infarcts extending to the cortex may produce cortical deficits such as aphasia.
Right MCA Lenticulostriate Branches
Left pure upper-motor hemiparesis due to damage to the basal ganglia (globus pallidus and striatum) and the genu of the internal capsule on the right side. Larger infarcts extending to the cortex may produce cortical deficits such aphasia.
Left PCA
Right homonymous hemianopia due to damage to left visual cortex in the occipital lobe. Extension to the the corpus collusom interferes with comunication between the two visual association areas so can cause alexia without agraphia. Larger infarcts involving the internal capsule and thalamus may cause right hemisensory loss and right hemiparesis due to disruption of the ascending and descending information passing through these structures. [Hemoanopia: visual loss in half of the visual field]
Right PCA
Left homonymous hemianopia due to damage to right visual cortex in the occipital lobe. Larger infarcts involving the internal capsule and thalamus may cause left hemisensory loss and left hemiparesis due to disruption of the ascending and descending information passing through these structures.
Left ACA
Right leg upper-motor neuron weakness due to damage to motor cortex and right leg cortical sensory loss due to damage to sensory cortex. Grasp reflex, frontal lobe behavioral abnormalities, and transcortical aphasia can also be seen if the prefrontal cortex and supplemental motor areas are involved.
Right ACA
Left leg upper-motor neuron weakness due to damage to motor cortex and left leg cortical type sensory loss due to damage to sensory cortex. Grasp reflex, frontal lobe behavioural abnormalities and left hemineglect can also be seen if the prefrontal cortex and non-dominant association cortex are involved.
Outcome Measures
Dynamic Gait Index, the 4-item Dynamic Gait Index, and the Functional Gait Assessment show sufficient validity, responsiveness, and reliability for assessment of walking function in patients with stroke undergoing rehabilitation, but the Functional Gait Assessment is recommended for its psychometric properties[7].
Chedoke-McMaster Stroke Assessment
Chedoke Arm and Hand Activity Inventory
CRS-R Coma Recovery Scale Revised is used to assess patients with a disorder of consciousness, commonly coma.
Take a look at our Stroke Outcome Measures Overview for more information
Management / Interventions
Early management of acute stroke: The goal for the acute management of patients with stroke is to stabilize the patient and to complete initial evaluation and assessment, including imaging and laboratory studies, within a short time frame. Critical decisions focus on the need for intubation, blood pressure control, and determination of risk/benefit for thrombolytic intervention.[8]
Patients presenting with Glasgow Coma Scale scores of 8 or less or rapidly decreasing Glasgow Coma Scale scores, require emergent airway control via intubation.
A recent study has showed gait improvement with high-intensity interval training and moderate-intensity continious training in ambualatory chronic stroke patients. Accoridng to the post-stroke guidelines, moderate-intensity, continuous aerobic training (MCT) to improve aerobic capacity and mobility after stroke. High-intensity interval training (HIT) has been shown to be more effective than MCT among healthy adults and people with heart disease.
Physiotherapy
Physiotherapists should be involved early, and should make their own assessment of how much they can work with a patient. Early mobilisation is associated with better outcomes – even after taking account of the potential confounding influence of disease severity. If rehabilitation is to take place on a different ward from acute care, the care received should be made as seamless as possible. Type and intensity of therapy should be determined by the patient’s needs not location.[9]
Primary goals of rehabilitation:
- Prevent complications
- Minimise impairments
- Maximise function
Optimising post stroke rehabilitation:
- early assessment with standardised evaluations and validated assessment tools
- early employment od evidence based interventions relevant to individual patient needs
- patient access to an experienced multidisciplinary rehabilitation team
- ongoing medical management of risk factors and co-morbidities
Upper Limb
Upper Limb Impairments:
- Subluxation
- Changes in Sensation
- Contracture
- Swelling
- Co-ordination Problems
- Weakness
- Altered Muscle Power
- Changes in Muscle Tone
- Hand Dysfunction
Aims of Treatment:
- Prevent shoulder pain and if unable to do so, manage should pain effectively.
- Be selective when choosing compensatory versus remedial intervention methods to treat clients who are predicted to have a low return of motor function and poor functional use of their arm and hand.
- Provide remedially focused rehabilitation to clients who are predicted to change in arm and hand function.
- Use measures of known reliability and evidence of validity for treatment planning and outcome prediction.
