Objective
The North Star Ambulatory Assessment (NSAA) is a 17-item rating scale that is used to measure functional motor abilities in ambulant children with Duchenne Muscular Dystrophy (DMD). It is usually used to monitor the progression of the disease and treatment effects.
Intended Population
Ambulant children with DMD.
Method of Use
Equipment Required:
- a size-appropriate chair or height adjustable plinth
- box step, approximately 15 cm high
- a mat
- a stopwatch
- a clear, straight, and marked 10 metres pathway
Test Details and Instruction[1]:
The test must be completed without the use of any thoracic brace or leg orthoses. Therapist asks the patient to complete activities listed in the table below.
The activities are graded as follows:
2 – “Normal” – no obvious modification of activity
1 – Modified method but achieves goal independent of physical assistance from another
0 – Unable to achieve independently
This scale is ordinal with 34 as the maximum score indicating fully-independent function.
| Activity | Instructions to patient | Starting position / test detail | Comments |
|---|---|---|---|
| 1. Stand | Can you stand up tall for me
for as long as you can and as still as you can? |
Feet should be close together and heels on the
ground if possible. Arms by sides. NO shoes should be worn. |
Best done on the floor rather than on a mat.
Whichever is chosen maintain consistency through repeated testing sessions. Minimum count of 3 seconds to score 2. |
| 2. Walk | Can you walk from A to B
(state to and where from) for me? |
Walk without shoes/socks on. Should be
enough of a distance to observe ‘normal gait’ for that subject. |
A value judgement needs to be made in scoring –
if the patient generally toe walks but occasionally gets heels flat, or can on request but doesn’t usually, they should score 1 |
| 3. Stand up
from chair |
Stand up from the chair
keeping your arms folded if you can |
Starting position 90º hips and knees, feet on
floor/supported on a box step. |
A size-appropriate chair or height adjustable plinth
should be used. Arms should be kept crossed throughout the activity to score 2. |
| 4. Stand on
one leg – Right |
Can you stand on your right
leg for as long as you can? |
Minimum count of 3 seconds to score 2. NO
shoes should be worn. |
Best done on the floor rather than on a mat.
Whichever is chosen maintain consistency through repeated testing sessions. |
| 5. Stand on
one leg – Left |
Can you stand on your left
leg for as long as you can? |
Minimum count of 3 seconds to score 2. NO
shoes should be worn. |
Best done on the floor rather than on a mat.
Whichever is chosen maintain consistency through repeated testing sessions. |
| 6. Climb
box step – right |
Can you step onto the top of
the box using your right leg first? |
Stands facing the box step. Step should be
approximately 15cm high |
Support may be provided by the use of a height
adjustable plinth, or, if not available a ‘neutral’ hand from the therapist. |
| 7. Climb
box step – left |
Can you step onto the top of
the box using your left leg first? |
Stands facing the box step. Step should be
approximately 15cm high |
Support may be provided by the use of a height
adjustable plinth, or, if not available a ‘neutral’ hand from the therapist. |
| 8. Descend
box step – Right |
Can you step down from the
box using your right leg first? |
Stands on top of the box step facing forwards.
Step should be approximately 15cm high |
Support may be provided by the use of a height
adjustable plinth, or, if not available a ‘neutral’ hand from the therapist. |
| 9. Descend
box step – Left |
Can you step down from the
box using your left leg first? |
Stands on top of the box step facing forwards.
Step should be approximately 15cm high |
Support may be provided by the use of a height
adjustable plinth, or, if not available a ‘neutral’ hand from the therapist. |
| 10. Gets to
sitting |
Can you get from lying to
sitting? |
Starting position supine on a mat. No pillow
should be used under head |
If patient turns into prone or towards the floor to
work their way into sitting 1 should be scored |
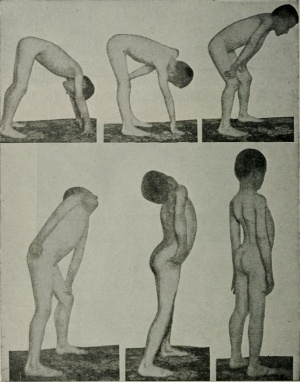
| 11. Rise
from floor |
Get up from the floor using
as little support as possible and as fast as you can (from supine) |
Starting position supine with arms by sides,
legs straight. No pillow to be used |
Activity should be attempted without use of
furniture in the first instance. Do not note time if a chair has to be used. |
| 12. Lifts
head |
Lift your head to look at your
toes keeping your arms folded |
Supine on a mat. No pillow should be used. | Ask patient to keep arms crossed over chest
during the activity to avoid self-assist. Also ask to look at toes to ensure neck is flexed – should be a chin to chest manoeuvre. |
| 13. Stands
on heels |
Can you stand on your
heels? |
Standing on the floor. No shoes to be worn. | Watch for inversion. If substantial inversion but
forefeet are still lifted – score 1. If only inversion with lateral border of foot still on the ground score 0. |
| 14. Jump | How high can you jump? | Standing on the floor, feet fairly close together. | Want height, not forward movement. Small
amount of forward movement acceptable |
| 15. Hop
right leg |
Can you hop on your right
leg? |
Starting position standing on floor on right leg.
