Definitions
Physical activity is defined as any bodily movement produced by skeletal muscles that result in energy expenditure.It includes all forms of activity, such as everyday walking or cycling to get from A to B, active play, work-related activity, active recreation (such as working out in a gym), dancing, gardening or playing active games, as well as organised and competitive sport[1]. Exercise is a subset of physical activity that is planned, structured, repeated and has a final or an intermediate objective to the improvement or maintenance of physical fitness[2]
Diabetes is a metabolic condition in which the body does not produce sufficient insulin to regulate blood glucose levels or where the insulin produced is unable to work effectively[3]. There are two main types of diabetes:
- Type 1 diabetes also known as Insulin Dependent Diabetes Mellitus (IDDM) is an auto-immune condition in which the cells that produce insulin are destroyed so lifelong treatment with insulin is required to prevent death. It is a chronic disorder characterised by hyperglycaemia (high blood sugar) and disruption in metabolism of carbohydrates, fats, and proteins.[4] It is reported that ~5% of all Diabetes cases are Type 1 DM. [5]
- Type 2 diabetes also known as Non-insulin Dependent Diabetes Mellitus (NIDDM) accounts for at least 90% of all cases of diabetes[6]. It occurs when the body either stops producing enough insulin for its needs or becomes resistant to the effect of insulin produced. The condition is progressive requiring lifestyle management (diet and exercise) at all stages. Over time most people with type 2 diabetes will require oral drugs and or insulin. Type 2 diabetes may remain undetected for many years[7].
Epidemiology
Diabetes Mellitus (both Type 1 and Type 2) is now a global epidemic. Usually correlated with being overweight and obese, a sedentary lifestyle and familial history are also being considered as risk factors.[8] The estimated diabetes prevalence worldwide for 2011 was 366 million and it is expected to affect 552 million people by 2030[9]. The global prevalence of diabetes* among adults over 18 years of age has risen from 4.7% in 1980 to 8.5% in 2014.[10] Diabetes prevalence has been rising more rapidly in middle- and low-income countries. The prevalence of diabetes is higher in men than women, but there are more women with diabetes than men. In England, 6% of people aged 17 years or older had diagnosed with diabetes in 2013[3].
A UK based study in 2004, which studied both type 1 and type 2 diabetes patients, found that only 34% of patients took some form of physical activity and only 9% of these patients exercised sufficiently to achieve a large change in heart rate or breathing[11].
Physical Activity and the Prevention of NIDDM
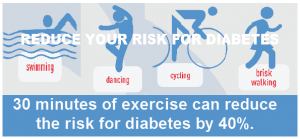
There is a 30% to 40% lower risk of metabolic syndrome and type 2 diabetes in at least moderately active people compared with those who are sedentary[1].
In a study of female registered nurses aged 34–59 years at baseline, women who reported engaging in vigorous exercise at least once a week had a lower incidence of self-reported type 2 diabetes during the 8 years of follow-up than did women who did not exercise weekly[12]. Similar findings were observed between exercise and incidence of type 2 diabetes in a 5-year prospective study of male physicians aged 40–84 years[13]. Likewise, in a large cohort of postmenopausal women aged 55–69 years, the 12-year incidence of diabetes was lower in those women who reported any physical activity compared with the sedentary women[14].
Physical activity may reduce the risk for type 2 diabetes directly through improvements in insulin sensitivity[15]. This may be independent of any effect of activity on weight loss and fat distribution [15]. According to a cross-sectional population study, physical activity was shown to be negatively associated with insulin concentrations in two populations at high risk for diabetes that differed greatly by body mass index[16].
However, a large portion of the effect of physical activity in decreasing insulin resistance is short lived and may last only few days[17][18]. Thus, the consistency of an individual’s activity throughout the years is essential to ensure getting the benefits of exercise on insulin sensitivity.
Benefits of Physical Activities in Diabetes
Physical activity has been shown to decrease cardiovascular risk and mortality[19], in addition to improving lipid profile and endothelial function[20].
Physical activity improves insulin sensitivity[21], which is not unique to those with NIDDM, as patients with IDDM tend to be more insulin resistant than their counterparts without diabetes[19].This effect is related to the promotion of glucose uptake in the skeletal muscles, loss of body fat in the body central part[22], the lipid products reduction and lipid oxidative capacity increase in the muscle cells,[23] the insulin function increase in the organs cells involved in the exercise, the positive regulation of signalling pathway stimulation by insulin[22] glycogen reserve decrease in liver and muscles,[24] the inflammatory markers change[24], the prevention of muscle atrophy, new muscle tissue being built and capillary network congestion increase in muscles[22][24].