In the upper extremity with severe impairment and/or poor prognosis for recovery (Chedoke McMaster Stroke Assessment (CMSA) of Arm and Hand ) treatment should focus on maintaining a comfortable, pain-free, mobile arm and hand[10][11].
- Focus on proper positioning to provide support at rest and careful handling during functional activities
- Participate in classes supervised by professional rehabilitation clinicians in institutional or community setting that teach the client and caregiver to perform self range of motion exercises.
- Avoid use of overhead pulleys (risk of shoulder tissue injury)
- Use some means of external support for stage 1 or 2 upper limb during transfers and mobility
- Place arm and hand in a variety of positions that include placement withing the client’s visual field
- Use some means of external support to protect the upper limb during wheelchair use
In the upper extremity with moderate impairments who show high motivation and potential for functional motor gains (CMSA => stage 4)[10][11]
- Engage in repetitive and intense use of novel tasks that challenge the stroke survivor to acquire necessary motor skills to use the involved upper limb during functional tasks and activities
- Engage in motor-learning training including the use of imagery.
Treatment Techniques:
- Strength Training – There is evidence that strength training can improve upper-limb strength and function without increasing tone or pain in individuals with stroke[12][13].
- Orthotics – therapy incorporating a dynamic wrist-hand orthosis may be no better than manual therapy[14]. Long term use of static orthoses requires complimentary appropriate treatment opportunities to prevent clenched fist, problems with ADL and hygiene maintenance[15]
- Gaming – goal orientated computer gaming has proven to singificantly reduce upper limb impairment in stroke suvivors[16][17]
- Virtual Reality – virtual reality training has been shown to be effective in restoring upper limb motor impairments and motor related functional abilities[18][19]
- Mirror Therapy – Mirror therapy has been shown to have a beneficial effect on motor control and function compared with conventional therapy[20][21][22]
- Robot-Assited Therapy – has been shown to have abeneficial effect on motor recovery and function[23][24][25]
Clinical Guidelines
Overall Management: National clinical guideline for stroke, The Royal College of Physicians, September 2012
Acute Care
Rehabilitation
Differential Diagnosis
- Hypoglycemia and hyperglycemia need to be identified and treated early in the evaluation. Not only can both produce symptoms that mimic ischemic stroke, but they can also aggravate ongoing neuronal ischaemia.
- Hemiplegic Migraine
Resources
Presentations
References
- ↑ Global Burden of Stroke. The Atlas of Heart Disease and Stroke. MacKay J, Mensah GA. World Health Organization.
- ↑ Townsend N, Wickramasinghe K, Bhatnagar P, Smolina K, Nichols M, Leal J, Luengo-Fernandez R, Rayner M (2012). Coronary heart disease statistics 2012 edition. British Heart Foundation: London. P21
- ↑ Cal Shipley, M.D. What Is A Stroke? – Narration and Animation by Cal Shipley, M.D. Available from: http://www.youtube.com/watch?v=uLJewzJcCZ0 [last accessed 10/10/14]
- ↑ USMLEFastTrack. Effects of Strokes – Middle Cerebral Artery. Available from: http://www.youtube.com/watch?v=6sk7AXNw9Ns [last accessed 10/10/14]
- ↑ USMLEFastTrack. Effects of Strokes – Posterior Cerebral Artery. Available from: http://www.youtube.com/watch?v=OFlL9Dm8qCM [last accessed 10/10/14]
- ↑ USMLEFastTrack. Effects of Strokes – Anterior Cerebral & Lateral Striate Artery. Available from: http://www.youtube.com/watch?v=NSWnNnfDt70 [last accessed 10/10/14]
- ↑ Lin JH, Hsu MJ, Hsu HW, Wu HC, Hsieh CL. Psychometric Comparisons of 3 Functional Ambulation Measures for Patients With Stroke. Stroke. 2010 Jul 29; online article ahead of print
- ↑ Adams H, Adams R, Del Zoppo G, Goldstein LB. Guidelines for the early management of patients with ischemic stroke: 2005 guidelines update a scientific statement from the Stroke Council of the American Heart Association/American Stroke Association. Stroke. Apr 2005;36(4):916-23.
- ↑ Harwood R, Huwez F, Good D. Stroke Care: A practical manual. New York: Oxford, 2011.
