Introduction
Diuretics help rid your body of sodium and water. Most work by making your kidneys release more sodium into the urine. The sodium then takes water with it from your blood decreasing the amount of fluid flowing through your blood vessels hence lowering blood pressure. Diuretics are used effectively in the management of hypertension, and are typically prescribed because of their efficacy, low cost, and low side effects profile. Diuretics are known for their ability to increase the formation and excretion of urine. The increase in excretion allows for more water and sodium to be removed, and ultimately affects the vascular system by leading to a decrease in fluid volume.[1] The decrease in fluid volume affects blood pressure directly, which is why they are effective in reducing high blood pressure.
Pharmacodynamics
There are three different groups of diuretics, these include thiazide diuretics, loop diuretics, and potassium-sparing diuretics. Potassium diuretics are used in congestive heart failure and are discussed here.
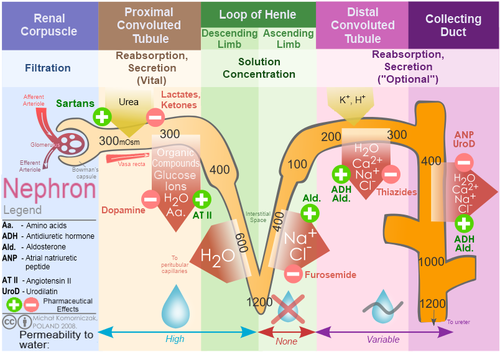
In this article we will be focusing specifically on Thiazide and Loop diuretics. The primary site of action for diuretics is the nephron within the kidneys. The different classes of diuretics are characterized by their various mechanism of action and specific location targeted within the nephron.
- Thiazide diuretics act on the distal tubule of the nephron by inhibiting sodium reabsorption. With this inhibition, more sodium stays within the nephron creating an osmotic force that allows for water retention in the nephron, and ultimately water excretion.[2] Thiazide diuretics are considered the drug of choice for long term treatment of hypertension by many physicians.[3]
- Loop diuretics, like thiazide diuretics, work to inhibit the reabsorption of sodium as well as chloride by targeting a sodium potassium chloride cotransporter, however they exert their effects in the ascending limb of the loop of Henle. By targeting these two specific electrolytes, loop diuretics prevent water reabsorption. The decrease in plasma volume that occurs in response to an increased sodium excretion reduces venous return and lowers cardiac output.[2]
Pharmacokinetics
All classes of diuretics are absorbed orally and widely distributed. Thiazide diuretics are known to bind extensively to plasma proteins, which limits their filtration and promotes appropriate delivery to tissues. However, they undergo extensive hepatic metabolism which plays into the dose and frequency of administration. The half-life of thiazides is approximately 8 to 12 hours allowing for a single daily dosing.[3] On the other hand, loop diuretics are known to be less effective than thiazides, and have a short duration of action at approximately 6 hours.[3] Loop diuretics are indicated for patients with coexistent renal or heart failure, in circumstances when thiazide diuretics are rarely effective.[1]
Adverse Effects
The adverse effects of diuretics are dose-dependent and are primarily metabolic. The most common adverse effect is electrolyte imbalances such as hypokalemia or hyponatremia and excessive fluid depletion.[4]Hypokalemia is one of the main problems with diuretics and can produce serious metabolic and cardiac issues. Excessive fluid depletion may lead to a reflex increase in cardiac output and vascular resistance due to the baroreceptor reflex being activated. This increased demand on the heart can become an issue for patients, especially those suffering from cardiac disease.[5] Other side effects associated with diuretics are orthostatic hypotension and hyperlipidemia.[6] Diuretics are contraindicated in patients that are diagnosed with gout.[3]
see also Pharmacological Management of Hypertension
References:
- ↑ 1.01.1 Shah SU, Anjum S, Littler WA. Use of diuretics in cardiovascular disease: (2) hypertension. Postgraduate Med J. 2004;80(943):271-276.doi: http://dx.doi.org/10.1136/pgmj.2003.010843.
- ↑ 2.02.1 Laurent S. Antihypertensive drugs. Pharmacological Research. 2017; 124,116-125. doi:10.1016/j.phrs.2017.07.026.
- ↑ 3.03.13.23.3 Ernst ME, PharmD., & Moser M, M.D. (2009). Use of diuretics in patients with HypertensionDrug therapy:N Engl J Med. 2009;361(22):2153-64. doi: http://dx.doi.org/10.1056/NEJMra0907219
- ↑ Sarafidis PA, Georgianos PI, Lasaridis AN. Diuretics in clinical practice. Part II: electrolyte and acid-base disorders complicating diuretic therapy. Expert Opin Drug Saf. 2010;9:259-273.
- ↑ Ciccone CD. Pharmacology in Rehabilitation.6thEdition.Philadelphia, PA: F.A. Davis Company; 2016.
- ↑ Palmar BF. Metabolic complications associated with use of diuretics. Semin Nephrol. 2011;31:542-552.