Introduction
According to Ryerson (2008)[1] assessment in neurological physiotherapy is a process of collecting information about disordered movement patterns, underlying impairments, activity restrictions, and societal participation for the purpose of intervention planning. While Bernhardt & Hill (2005)[2] outline that the purpose of assessment is to help the therapist determine the best intervention. Assessment is arguably the most important step in the rehabilitation process, as our clinical reasoning is based on the information it provides and provides the basis for our decision making throughout the rehabilitation process. Johnson & Thompson (1996) outlined that treatment can only be as good as the assessment on which it was based. So in order for us to progress and manage our treatment plan and ensure we are identifying out patients problems assessment should be an ongoing and continuous, and should allow us toindividualised, patient-centred goals and ultimately a tailor-made treatment plan for the individual.
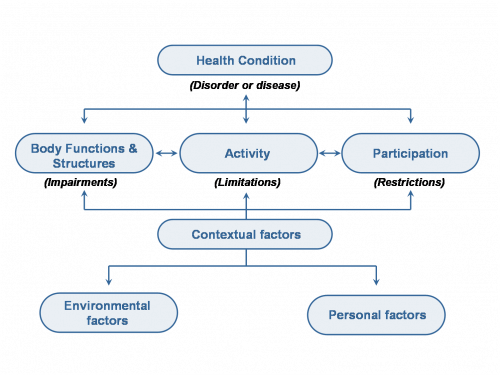
Tempest et al (2013)[3] identified that the International Classification of Functioning, Disability and Health (ICF) enhanced clarity of communication and team roles within an acute stroke multidisciplinary team as well as with other clinicians, patients and their relatives. In addition, the ICF challenged stroke clinicians to think holistically, thereby appropriately extending their domain of concern beyond their traditional remit. We can use the framework of the ICF to define the role and purpose of physiotherapy for patients with neurological conditions. The ICF was introduced by the World Health Organization (WHO) in 2011 and is a revised version of the International Classification of Impairment, Disability and Handicap. The ICF defines components of health from the perspective of the body, the individual and society. One of its primary purposes is to provide unified and standard language for those working in the area disability.
We can use the ICF to articulate the goals and purpose of physiotherapy for patients following Stroke. For example, the health condition is Stroke. An associated impairment is poor strength. Poor strength directly impacts on the ability to perform activities such as walking and moving. This in turn has implications for participation, such as working, engaging in family life and participating in community activities. Impairments, activity limitations and participation restrictions are all affected by environmental and personal factors, such as support from family and employers, access to appropriate equipment, financial situation and coping mechanisms. In the ICF framework, such environmental and personal influences are termed contextual factors.
Tempest et al (2013)[3] also found that the ICF can also challenge clinicians, in a positive way, to help them think more holistically about patient needs following a stroke. The framework and classification allowed the holistic nature of acute stroke multidisciplinary team work to be communicated within and beyond the team. Furthermore, it promoted team work by clarifying team roles in relation to patient care.
Ensure you are familiar with the ICF, its general use in Clinical Practice and its use within the Neurorehabilitation Process as it should provide the framework for your assessment and treatment throughout the rehabilitation process: You can find out more about the role of the ICF in your assessment process from the following articles
Database
Reviewing the patients medical chart and leasing with the medical team forms the initial element of any patient assessment, providing background data about the patient to assist us to determine if the patient is medically stable and ready for physiotherapy intervention[1].
Presenting Condition
- Diagnosis
Type of Stroke e.g Ischemic or Haemorrhagic
Location of Stroke e.g. Right of Left Hemisphere, MCA, PCA etc.
History of Presenting Condition
- Date of Onset of Signs & Symptoms
When did initial symptoms appear, where they sudden or did they come on gradually. This can have a bearing on what type of Medical Treatment options may be available to the patient. - Progression of the Condition
Look for changes in the initial symptoms, which may provide some information about the behavior of the condition and some prediction of prognosis e.g. has there been a change in the NIHSS Scale since addmission? Following treatment? - Medical Management
How has the condition been managed by the medical team? Did they require neurosurgery or other medical interventions? - Medical Observations
Provides information on how medically stable the patient is and on their suitability for assessment - Other Management
What other management is in place for the patient that your assessment may need to be scheduled around e.g. Nutritional and Feeding needs – if patient has not got adequate intake this could affect your assessment - Previous Therapy
Has the pateint previously been involved in Physiotherapy? What are their expectations of physiotherapy? - Results of Specific Investigations
Results of these investigations assis us in having an overall understanding of the patients condition and provide us with specific information which allow us to predict the signs and symptoms that are likely to be present and assist us in planning our objective assessment e.g. in a cerebellar artery infarct we would expect our patient to have ataxia and therefore need to ensure our objective assessment caters for this. Please click on the links to find out more detailed information about these types of investigations.
