Introduction
Positive Expiratory Pressure (PEP) is breathing against resistance, which can be performed either through a device or against pursed lips[2] .
Mechanism of PEP
The increase in pressure is transmitted to airways creating back pressure stenting them during exhalation [3], therefore preventing premature airway closure thus reducing gas trapping [4]. It promotes collateral ventilation, allowing pressure to build up distal to the obstruction[3] . Not only does PEP retains airways from collapsing and prolongs expiratory flow, it is effective airway clearance promoting movement of mucus proximally [4].Collateral ventilation is a phenomenon found in the human lungs where alveolar structures are ventilated through channels that bypass normal airways[5]
Types of PEP
Some literature has described PEP as two types varying in pressure range low and high pressure PEP. Low pressure PEP ranges from 5-20cm H2O at mid-expiration, whereas high-pressure PEP ranges from 26-102cm H2O which is achieved by maximal inspiration followed by performing forced expiratory maneuver into PEP mask[6]. Other sources have described PEP as a three airways techniques that has been developed based on expiratory resistance:- PEP, High Positive Expiratory Pressure (HiPEP), and Oscillatory Positive Expiratory Pressure (OscPEP)[2].
- HiPEP
- Involves breathing against resistance by augmenting expiratory flow using FVC[2].
- Oscillating PEP
- Oscillating PEP is an airway clearance technique, where the person blows all the way out many times through a device[2]. Commonly known by their brand names (Flutter®, Acapella®, AerobikA®, and RC-Cornet®), these types of oscillating PEP devices work in two ways. Firstly, they use resistance to make it more difficult during the breath out, like non-oscillating PEP devices. Oscillating PEP devices also create vibrations when a patient breathes out. The vibrations move mucus from the surface of the airways. After blowing through the device several times, the person will huff and cough to clear the mucus from the lungs.
Indications for PEP
Relative Contraindications for PEP
- Untreated pneumothorax [7]
- Intracranial pressure > 20mm Hg[7]
- Active haemoptysis [7]
- Recent trauma or surgery to skull, face, mouth, or oesophagus[7]
- Patient with acute asthma attack or acute worsening of Chronic Obstructive Pulmonary Disease (COPD) unable to tolerate increased work of breathing [7]
- Acute sinusitis or epistaxis [7]
- Tympanic membrane rupture or other known or suspected inner ear pathology[7]
- Nausea [7]
There are no absolute contraindications to PEP that have been noted by literature
Physiology of PEP
Literature has stated theoretical explanations that discuss the physiology behind PEP therapy and its effects on cardiopulmonary status. The theories are:-
Increasing lung volume FRC and VT
- A progressively temporary increase in FRC has been found to be proportionally correlated when increasing PEP[2]
- An increase in FRC is attained by alteration of breathing pattern that is a product of a decrease in expiratory flow and an increase in expiratory time leading to exhalation of smaller volumes[2].
- lung volume increase is achieved by altering breathing pattern, thereby increasing VT and decreasing respiratory frequency, which is due to an increase in muscle activity of inspiratory and expiratory muscles[2].
- Improved gas exchange is a result of breathing during a prolonged period with normalized lung volumes[2].
Reduction of hyperinflation
- Hyperinflation is a result of air entrapment causing the lungs to over inflate. It is caused by muscle spasm, mucosal inflammation, hyper-secretions, reduced lung elasticity due to destruction of lung parenchyma. If Untreated may lead to inspiratory muscle exhaustion, decreased ventilation, and deficient gas exchange[2].
- PEP reduces expiratory flow, which in return decreases the declining pressure across the airway wall thereby reducing collapse[2]
- Increasing pressure within airways transports EPP centrally and in stable airways therefore stenting them. Reduction of airway collapse increases expired volume leading to additional emptying of lung volume thus lowering FRC and improving ventilation distribution and gas exchange[2].
Airway Clearance
When using HiPEP
- It homogenously mobilize secretions in collapsed airways. It aims towards increasing FRC by recruiting collapsed lung volumes and uses resistance to obtain progressive homogenization emptying of the lungs[2].
- Homogenization is achieved by the facilitation of EPP to move peripherally during expiration avoiding collapsed airways, trapped gas, and atelectasis. This results in reduction of respiratory flow and an increase in expiratory flow combined with an increase in FRC. In doing so secretion is mobilized in closed or collapsed and unreachable parts of the lungs. HiPEP is proven to be an airway clearance technique equally or more effective than PEP[2].
When using OscPEP
- The oscillating property is achieved by bursts and turbulent expiratory airflow due to the opening and closing of the valve. Oscillations during expiration decreases the viscoelasticity properties of mucus, effecting its movement which depends on the oscillating frequency. OscPEP is equally as effective as other Airway Clearance Technique (ACT) as PEP and Active Cycle Breathing Technique (ACBT)[2].
Different PEP devices
PEP therapy may be applied through:
Face mask with a one-way valve to which expiratory resistors are attached or face-mask connected to a plastic ring drilled by holes of different caliber that act as resistors. Both devices could be suited to mouthpiece application if necessary. These systems are considered to be flux-dependent.