Currently, around 50% of patients with IDDM are either overweight or obese. They also have higher waist and hip circumferences when compared to healthy controls[25]. Co-morbidities often associated with excess body weight, reduce the benefits of good metabolic control[26]. Thus, controlling body weight in patients with diabetes is necessary due to the well-known relationship between obesity and cardiovascular disease (CVD)[27].
Carroll & Dudfield reported that in addition to changing Type 2 diabetic patients’ life style, exercise has positive effects on weight loss, waist circumference, fasting glucose plasma and insulin serum levels[28].
The results of one meta-analysis suggest that High Intensity Training is effective at improving measures of insulin resistance compared with continuous exercise and a non-exercising control group. Importantly, the largest effects were seen in those with type 2 diabetes or metabolic syndrome. Furthermore, in those with type 2 diabetes or metabolic syndrome, there was a 0.92 mmol L−1 reduction in fasting glucose and a 0.47% (5 mmol L−1) reduction in HbA1c when compared to studies with a non-exercising control group.There was a significant reduction of 1.3 kg in body weight compared with the non-exercising control group, an effect largely observed in those described as overweight, obese, with, or at risk of type 2 diabetes. In addition, cardiorespiratory fitness improved compared with both controls[29].
Barriers to Physical Activities
Addressing perceived barriers to performing recommended PA levels in this population is crucial for planning effective PA-promoting interventions[30].
Different studies in many communities identified variable barriers. One study of barriers among Irish patients with NIDDM concluded the perceived boring nature of exercise, lack of time, physical pain and depression were the commonest reported major barriers to exercise, and are, therefore, the main issues that need to be overcome when attempting to increase exercise levels in obese Irish patients with NIDDM[31]. Another study in Oman reported lack of willpower, low resources and low social support (especially in females) as the most common barriers to performing leisure PA[30]. Whilst fear of hypoglycaemia, work schedule, loss of control over diabetes, and low levels of fitness were identified by identified by Razeau et al[32].
Other barriers include[33]:
- Fatigue
- Lack self-motivation
- Low self-efficacy
- Fear being injured or have been injured recently
- Lack self-management skills, such as the ability to set personal goals, monitor progress, or reward progress toward such goals
- Barriers related to exercise facilities such as parks, sidewalks, bicycle trails or safe and convenient pleasant walking paths .
On the other hand, Perceived well-being, knowledge of insulin pharmacokinetics, implementation of strategies to reduce the probability of exercise-induced hypoglycaemia, and greater social support were associated with fewer barriers. Moreover, having someone with whom to perform physical activity was also associated with fewer barriers[34].
Promoting Physical Exercise in Individuals with Diabetes
Lifestyle changes may be difficult to undertake, especially in older adults; therefore, self-management education and support focused on general knowledge of diabetes, adherence to therapy, lifestyle changes, and self-monitoring of blood glucose are fundamental to optimise glycemic control in order to prevent or delay acute and chronic complications and to improve quality of life for people with diabetes[35][36][37].
A lot of evidence shows that educational programs addressing nutrition and training administered in the community setting for those with NIDDM can lead to favourable health benefits, including weight reduction, decrease of cardiovascular risk, and improved physical function, especially when these interventions include a cognitive-behavioural approach[38][39][40][37].
Several studies were carried out to investigate the role of exercise in diabetes management, and they confirmed a reduction of medication use (with a consequent decrease of costs) and an improvement of clinical, metabolic, and anthropometric parameters in patients undergoing structured community programs of supervised exercise[41][42][43]. Most of these programs showed the opportunity to combine a multidisciplinary educational intervention with a training program in order to improve the self-management of NIDDM and to establish durable behaviour changes[44][45][46][37].
Exercise Prescription/Recommendations
For meaningful improvements in cardiorespiratory fitness and metabolic health to occur in adults is engaging in a minimum of 150 min of moderate-intensity or 75 min of vigorous-intensity physical activity per week, accumulated in bouts of 10 min or more[29]. The guidelines for weight loss are greater, suggesting that 200–300 min per week are required for long-term reductions[29].