Past Medical History
- Co-morbidities
Consider the impact of other co-morbidities on treatment and management - Previous Neurological Conditions
Has the patient had previous neurological conditions which had an impact on their functional abilities and may be useful in predicting future outcomes e.g. previous TIA’s, CVA’s - Special Equipment
Does the patient require the use of specialized equipment for their management
e.g. Suction Units, Special Seating, Orthotics, Gait Aids - Technology Dependency
Is the patient dependant on certain technologies either prior to this addmission or new since this addmission that you need to be aware of?
e.g. Home Oxygen, Pacemaker, Nasal Gastric Tube - Previous Surgery
Has the patient had previous surgery which could impact on your assessment and has impacted on their function?
e.g. Joint Replacements, Abdominal Surgery - Risk Factors
Does the patient have specific risk factors that could be related to further Neurological Incident
e.g. Atrial Fibrillation, Hypertension, High Cholesterol, Diabetes Mellitus - Medication History
Recognise any contraindications for Physiotherapy Treatment e.g. Timeframe to treat post Thrombolysis
Impact of Related Side Effects on Treatment e.g. Dantrolene can cause Nausea
Subjective
The subjective assessment is used to provide a detailed picture of how the present condition affects the patient. Always consider your verbal and non-verbal communication as this will influence your interaction, as will thh environment and your position in relation to the patient. Understanding what the patient was able to do pre-stroke is vital in order to guide your objective assessment, set appropriate, realistic goals to guide treatment and maintain patient motivation.[5]
Social History
Having an understanding of the patients Social Situation will allow you to plan for discharge and to ensure adequate supports are in place for the patient both during and after their treatment.
- Social Situation
What is the patients background - Support Structures
What support structures does the patient have from family, friends, colleagues or dependants. Having an understanding of these structures is key when looking at your discharge plans and what may be needed for that patient when their inpatient treatment may be complete. - Accommodation
What type of accommodation are they living in and who are they living with?
Again this is key information for goal planning with the patient and when planning for discharge options.
e.g. Two Storey, Bungalow, Apartment, Access such as Stairs, Steps Elevators - Social Service Support
Was the patient previously linked in with any Social Services supports?
Public Health Nurse, Home Care Supports, Meals on Wheels
Activity
Understanding the patients involvment in actcities of daily life prior will give an indication of what their level of participation was prior to their Stroke and assists in Goal Setting and treatment plannning for the patient. It can also provide motivation for the patient during treatment if our treatment plans incorporate activities of interest to the patient.
- Normal Daily Routine
What would the patients daily routine be? Do they do their own cooking, cleaning and other domestic tasks? What time do they tend to get up, go to bed etc. - Employment
Is the patient Employed? Unemployed? In Education? Retired? Work in the Home?
What type of activities were involved ? - Leisure Activities
How does the patients normally spend their free time? What activities do they like to be ivolved in? Can these be incorporated into Treatment?
Sport, Art, Music, Reading, Outdoors
Mobility
It is important to understand what an indivduals mobility had been prior to their Stroke and to understand what factors influenced their mobility. We need to ensure we consider mobility in relation to the following areas:
- General
- Indoor
- Outdoor
- Steps & Stairs
- Falls History
Personal Care
How did the patient manage personal care prior to the Stroke? Did they need assistance and use any aids/devices to assist.
- Washing
- Dressing
- Continence
Other
- Vision
Do they wear glasses?
What do they wear them for? e.g Reading, Driving - Hearing
Do they wear a Hearing Aid?
Are they wearing it?
Is it Switched On / Working - Communication
Do they have difficulty expressing themselves or understanding your requests? - Cognition
Does the patient have difficulty concentrating, understanding instructions or following instructions? Consider how this impacts on both your assessment but also on your ongoing treatment planning. - Swallowing
Do they have difficulty swallowing?
