Definition/Description
Kawasaki disease, also known as mucocutaneous lymph node syndrome[1], is a medium-sized vessel [2].
The prognosis is generally good for patient’s who are able to get treatment early enough, although there is the possibility of serious cardiovascular problems developing later on in life. For those who develop a large aneurysm (diameter larger than 8 mm) have the worst prognosis, as those will probably not regress or resolve. In some patients, severe [1].
Prevalence
Kawasaki Disease can be found in any ethnic group, but is predominately found in the Asian population, more specifically the Japanese[1]. Japanese children under the age of 5 are 10 times more likely to get Kawasaki Disease than Caucasian children of the same age group. The incidence of this disease in Hispanic and African American children falls in the middle. Males are 1.5 times more likely to get Kawasaki Disease than females. In the United States, there are approximately 4,000 diagnosed cases each year[4]. Eighty percent of the cases of Kawasaki Disease are found in children under the age of 5[1]. The most prevalent age group is 18-24 months, and it is rare under the age of 4 months[2].
Characteristics/Clinical Presentation
Kawasaki Disease begins with a fever that lasts for at least 5 days. Along with the fever the child may display irritability, intermittent fatigue, and occasional colicky abdominal aching[2]. During the acute stage, which occurs during the first 2 weeks after onset, there is inflammation of the vascular system and the immune system has been activated. During this time, the arterioles, venules, and capillaries are affected. Later on in the disease the main coronary arteries, the heart, and the larger veins will be affected. Also during the acute phase, there are circulating antibodies that are cytotoxic to vascular endothelial cells, and the anticardiac myosin autoantibodies may be elevated. The elevation of the anticardiac myosin autoantibodies may be responsible for the myocardial damage that occurs[1]. One to 2 days after the start of the fever, [2].
Clinical manifestation[1][2]:
• Acute Phase:
• Abrupt high fever lasting more than 5 days that will not respond to antibiotics or antipyretics
• Extreme irritability
• Fatigue
• Abdominal pain
• Sub-acute Phase:
• Fever resolves
• Irritability continues
• Anorexia
• Rash of the trunk and extremities with a reddened palmar surface of the hands and feet
• Desquamation of the tips of the fingers and toes
• Peripheral edema of the hands and feet
• Pallor of the fingernails and/or toenails
• Cervical lymphadenopathy (typically unilateral)
• Conjunctival infection without exudate (bilateral)
• Changes in the oral mucous membranes, such as erythema, dryness or cracking of the lips, and reddening of tongue
• The following are signs/symptoms found in 1/3rd of all cases:
o Arthalgias
o Gastrointestinal tract symptoms
oCardiac involvement, such as myocarditis, pericarditis, and arteritis. These can predispose one with
Kawasaki Disease to the development of coronary artery aneurysm. This occurs in 25% of the cases
that are not treated within 10 days of the onset of the fever.
• Convalescent Phase:
• All of the clinical signs and symptoms have resolved
• The blood values are still abnormal







Associated Co-morbidities
Currently there are no associated comorbidities with Kawasaki Disease, but there are possible risks that can develop after having the disease. Twenty percent of cases will go on to develop cardiac complications, while there is also a small risk of developing [1][2].
Medications
The medications use to treat Kawasaki Disease include:
• [1][2].
Diagnostic Tests/Lab Tests/Lab Values
The diagnosis of Kawasaki Disease is made based off the clinical signs and symptoms of the patient, laboratory tests, a serial ECG and echocardiogram. There are no specific laboratory tests used to diagnose Kawasaki Disease, but they tend to check the child’s [1][2].
Criteria for diagnosing Kawasaki Disease[2]:
• The diagnosis is made if the child has a fever 5 or more days and if 4 of the following 5 conditions are met:
• Bilateral non-exudative conjuntival infection
• Changes in the lips, tongue, or oral mucosa (infection, drying, fissuring, red strawberry tongue)
• Changes in the peripheral extremities (edema, erythema, desquamation)
• Polymorphous truncal exanthema
• Cervical lymphadenopathy (at least 1 node > 1.5 cm in diameter)
[2].