People with diabetes should perform aerobic exercise at moderate intensity 3 or more days per week for a total of 150 minutes minimum per week. Exercise routine should consist of a combination of aerobic and muscle strengthening training. For those who have been sedentary, these individuals should request clearance from their health care provider prior to beginning an exercise program[33].
Safe and effective exercise prescription for the individual with diabetes depends on the careful weighing of multiple factors and sound clinical judgement. Assessment of the individual’s medical history and physical examination will help determine the degree of risk and identify the most appropriate physical activity[33].
PA advice specific to Diabetes:
- The PA programme should consist primarily of aerobic and resistance training, as these have been shown to have clear benefits in prevention and management of diabetes and metabolic syndrome[47][48].
- Aerobic and resistance exercise should be performed at least three times a week; this is because the effect of exercise-induced improvements in insulin action is short-lived[49][43][48]. Most clinical trials evaluating exercise interventions in type 2 diabetes have used a frequency of three times per week, but current guidelines for adults generally recommend five sessions of moderate activity per week[48].
Physiological concerns for Type 2 Diabetes include the following:
- When BG values are above 300 mg/dl during physical activity, hydration is important. If BG results are consistently elevated, patients should consult with their health care provider and/or diabetes specialist prior to continuing their regular exercise program[50][33].
- Persons with type 1 diabetes should check for ketones if BG is greater than 300 mg/dl. If present, activity should be delayed, individual should hydrate and follow plan of care for elevated ketones. However, it is not necessary to postpone physical activity based simply on hyperglycaemia, provided the patient feels well and urine and/or blood ketones are trace or absent[51][33].
- Peripheral neuropathy is a concern in regards to foot injury. Individuals without acute ulceration can participate in moderate weight bearing exercise. Careful attention to appropriate foot wear and any signs of foot damage should be emphasised[52]. Balance may also be compromised and should be evaluated due to increased risk of falls[53]. Consider consultation with a podiatrist to determine patient’s risk[33].
- Autonomic neuropathy increases the risk of silent heart attack and hypotension. If there are unexplained symptoms and feelings of extreme fatigue which last for more than a few minutes, physical activity should be stopped and the individual should be coached to report it immediately to their health care provider. The individual may also have more difficulty adjusting to temperature extremes and should consider this when choosing a physical activity for that day[52]. Evaluation by their health care provider is appropriate and the individual may be referred to a cardiac rehabilitation program for monitoring during exercise[33].
- Those with a history of uncontrolled proliferative retinopathy should avoid activities that increase the risk of intra-ocular pressure such as the Valsalva manoeuvre that include lifting heavy weights or jarring the head, that may occur in contact sports. In the absence of haemorrhaging, individuals can participate in moderate activity[48][33].
Exercising with Type 1 Diabetes
- Regular monitoring of blood glucose concentrations, and trial and error is needed to understand and manage each individuals response to exercise
- Intensity and duration of exercise
- Pre-exercise insulin dose generally needs to be reduced when exercise extends beyond 30 minutes
- Varies for each individual; generally, longer exercise, less insulin
- Degree of metabolic control before exercise
- Easier to manage and predict the body’s response to exercise when metabolic control is good
- Dangerous to commence exercise when blood glucose levels are high and ketones are present in the urine
- Type and dose of insulin injected before exercise
- Common practice to use a mixture of short and long lasting insulin
- Necessary to predict the peak period of insulin activity to avoid excessive levels of insulin in the blood at the same time as exercising.
- Site of insulin injection
- Insulin absorption is increased in exercising muscles
- The abdomen is usually the preferred site for insulin injection prior to exercise
- Timing of previous meal
- Insulin requirements are influenced by the amount and type of food consumed
- During exercise carbohydrate
- Blood glucose 5 to 10 mmol/l: 30 to 45 g CHO/h
- Blood glucose 10 to 14 mmol/l: 15 g CHO/h
- Blood glucose >14 mmol/l: no exercise
Role of the Physiotherapist
Exercise training programs have emerged as a useful therapeutic regimen for the management of diabetes mellitus. [54] Primary effects include the development of aerobic and resistance exercise programs which have been shown to decrease the incidence of NIDDM. Secondary effects include the ability of aerobic and resistance training to help in the control of diabetes. There is accumulating evidence that combined aerobic and resistance exercise training is more effective than either model alone.