- ↑ 10.010.1 Norine Foley, Swati Mehta, Jeffrey Jutai, Elizabeth Staines, Robert Teasell. Upper Extremity Interventions. EBRSR, 2013
- ↑ 11.011.1 Susan Barreca et al. Management of the Post Stroke Hemiplegic Arm and Hand: Treatment: Recommendations of the 2001 Consensus Panel. Heart and Stroke Foundation of Ontario, 2001.
- ↑ Carolynn Patten, Elizabeth G Condliffe, Christine A Dairaghi5 and Peter S Lum. Concurrent neuromechanical and functional gains following upper-extremity power training post-stroke. Journal of NeuroEngineering and Rehabilitation 2013, 10:1
- ↑ Harris JE, Eng JJ. Strength training improves upper-limb function in individuals with stroke: a meta-analysis. Stroke. 2010 Jan;41(1):136-40.
- ↑ Barry JG1, Ross SA, Woehrle J. Therapy incorporating a dynamic wrist-hand orthosis versus manual assistance in chronic stroke: a pilot study. J Neurol Phys Ther. 2012 Mar;36(1):17-24.
- ↑ Aukje Andringa, Ingrid van de Port, and Jan-Willem Meijer. Long-Term Use of a Static Hand-Wrist Orthosis in Chronic Stroke Patients: A Pilot Study. Stroke Research and Treatment, 2013.
- ↑ Ann Reinthal, Kathy Szirony, Cindy Clark, Jeffrey Swiers, Michelle Kellicker and Susan Linder. ENGAGE: Guided Activity-Based Gaming in Neurorehabilitation after Stroke: A Pilot Study. troke Research and Treatment, Volume 2012 (2012), Article ID 784232, 10 pages
- ↑ Jordan, Kimberlee; Sampson, Michael; King, Marcus. ;atlitid=212008 Table-Top Exergaming Improves Arm Function in Chronic Stroke. Rehabilitation Engineering and Assistive Technology Society of North America, 2013
- ↑ Andrea Turolla1, Mauro Dam1, Laura Ventura, Paolo Tonin, Michela Agostini, Carla Zucconi, Pawe Kiper, Annachiara Cagnin and Lamberto Piron. Virtual reality for the rehabilitation of the upper limb motor function after stroke: a prospective controlled trial. Journal of NeuroEngineering and Rehabilitation 2013, 10:85
- ↑ S Bermúdez i Badia, E Lewis, S Bleakley. Combining virtual reality and a myo-electric limb orthosis to restore active movement after stroke: a pilot study . Proc. 9th Intl Conf. Disability, Virtual Reality Associated Technologies Laval, France, 10–12 Sept. 2012
- ↑ Thieme H, Mehrholz J, Pohl M, Behrens J, Dohle C. Mirror therapy for improving motor function after stroke. Cochrane Review, 2012
- ↑ Ching-Yi Wu, Pai-Chuan Huang, Yu-Ting Chen, Keh-Chung Lin, Hsiu-Wen Yang. Effects of Mirror Therapy on Motor and Sensory Recovery in Chronic Stroke: A Randomized Controlled Trial. Archives of Physical Medicine and Rehabilitation, American Congress of Rehabilitation Medicine, 2013
- ↑ Lee, Myung Mo; Cho, Hwi-young; Song, Chang Ho. The Mirror Therapy Program Enhances Upper-Limb Motor Recovery and Motor Function in Acute Stroke Patients. American Journal of Physical Medicine and Rehabilitation: August 2012 – Volume 91 – Issue 8 – p 689–700
- ↑ Nahid Norouzi-Gheidari, Philippe S. Archambault, Joyce Fung. Effects of robot-assisted therapy on stroke rehabilitation in upper limbs: Systematic review and meta-analysis of the literature. JRRD, 2012, 49 (4), 479–496
- ↑ Patrizio Sale1, Marco Franceschini1, Stefano Mazzoleni, Enzo Palma1, Maurizio Agosti and Federico Posteraro. Effects of upper limb robot-assisted therapy on motor recovery in subacute stroke patients. Journal of NeuroEngineering and Rehabilitation 2014, 11:104
- ↑ Kwakkel G, Kollen BJ, Krebs HI. Effects of robot-assisted therapy on upper limb recovery after stroke: a systematic review. Neurorehabil Neural Repair. 2008 Mar-Apr;22(2):111-21. Epub 2007 Sep 17.