Do they cough or choke after eating or drinking? - Fatigue
Do they tire quickly? - Pain
Is pain an issue either now or prior to Stroke? How does this impact on the patient? Does it have an impact on your assessment? How is pain managed? - Perceptions of own Problems/Main Concern
Understanding what is important to the patient is key to successful goal planning and eventually patient motivation for treatment. Ensure you try to determine what the patient perceives to be their main issues and why? - Expectations of Treatment
What does the patient expect to get from Physiotherapy? Do they have realistic expectations or understanding of their situation?
Objective
Posture
[6]. Posture in easy terms can be understood as the position in which you hold your body when standing or sitting. Read more about Posture in physiopedia Balance
Voluntary Movement
According to Jones (2011) muscle tone is the state of readiness in a muscle at rest which provides us with a background level of tone from which we can function efficiently, defined by teh resistance to passive movement. NOrmal tone should be high enough to maintain our position upright against gravity but low enough to allow voluntary movement[5]. Muscle tone is dependant on two physiologial factors;
Neural factors relate to the degree of activation of the contractile apparatus of the muscle which is a result of output from the alpha motor neuron in the ventral horn of the spinal cord[5].
Non-Neural factors relate to mecanical-elastic properties of the soft tissue incorporating the viscosity of the muscle and muscle length, which can be influenced by age, temperature and exercise[5].
Involuntary Movement
Tremor is an involuntary, somewhat rhythmic, muscle contraction and relaxation involving oscillations or twitching movements of one or more body parts. It is the most common of all involuntary movements and can affect the hands, arms, eyes, face, head, vocal folds, trunk, and legs. Most tremors occur in the hands.
Clonus is a series of involuntary, rhythmic, muscular contractions and relaxations which is a sign of an upper motor neuron lesion involving descending motor pathways, and in many cases is, accompanied by spasticity (another form of hyper excitability). Clonus causes large motions that are usually initiated by a reflex[5].
Chorea is characterized by brief, semi-directed, irregular movements that are not repetitive or rhythmic, but appear to flow from one muscle to the next. These ‘dance-like’ movements of chorea often occur with athetosis, which adds twisting and writhing movements. Walking may become difficult, and include odd postures and leg movements. Movements of chorea and ballism occur on their own, without conscious effort. Thus, chorea is said to be a hyperkinetic movement disorder.
An involuntary movement of a body part associated with the resisted movement of another body part. Movements of body parts other than the ones that are intended to move, often increased with increased effortTone
Damage to the Central Nervous System may cause an individual to lose the ability to control muscle tone which can lead to eithe an increase or decrease in muscle resting tone[8].
- Decreased
Hypotonia, or low tone, is a reduced level of muscle stiffness, providing little to no resistance to passive movement. Patients with hypotonia have heavy limbs when handled and have difficulty maintining an upright position against gravity. - Increased
[9]. Read more about Spasticity on Physiopedia [5].
Reflexes
Hoffmann’s reflex, named for Johann Hoffmann, is a finding elicited by a reflex test which verifies the presence or absence of problems in the corticospinal tract. The test involves tapping the nail or flicking the terminal phalanx of the middle or ring finger. A positive response is seen with flexion of the terminal phalanx of the thumb.
Sensation
According to Jones (2011)[5] sensation is complex consisting of several modalities including our four special senses including Vision, Hearing, Smell and Taste and our Somatosensory Senses including tactile – light touch and pressure, proprioception, temperature and pain. Sensation plays a huge role in how we perceive our environment, impacts on our control of movement, maintaining arousal and provides warning of potential danger[5]. The evaluation of sensation, or any sensory modality for that mattter, is highly dependent on the ability and desire of the patient to cooperate. Sensation belongs to the patient (i.e., is subjective) and the examiner must therefore depend almost entirely on their reliability. Sensory changes that are unassociated with any other abnormalities (i.e., motor, reflex, cranial, hemispheric dysfunctions) must be considered weak evidence of disease unless a pattern of loss in a classical sensory pattern is elicited e.g. in a typical pattern of peripheral nerve or nerve root distribution. Therefore, one of the principle goals of the sensory exam is to identify meaningful patterns of sensory loss. Basic testing should sample the major functional subdivisions of the sensory systems. The patient’s eyes should be closed throughout the sensory examination.