It is important to be aware of Hyperglycaemia, caused by a lack of glucose control, and Hypoglycaemia, caused by taking too much insulin or glucose-lowering drugs. Contra-indications to exercise are blood glucose levels >250mg/dl and
A combination of aerobic and strengthening exercises should be recommended. But precautionary measures for exercise involving the feet are essential for many patients with diabetes. The overall aim of exercise prescription, as mentioned above, is to achieve the ACSM guidelines for healthy sedentary individuals. A diabetes identification bracelet or shoe tag should be clearly visible when exercising.
Resources
References
- ↑ 1.01.1 Officers, C. M. (n.d.). Start Active , Stay Active.
- ↑ Caspersen, C. J., Powell, K. E., & Christenson, G. M. (1985). Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Reports (Washington, D.C. : 1974), 100(2), 126–31. https://doi.org/10.2307/20056429)
- ↑ 3.03.1 England, P. H. (n.d.). Adult obesity and type 2 diabetes About Public Health England.
- ↑ Goodman CC, Snyder TEK. Differential Diagnosis for Physical Therapists: Screening for Referral. 5th ed. St. Louis, MO: Saunders/Elsevier; 2013: 425-432.
- ↑ American Diabetes Association. Type 1 Diabetes. Available from: http://www.diabetes.org/diabetes-basics/type-1/?loc=util-header_type1 (accessed 8 April 2016).
- ↑ National Collaborating Centre for Chronic Conditions. Type 2 diabetes. National clinical guideline for management in primary and secondary care (update). London: Royal College of Physicians, 2008.
- ↑ International Diabetes Federation. Types of diabetes. Secondary International Diabetes Federation. Types of diabetes. http://www.idf.org/types-diabetes.
- ↑ Diabetes. (2017, November 14). Physiopedia, . Retrieved 14:29, April 8, 2018 from https://www.physio-pedia.com/index.php?title=Diabetes&oldid=180689.
- ↑ DIABETES IN THE UK 2012 Key statistics on diabetes. (2012), (April).
- ↑ Projections of global mortality and burden of disease from 2002 to 2030.
Mathers CD, Loncar D. PLoS Med, 2006, 3(11):e442.
- ↑ Thomas N, Alder E, Leese GP. Barriers to physical activity in patient with diabetes. Postgrad Med J 2004; 80:287–91.
- ↑ Manson JE, Rimm EB, Stampfer MJ, et al. Physical activity and incidence of non-insulin-dependent diabetes mellitus in women. Lancet 1991;338:774–8.
- ↑ Manson JE, Nathan DM, Krolewski AS, et al. A prospective study of exercise and incidence of diabetes among US male physicians. JAMA 1992;268:63–7.
- ↑ Folsom AR, Kushi LH, Hong CP. Physical activity and incident diabetes mellitus in postmenopausal women. Am J Public Health 2000;90:134–8mellitus. Exerc Sport Sci Rev 1999; 27:1–35.
- ↑ 15.015.1 Ivy JL, Zderic TW, Fogt DL. Prevention and treatment of noninsulin-dependent diabetes 16. Manson JE, Rimm EB, Stampfer MJ, et al. Physical activity and incidence of non-insulin-dependent diabetes mellitus in women. Lancet 1991;338:774–8.
- ↑ Kriska AM, Pereira MA, Hanson RL, et al. Association of physical activity and serum insulin concentrations in two populations at high risk for type 2 diabetes but differing by BMI. Diabetes Care 2001;24:1175–80.
- ↑ Heath GW, Gavin JR 3rd, Hinderliter JM, et al. Effects of exercise and lack of exercise on glucose tolerance and insulin sensitivity. J Appl Physiol 1983;55:512–17.
- ↑ Koivisto VA, Yki-Jarvinen H, DeFronzo RA. Physical training and insulin sensitivity. Diabetes Metab Rev 1986;1:445–81.
- ↑ 19.019.1 Chimen M, Kennedy A, Nirantharakumar K, Pang TT, Andrews R, Narendran P.What are the health benefits of physical activity in type 1 diabetes mellitus? A literature review. Diabetologia. 2012;55(3):542–51. doi:10.1007/s00125-011-2403-2.
- ↑ 40. Fuchsjäger-Mayrl G, Pleiner J,Wiesinger GF, Sieder AE, Quittan M, NuhrMJ, et al. Exercise training improves vascular endothelial function in patients with type 1 diabetes. Diabetes Care. 2002;25(10):1795–801. doi:10.2337/diacare.25.10.1795.
