Definition/Description
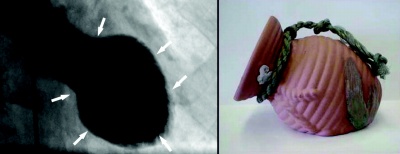
Takotsubo cardiomyopathy occurs when there is an abnormal contraction of the transient left ventricle, creating a balloon shape appearance initially during systole. The Japanese first described the heart condition around 1991. The shape of the heart resembles a Japanese octopus trapping pot with a rounded bottom and narrow neck; hence the name tako-tsubo.[1]
Image depicting resemblance between heart during contraction phase in patient with TC (on left) and Japanese takotsubo (on right)[2]
Typically an intense emotional stress can trigger this type of event. High levels of catecholamines are present in these patients and can cause the heart to be stunned temporarily. This is a reversible cardiomyopathy and clinically presents as a myocardial infarction. Individuals that experience this may or may not have a cardiovascular disease.
Other names include:
- Broken heart syndrome
- Ampulla cardiomyopathy
- Stress cardiomyopathy
- Apical ballooning syndrome (ABS)
- Acute left ventricular ballooning[1]
Prevalence
Takotsubo cardiomyopathy is a very rare condition and has to be differentiated from myocardial infarct. The incidence of takotsubo cardiomyopathy is 1-2% in patients diagnosed with MI. These individuals are usually postmenopausal females (90%). The average age is 62-75 years old. There are approximately 7,000-14,000 cases of takotsubo cardiomyopathy in the U.S.[3]
Characteristics/Clinical Presentation
Usually takotsubo cadiomyopathy is triggered by emotional stress, physical stress, non-cardiac surgery or procedure (refer to table). The onset is insidious and presents with chest pain at rest.
| Table I. Stressors reported to trigger ABS[3] Emotional stress Death or severe illness or injury of a family member, friend, or pet Receiving bad news—diagnosis of a major illness, daughter’s divorce, spouse leaving for war Severe argument Public speaking Involvement with legal proceedings Financial loss—business, gambling Car accident Surprise party Move to a new residence Physical stress Non-cardiac surgery or procedure—cholecystectomy, hysterectomy Severe illness—asthma or chronic obstructive airway exacerbation, connective tissue disorders, acute cholecystitis, pseudomembranous colitis Severe pain—fracture, renal colic, pneumothorax, pulmonary embolism Recovering from general anesthesia Cocaine use Opiate withdrawal Stress test—dobutamine stress echo, exercise sestamibi Thyrotoxicosis |
Signs and Symptoms of Takotsubo include:[3][4]
- Chest pain
- Dyspnea
- Hypotension
- Syncope
- Mild to moderate HF
- Pulmonary edema
- Lab Changes
- Modest increase in troponin T levels
- Increase in creatine phosphokinase (CPK)
- Elevation in pBNP
- High levels of serum catecholamines
The most common signs and symptoms are chest pain and dyspnea; resembling a myocardial infarction.
Associated Co-morbidities
Research has not shown any comorbidities linked with TC.
Medications
There have not been any randomized control trials done to assess medical therapies used for TC. During left ventricular dysfunction, angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers are given. Beta-blockers are also given for long-term treatment to maybe reduce the risk of another episode.
Some medications include:[5]
- Salicylate- inhibit platelet aggregation
- Antianginal Agents- reduce blood pressure
- Anagesics- pain control
- Anticoagulants- inhibit thrombogenesis
- Low Molecular Weight Heparins- inhibit thrombogenesis
- Antiarrhythmic Agents- reduce episodes of chest pain.
- Platelet Aggregation Inhibitors- reduce platelet aggregation
- Loop Diuretics- reduce blood pressure
- Thiazide Diuretics- reduce blood pressure
- Antihypertensive Agents- reduce blood pressure
- Antiplatelet Agents- inhibit platelet aggregation
- ACE Inhibitors- control blood pressure
- Beta-adrenergic Blockers- reduce blood pressure
- Calcium Channel Blockers- improve oxygen delivery to myocardial tissue
Diagnostic Tests/Lab Tests/Lab Values
Diagnostic tests used for TC include lab values, echocardiography, cardiac angiography, and electrocardiography.
Lab Values[5]
Troponin T level:
- Mean value of healthy individuals = 0.49 ng/mL,
- Mean peak value of patients with TC = 0.64 ng/mL
Troponin I level:
- Mean value of healthy individuals = 4.2 ng/mL
- Mean peak value of patients with TC = 8.6 ng/mL
Brain natriuretic peptide level is elevated
Catecholamines are elevated in the acute phase
Echocardiography[5]
An echocardiography is used when diagnosing wall-motion abnormalities. The heart will show hypokinesis or akinesis of the middle and apical segment of the left ventricle if the diagnosis is TC.
Cardiac Angiography[5]
The test will show normal coronary arteries in patients with TC.