Etiology/Causes
The cause of this disease is currently unknown, but due to seasonal and geographic outbreaks, there is thought to be an infectious etiology. The infectious cause is thought to be an immunologic reaction to an “infectious, toxic, or antigenic substance”[1]. It is proposed that a genetically predisposed child comes in contact with an infection or has an abnormal immunologic response to an infection, and that combination causes Kawasaki Disease[1].
Systemic Involvement
The main effects of Kawasaki Disease on the child’s body include[1][2]:
• Fever
• Fatigue
• Stomach pain
• Vascular inflammation
• Bulbar conjunctiva
• Skin rash
• Red tongue
• Dry, cracked, and fissured lips
• Red-purple and swollen palms of the hand and soles of the feet
• Desquamation of the palms of the hands, soles of the feet, perineal region, and periunguinal region
• Swollen and tender lymph nodes
• Cardiac complications
For more information, refer to the “characteristics/clinical presentation” section.
Medical Management (current best evidence)
The coronary artery involvement can be controlled by the use of high-dose IV immune globulin (IVIG) along with high-dose aspirin therapy, which helps lower the fever, control the inflammation throughout the body, and decrease the occurrence of abnormalities of the coronary artery. As the child’s fever goes away or if it has reached day 14 of the disease, the dose of aspirin should be decreased. It is important to monitor the serum aspirin level, especially if the aspirin is taken for 14 days. A smaller dosage of aspirin is typically continued for at least 8 weeks after the disease begins, but will usually be continued indefinitely for children with coronary artery abnormalities. For children with large coronary artery abnormalities other anticoagulant therapy will be needed, such as warfarin or dipyridamole[1][2].
The IVIG therapy can cause a lower response rate to live viral vaccinations, so children who were treated with these medications should not receive any vaccinations for at least 11 months. It is also recommended that children on aspirin therapy receive the yearly influenza vaccination, as there is a small risk of the child developing Reye’s Syndrome due to the aspirin therapy[2].
Physical Therapy Management (current best evidence)
Kawasaki Disease is managed medically and there is no known physical therapy management, but it is possible that a child may come to physical therapy with complaints of joint pain, which is a possible symptom of the disease. It is important for physical therapists to recognize the symptoms of Kawasaki Disease so they are able to refer out when necessary.
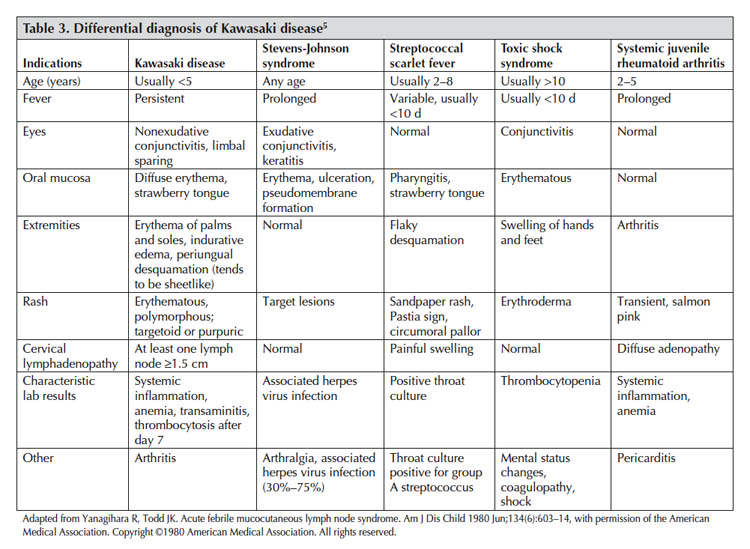
Differential Diagnosis
The following must be cleared before diagnosing Kawasaki Disease[12][13][14]:
• Measles
• Scarlet fever
• Toxic shock syndrome
• • Juvenile rheumatoid arthritis
• Systemic lupus erythematosis
•
Case Reports/ Case Studies
Resources o Kawasaki Disease Foundation-www.kdfoundation.org
o American Heart Association-www.americanheart.org
o Department of Pediatrics at the University of California, San Diego-www.pediatrics.ucsd.edu/Kawasaki
o Kawasaki Disease Foundation of South Africa-www.kawasakidiseasefoundation.co.za/
o Kawasaki Disease Canada Parent Awareness Group-www.kdcanada.ca/news.php
o Vasculitis Foundation-www.vasculitisfoundation.orgReferences