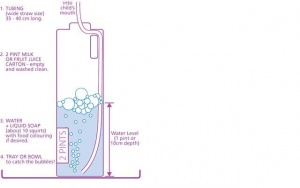
A very common threshold-dependent system is “PEP Bottle” or bubble PEP that consists of a bottle filled with a predetermined quantity of water in which a tube that draws from the bottom. Patient blows into the tube and has to overcome the pressure opposed by the level of water until bubbles are produced.
PEP may also be applied tighter with vibrations with oscillating PEP (OscPEP) devices .
Aerobika® , Acapella®, VibraPEP®, vPEP® are flux-dependent plastic-made devices with a general mechanism of opening and vibrating.
OscPEP can also be applied with a threshold-dependent mechanism with a high density steel “movable ball” that is interposed on a funnel or circular cone between the exhalation tract of the device causing a vibration that is transmitted to the lungs (examples are PARI O PEP®, Flutter® , TurboForte®, PEPE).
==Instructions for the use of PEP devices
- Treatment can be carried out in sitting or any postural drainage position (where possible).
- Relax your stomach muscles and take a few normal breaths before using the PEP device.
- Close your lips around the mouthpiece of the PEP device, making sure there is a good seal.
- Take a slightly bigger breath in through your nose and then blow out through the PEP device. You may feel vibrations on your chest wall.
- Repeat eight to 10 times.
- Following this you should put the PEP device down and do huffing and coughing to clear any sputum. You should then have a period of relaxed breathing before continuing.
This cycle should continue for 10-20 minutes or until you have cleared all your sputum.
Instructions for PEP devices may vary. Please see manufacturers instructions.
==Scientific literature about PEP
“Using positive expiratory pressure physiotherapy to clear the airways of people with cystic fibrosis” – Cochrane review[13]
- Following meta-analyses of the effects of PEP versus other airway clearance techniques on lung function and patient preference a cochrane review demonstrated that there was a significant reduction in pulmonary exacerbations in people using PEP where exacerbation rate was a primary outcome measure.
“PEP therapy in bronchiectasis” – Cochrane review[14]
- PEP therapy appears to have similar effects on health related quality of life, symptoms of breathlessness, sputum expectoration, and lung volumes compared to other ACTs when prescribed within a stable clinical state or during an acute exacerbation.
“Chest physiotherapy with positive expiratory pressure breathing after abdominal and thoracic surgery: a systematic review”[15]
- This review has investigated the effect of PEP breathing after an open upper abdominal or thoracic surgery.
- Questionable quality standards, different protocols and PEP devices used among the six RCTs included concur to uncertainty about PEP effect. It is not possible to assume that a prophylactic chest physiotherapy treatment is superior to a PEP device protocol in preventing within five-days postoperative complications.
References
- ↑ ↑ 2.002.012.022.032.042.052.062.072.082.092.102.112.122.132.142.152.162.172.182.192.20 Fagevik Olsén M, Lannefors L, Westerdahl E. Positive expiratory pressure e Common clinical applications and physiological effects.Respiratory Medicine.2015;105(3):297- 307.
- ↑ 3.03.1 Frownfelter DL, Dean E. Cadiovascular and Pulmonary Physical Therapy: Evidence and Practice 4th ed.St. Louis, Mo. : Mosby/Elsevier, 2006.
- ↑ 4.04.1 Darbee JC, Ohtake PJ, Grant BJ, Cerny FJ. Physiologic evidence for the efficacy of positive expiratory pressure as an airway clearance technique in patients with cystic fibrosis. Phys Ther. 2004;84(6):524-37.
- ↑ Cetti EJ, Moore AJ, Geddes DM. Collateral ventilation.Thorax. 2006;61(5):371-373
- ↑ Myers TR. Positive Expiratory Pressure and Oscillatory Positive Expiratory Pressure Therapies. Respiratory Care. 2007;52(1):1308-1327.
- ↑ 7.007.017.027.037.047.057.067.077.087.097.107.11 Sills JR. Airway Clearance Therapy.The Comprehensive Respiratory Therapist Exam Review. 6th ed. St. Louis, Missouri : Elsevier, 2016
- ↑ 8.08.18.2 PARI PEP S-System. Available from: ↑ 9.09.1 TheraPEP® PEP Therapy System. Available from: ↑ Positive Expiratory Pressure Therapy using PARI PEP. Available from:↑ Positive Expiratory Pressure Therapy using Thera PEP. Available from:↑ Bubble PEP (Positive Expiratory Pressure). Cincinnati Children’s. Available from:↑ McIlwaine M, Button B, Dwan K. Positive expiratory pressure physiotherapy for airway clearance in people with cystic fibrosis. Cochrane Database of Systematic Reviews 2015; (6): CD003147. DOI: 10.1002/14651858.CD003147.pub4
- ↑ Lee AL, Burge AT, Holland AE. Positive expiratory pressure therapy versus other airway clearance techniques for bronchiectasis. Cochrane Database of Systematic Reviews 2017;(9): CD011699. DOI: 10.1002/14651858.CD011699.pub2
- ↑ Örman J, Westerdahl E. Chest physiotherapy with positive expiratory pressure breathing after abdominal and thoracic surgery: a systematic review. Acta Anaesthesiologica Scandinavica. 2010; 54(3): 261-267.