| Sensory Receptor | Nerve Fibre | Sensory Pathway | |
| Light Touch |
Meissner’s Corpuscle Merkel’s Discs |
Aβ Fibers | Spinothalamic |
| Pressure |
Pacinian Corposcles |
Aβ Fibers | |
| Pain / Pin Prick |
Free Nerve Endings |
Aδ Fibers (Nociceptors of Neospinothalamic Tract) C Fibers (Nociceptors of Paleospinothalamic Tract) |
|
| Temperature |
Thermoreceptors |
Aδ Fibers (Cold Receptors) C Fibers (Warmth Receptors) |
|
| Vibration |
Meissner’s Corpuscle Pacinian Corposcles |
Aβ Fibers | Dorsal Column |
| Proprioception |
Muscle Spindle Ruffini Endings |
Aβ Fibers | |
| Touch Localization |
Meissner’s Corpuscle Merkel’s Discs |
Aβ Fibers | |
| Stereognosis | Hemispheric | ||
| Graphesthesia |
- Light Touch
Light touch allows us to be aware of tactile stimuli and has a role in warning us of impending damage.
- Pain / Pin Prick
Pain provides a mean to alert the body that tissue damage has occurred, although pain can be elicited without tissue damage..
- Two Point Discrimination
Two point discrimination is the ability to identify two objects in contact with the skin as two discount points, rather than 1.
- Proprioception
Proprioception is the sense of the relative position of body segments in relation to other body segments. Unlike the six exteroceptive senses (sight, taste, smell, touch, hearing and Balance) by which we perceive the outside world, and interoceptive senses, by which we perceive the pain and the stretching of internal organs, proprioception is a third distinct sensory modality that provides feedback solely on the status of the body internally. It is the sense that indicates whether the body is moving with the appropriate effort and where the various segments of the body are located in relation to each other. Read more about
- Temperature
Temperature, like pain provides a mean to alert the body to potential tissue damage
- Vibration
The appreciation of vibration, a form of pressure sense; most acute when a vibrating tuning fork is applied over a bony prominence.It should also be remembered that vibration sense is diminished in the older person.
- Vision
Vision plays an important role in balance and movement, therefore any deficits may have a huge impact on functional activities. As many as 40% of individuals with Stroke will present with visual deficits post-Stroke.
Functional ActivitiesAssessment of functional daily living activities are vital to ensure the patient receives the level of upport required on the ward at each given stage within their rehabilitation and also provides assistance with goal setting and treatment plans.
- Bed Mobility
- Transfers
- Sitting Balance
- Standing Balance
- Upper Limb Function
- Lower Limb Function
- Mobility
- Stairs
Video
References
References will automatically be added here, see adding references tutorial.
- ↑ 1.01.1 Ryerson S, Neurological Assessment: The Basis of Clinical Decision Making. In: Lennon S, Stokes M, editors. Pocketbook of Neurological Physiotherapy. Elsevier Health Sciences; 2008 Oct 10.
- ↑ Bernhardt J, Hill K. We Only Treat What It Occurs to us to Assess: The Importance of Knowledge-based Assessment. Science-based Rehabilitation: Theories into Practice. 2005:15-48.
- ↑ 3.03.1 Tempest et al., Enhanced Clarity and Holism: The Outcome of Implementing the ICF within an Acute Stroke Multidisciplinary Team in England, 2013, Disability and Rehabilitation, 35:22, 1921-1925
- ↑ Rehab Scales. The International Classification of Functioning, Disability and Health (ICF). ↑ 5.005.015.025.035.045.055.065.075.085.095.10 Jones K. Neurological Assessment: A Clinician’s Guide. Elsevier Health Sciences; 2011 Nov 29.
- ↑ Gardiner MD. The Principles of Exercise Therapy. Bell; 1957.
- ↑ Porter S. Tidy’s Physiotherapy. Edinburgh: Churchill Livingstone, 2013.
- ↑ Brodal P. The central nervous system: structure and function. Oxford University Press; 2004.
- ↑ Lance JW. Symposium synopsis. In: Feldman RG,fckLRYoung RR, Koella WP (eds). Spasticity: Disordered Motor Control. Chicago, IL: Year Book 1980:485–94.