No shoes should be worn. |
Needs obvious floor clearance to score 2 |
| 16. Hop left
leg |
Can you hop on your left
leg? |
Starting position standing on floor on right leg.
No shoes should be worn. |
Needs obvious floor clearance to score 2 |
| 17. Run
(10m) |
Run as fast you can
to……(give point) |
A straight 10m walkway should be clearly
marked in a quiet department or corridor. A stopwatch should be used to time the walk. Be consistent as to whether shoes are worn or not. Ensure safety of patient. They should self select speed after being asked to go ‘as fast as they can’. |
‘Duchenne jog’ – not a true run (there probably IS
a double support phase), but more than a walk. Typically characterized by excessive use of arms, trunk rotation, substantial ’waddle’. No real ‘pushoff’ |
Evidence
Several studies have shown that NSAA is a quick[2], specific[2], reliable[3][4][5], valid[3], and clinically relevant[2][3] method to measure the functional motor ability of ambulant children with DMD. NSAA is also considered to be suitable to be used in research[2] and in a multicentric setting provided that adequate training is given[4].
Reliability
- A psychometric assessment of NSAA[3] showed that NSAA has 0.91 Person Separation Index (i.e. a reliability statistic).
- A multicentric study[4] showed that NSAA has a high intra-observer reliability of 0.95. It has a low inter-observer reliability (
- Another study[5] showed that NSAA has a high test-retest ability. It also has a high inter-rater reliability with 0.95 consistency and more than 0.93 absolute agreement.
Validity
A psychometric assessment of NSAA[3] showed that NSAA is valid with a good targeting (i.e. very few items measure the same level of ability) which equates to a better interpretation of results, This study also showed that NSAA has little misfit; which means that there was only a few items where the participants performed differently from the prediction. In fact, there was only one item (i.e. “lifting head from supine”) where the participants performed significantly differently from the prediction.
Clinical Relevance
- A psychometric assessment of NSAA[3] showed that the hierarchy of items within NSAA was supported by clinical expert opinion, thus increasing its clinical interpretability. The items in NSAA scale are listed based on their level of difficulty which is mostly agreed by experts (ρ = 0.80).
- A questionnaire-based study[2] showed that clinicians considered NSAA as clinically relevant.
Miscellaneous
A revised version of NSAA was developed with items ordered according to the participants’ age when they could be reliably performed. This version showed that NSAA can be used in patients starting from the age of three years[6].
Links
North Star Ambulatory Assessment
Registry of Outcome Measures – North Star Ambulatory Assessment
References
- ↑ Muscular Dystrophy UK. North Star Ambulatory Assessment. http://www.musculardystrophyuk.org/assets/0000/6388/NorthStar.pdf (accessed in 7 March 2018)
- ↑ 2.02.12.22.32.4 Mercuri E, Mayhew A, Muntoni F, Messina S, Straub V, Van Ommen GJ, et al. On behalf of the TREAT-NMD Neuromuscular Network. Towards harmonisation of outcome measures for DMD and SMA within TREAT-NMD; Report of three expert workshops: TREAT-NMD/ENMC workshop on outcome measures, 12th–13th May 2007, Naarden, The Netherlands; TREAT-NMD workshop on outcome measures in experimental trials for DMD, 30th June–1st July 2007, Naarden, The Netherlands; Conjoint Institute of Myology TREAT-NMD Meeting on physical activity monitoring in neuromuscular disorders, 11th July 2007, Paris, France. Neuromuscul Disord 2008;18:894–903.
- ↑ 3.03.13.23.33.43.5 Mayhew A. Cano S. Scott E. Eagle M. Bushby K. Muntoni F. On behalf of the North Star Clinical Network for Paediatric Neuromuscular Disease. Moving towards meaningful measurement: Rasch analysis of the North Star Ambulatory Assessment in Duchenne muscular dystrophy. Developmental medicine & child neurology 2011; 535-542
- ↑ 4.04.14.2 Mazzone ES, Messina S, Vasco G, et al. Reliability of the North Star Ambulatory Assessment in a multicentric setting. Neuromuscul Disord 2009; 19: 458–61.
- ↑ 5.05.1 Scott E. Eagle M. Mayhew A. Freeman J. Main M. Sheehan J. Manzur A. Muntoni F. Development of a functional assessment scale for ambulatory boys with Duchenne muscular dystrophy. Physiother Res Int. 2012; 17(2): 101-9
- ↑ Mercuri E. Coratti G. Messina S. Ricotti V. Baranello G. D’Amico A. et al. Revised North Star Ambulatory Assessment for Young Boys with Duchenne Muscular Dystrophy. PLoS ONE 2016; 11(8): e0160195. doi:10.1371/journal.pone.0160195