Electrocardiography (EKG) Changes[4]
Generally, patients could have 4 different EKG changes:
- ST-segment elevation
- T-wave inversion
- Abnormal Q waves
- QT segment prolongation
In a study conducted by Mitsuma et al, they showed that EKG changes could occur in phases:
- ST-segment elevation (immediately)
- T-wave inversion (days 1-3)
- Improvement in T-wave inversion (days 2-6)
- Deeper T-wave inversion
Diagnostic Criteria[4]
Must have all 4 criteria to be diagnosed with ABS
• Transient hypokinesis, akinesis, or dyskinesis of the LV midsegments
• Absence of obstructive coronary artery or angiographic evidence of acute plaque rupture
• New EKG abnormalities or elevated cardiac troponin
• Absence of recent head trauma, intracranial bleeding, pheochromocytoma, myocarditis, and hypertrophic cardiomyopathy
Etiology/Causes
Research has shown three possible causes of takotsubo cardiomyopathy: increased levels of catecholamines, left ventricular outflow tract (LVOT) obstruction, and microcirculation dysfunction.
- Catecholamines (norepinephrine, epinephrine, and dopamine): In individuals with suspected TC, catecholamines are 7 to 34 times higher than the values of normal individuals. The catecholamine levels are also 2 to 3 times greater than with individuals diagnosed with a myocardial infarction. These levels stay elevated for 7 to 9 days following the episode.[6] TC can develop due to high doses of epinephrine. There are also more catecholamine-sensitive receptors in the apex of the heart, making it more sensitive to increased levels.[7]
- LVOT obstruction: It could be linked to the increased catecholamine levels and occurs in approximately 25% of patients with TC.[8] Other factors that lead to this obstruction are mid-ventricular septal thickening (common in elderly women), increased ventricle wall stress, increased filling pressure, and decreased systemic blood pressure.[9] This obstruction can result in myocardial ischemia and “stunning” of the heart due to the increased oxygen demand and decreased coronary artery perfusion pressure.
- Microcirculation dysfunction[8][9]: It can involve many vessels and occurs in the majority of patients who present with TC. The dysfunction can either be vasospasms or decreased coronary artery blood flow without any indication of atherosclerosis. The vasospasms could possibly be due to increased stimulation of the B1 receptors. Studies attempted to provoke vasospasms using a chemical and among the studies, only 0-43% patients experienced the effect; therefore, microcirculation dysfunction is a questionable cause of TC.
Systemic Involvement
There are a number of possible complications in patients who present with takotsubo cardiomyopathy. Left-sided congestive heart failure with pulmonary edema, cardiogenic shock, ventricular fibrillation, left ventricular thrombus formation, and left ventricular free wall rupture are all possibilities. Death is included in this list; however, the mortality rate is only 0-8%, and generally less than 2%.[10]
Medical Management
The optimal management of TC has not been established. Current medical management for TC has included medication. Since the disease presents similarly to myocardial ischemia it is important to treat the patient initially with EKG monitoring, aspirin, heparin, and beta-blockers.[3] The medications used are described earlier in the medication section. The main focus is “reducing pain, alleviating anxiety, patient monitoring, and prevention of complications,” and risk of a second event.[3] The patients are monitored to ensure that the disease resolves. After discharge the patient is instructed to follow up with a primary care physician to review medications (chronic beta blockers) and health status.[1]
Physical Therapy Management
Preferred Practice Pattern:
Pattern 6D: Impaired Aerobic Capacity/Endurance Associated With Cardiovascular Pump Dysfunction or Failure
Studies have not investigated the direct effects of physical therapy on the status of patients with TC. Research has demonstrated favorable effects of cardiac rehabilitation on other cardiovascular conditions, including myocardial infarction. A systematic review and meta-analysis examining myocardial infarction by Lawler et al found that “patients randomized to exercise-based cardiac rehabilitation had a lower risk of reinfarction and cardiac mortality…Exercise-based CR had favorable effects on cardiovascular risk factors, including smoking, blood pressure, body weight, and lipid profile.”[11]
One study by Yu et al in 2007 compared a relaxation training group, exercise training group, and control group[12]. Both the relaxation and exercise groups showed significant improvement in psychological and various disease-specific quality of life outcomes compared to the control group. Relaxation training proved better to decrease psychological distress, while exercise training controlled fatigue symptoms.
A later study by Yu et al in 2010 placed 59 of the 121 Chinese patients with chronic heart failure into a relaxation-training program and compared them to a control group[13]. The relaxation training included “two relaxation training sessions, one skill revision workshop, twice daily relaxation self-practice, and biweekly telephone follow-up.” The program had significantly improved the psychological and social health-related quality of life compared to the remaining patients in the control group.
Differential Diagnosis
• Esophageal spasm
• Gastroesophageal reflux disease
• Myocardial infarction
• Myocardial ischemia
• Myocarditis
• Acute pericarditis
• Pneumothorax
• Cardiogenic pulmonary edema
• Pulmonary embolism
• Unstable angina
• Acute Coronary Syndromes
• Angina Pectoris
• Aortic Dissection
• Boerhaave Syndrome
• Cardiac Tamponade
• Cardiogenic Shock
• Cardiomyopathy, Cocaine
• Cardiomyopathy, Dilated
• Cardiomyopathy, Hypertrophic
• Coronary Artery Vasospasm
Case Reports/ Case Studies
Resources
References