- ↑ 41. Hawley JA. Exercise as a therapeutic intervention for the prevention and treatment of insulin resistance. Diabetes Metab Res Rev. 2004;20(5):383–93. doi:10.1002/dmrr.505.
- ↑ 22.022.122.2 Teixeira-Lemos, E., Nunes, S., Teixeira, F., & Reis, F. (2011). Regular physical exercise training assists in preventing type 2 diabetes development: focus on its antioxidant and anti-inflammatory properties. Cardiovascular Diabetology, 10(1), 12. doi:10.1186/1475-2840-10-12
- ↑ Turcotte, L. P., & Fisher, J. S. (2008). Skeletal Muscle Insulin Resistance: Roles of Fatty Acid Metabolism and Exercise. Physical Therapy, 88(11), 1279–1296. http://doi.org/10.2522/ptj.20080018
- ↑ 24.024.124.2 Praet, S., & van Loon, L. (2009). Exercise therapy in Type 2 diabetes. Acta Diabetologica, 46(4), 263-278. doi:10.1007/s00592-009-0129-0
- ↑ Szadkowska A,Madej A, Ziolkowska K, Szymanska M, Jeziorny K,Mianowska B, et al. Gender and age dependent effect of type 1 diabetes on obesity and altered body composition in young adults. Annals of Agricultural and Environmental Medicine: AAEM. 2015;22(1):124–8. doi:10.5604/12321966.1141381.
- ↑ Chillaron JJ, Benaiges D,Mane L, Pedro-Botet J, Flores Le-Roux JA. Obesity and type 1 diabetes mellitus management. Minerva Endocrinol. 2015;40(1):53–60.
- ↑ de Ferranti SD, de Boer IH, Fonseca V, Fox CS, Golden SH, Lavie CJ, et al. Type 1 diabetes mellitus and cardiovascular disease: a scientific statement from the American Heart Association and American Diabetes Association. Diabetes Care. 2014;37(10): 2843–63. doi:10.2337/dc14-1720.
- ↑ M, Carroll. 2018. “What Is The Relationship Between Exercise And Metabolic Abnormalities? A Review Of The Metabolic Syndrome. – Pubmed – NCBI
- ↑ 29.029.129.2 Jelleyman, C., Yates, T., Donovan, G. O., Gray, L. J., King, J. A., Khunti, K., & Davies, M. J. (2015). Physical Activity / Metabolic Effects The effects of high-intensity interval training on glucose regulation and insulin resistance : a meta-analysis, (10). https://doi.org/10.1111/obr.12317
- ↑ 30.030.1 Alghafri, T., Alharthi, S. M., Mohd, Y., Farsi, A., Bannerman, E., Craigie, A. M., & Anderson, A. S. (2017). Perceived barriers to leisure time physical activity in adults with type 2 diabetes attending primary healthcare in Oman : a cross-sectional survey. https://doi.org/10.1136/bmjopen-2017-016946
- ↑ Egan, A. M., Mahmood, W. A. W., Fenton, R., Redziniak, N., Tun, T. K., Sreenan, S., & Mcdermott, J. H. (2017). Barriers to exercise in obese patients with type 2 diabetes, (March 2013), 635–638. https://doi.org/10.1093/qjmed/hct075
- ↑ Razeau, A. N. N. E. O. B., & Ircescu, H. O. M. (2008). Barriers to Physical Activity Among Patients With Type 1 Diabetes, 31(11), 2108–2109. https://doi.org/10.2337/dc08-0720.
- ↑ 33.033.133.233.333.433.533.633.7 Diabetes and Physical Activity Practice Synopsis October 22, 2015. American Association of Diabetics Educators.
- ↑ Brazeau, A., Rabasa-Lhoret, R., Strychar, I., & Mircescu, H. (2008). Barriers to Physical Activity Among Patients With Type 1 Diabetes. Diabetes Care, 31(11), 2108-2109. doi:10.2337/dc08-0720
- ↑ Goudswaard AN, Stolk RP, Zuithoff NP, de Valk HW, Rutten GE. Long-term effects of self-management education for patients with type 2 diabetes taking maximal oral hypoglycaemic therapy: a randomized trial in primary care. Diabet Med. 2004;21(5):491–6.
- ↑ Haas L, Maryniuk M, Beck J, et al. National standards for diabetes self-management education and support. Diabetes Care. 2014;37(1):S144–53.
- ↑ 37.037.137.2 Galle, F., Di, V., Assunta, O., Di, M., Alessandra, D., Tiziana, M., & Giorgio, S. (2017). Improving Self-Management of Type 2 Diabetes in Overweight and Inactive Patients Through an Educational and Motivational Intervention Addressing Diet and Physical Activity : A Prospective Study in Naples , South Italy, 875–886. https://doi.org/10.1007/s13300-017-0283-2
- ↑ Dunstan DW, Daly RM, Owen N, et al. High-intensity resistance training improves glycemic control in older patients with type 2 diabetes. Diabetes Care. 2002;25(10):1729–36.
- ↑ Goldhaber-Fiebert JD, Goldhaber-Fiebert SN, Tristain ML, Nathan DM. Randomized controlled community-based nutrition and exercise intervention improves glycemia and cardiovascular risk factors in type 2 diabetic patients in rural Costa Rica. Diabetes Care. 2003;26(1):24–9.
- ↑ Klein S, Sheard NF, Pi-Sunyer X, et al. Weight management through lifestyle modification for the prevention and management of type 2 diabetes: rationale and strategies: a statement of the American Diabetes Association, the North American Association for the Study of Obesity, and the American Society for Clinical Nutrition. Diabetes Care. 2004;27(8):2067–73.
- ↑ Di Loreto C, Fanelli C, Lucidi P, et al. Validation of a counselling strategy to promote the adoption and the maintenance of physical activity by type 2 diabetic subjects. Diabetes Care. 2003;26:404–8.
- ↑ Di Loreto C, Fanelli C, Lucidi P, et al. Make your diabetic patients walk: long-term impact of different amounts of physical activity on type 2 diabetes. Diabetes Care. 2005;28:1295–302.
- ↑ 43.043.1 Balducci S, Zanuso S, Massarini M, et al. The Italian diabetes and Exercise Study (IDES): design and methods for a prospective Italian multicentre trial of intensive lifestyle intervention in people with type 2 diabetes and the metabolic syndrome Group1. Nutr Metab Cardiovasc Dis. 2008;18:585–95.
- ↑ Italian Barometer Diabetes Observatory. Italian barometer of diabetes and physical activity. 2011. http://www.ibdo.it/pdf/2-Diabetes-Barometer-Report.
- ↑ Coppola A, Sasso L, Bagnasco A, Giustina A, Gazzaruso C. The role of patient education in the prevention and management of type 2 diabetes: an overview. Endocrine. 2016;53(1):18–27.
- ↑ Sun J, Wang Y, Chen X, et al. An integrated intervention program to control diabetes in overweight Chinese women and men with type 2 diabetes. Asia Pac J Clin Nutr. 2008;17(3):514–24.
- ↑ Zanuso s, Jimenez A, Pugliese G, Corigliano G, Balducci S.
Exercise for the management of type 2 diabetes: a review of the evidenceActa Diabetologica , Volume 47, Issue 1, pp 15–22
- ↑ 48.048.148.248.3 Colberg S et al. Exercise and Type 2 Diabetes: American College of Sports Medicine and the American Diabetes Association: Joint Position Statement. Diabetes Care. 2010;33(12):2692-2696.
- ↑ O’Donovan G1, Kearney EM, Nevill AM, Woolf-May K, Bird SR.
The effects of 24 weeks of moderate- or high-intensity exercise on insulin resistance.
Eur J Appl Physiol. 2005 Dec;95(5-6):522-8. Epub 2005 Sep 6 - ↑ Lopez-Jimenez, et al. Recommendations for managing patients with diabetes mellitus in cardiopulmonary rehabilitation: an American association of cardiovascular and pulmonary rehabilitation statement. Journal of Cardiopulmonary Rehabilitation and Prevention. 2011; 32:101-112.
- ↑ Standards of Medical Care. Diabetes Care. 2015;38 (suppl 1),S24.
- ↑ 52.052.1 Colberg, Sheri. Exercise and Diabetes: A Clinician’s Guide to Prescribing Physical Activity. American Diabetes Association: Alexandria, VA, 2013; 66.
- ↑ Botelhoa M, Conde M, Rebelo Braz NM. Functional aspects in aging adults with diabetic neuropathy. A review. Curr Diabetes Rev. 2015 Jul 22
- ↑ Thent ZC, Das S, Henry LJ. Role of exercise in the management of diabetes mellitus: the global scenario. PloS one. 2013 Nov 13;8(11):e80436.