This article is currently under review and may not be up to date. Please come back soon to see the finished work! (26/05/2019)
Discussion & Background
The purpose of this clinical guideline is to describe the evidence based physical therapy practice including diagnosis, prognosis, intervention and assessment of outcome for musculoskeletal disorders related to hip osteoarthritis that are commonly managed with orthopaedic physical therapy techniques.
More specifically, in the paragraphs that follow, there will be a review of recommendations related to: diagnosis and classification, examination, and treatment/interventions. These recommendations will be supported with a grade of evidence based on Guyatt et al[1], as modified by MacDermid.In this modified system, the typical A, B, C, and D grades of evidence have been modified to include the role of consensus expert opinion and basic research to demonstrate baseic biological or biomechanical plausibility.[2]
Diagnosis & Classification Recommendations
Diagnosis/Classification (Grade: A)
Moderate lateral or anterior hip pain during weight bearing, in adults over the age of 50 years, with morning stiffness less than 1 hour, with limited hip interanl rotation and hip flexion by more than 15 degrees when comparing the painful to the nonpainful side are useful clinical findings to classify a patient with hip pain into the International Statistical Classification of Diseases and Related Health Problems (ICD) category of unilateral coxarthrosis and the associated International Classification of Functioning, Disability, and Health (ICF) impairment based category of hip pain and mobility deficits.
Risk Factors (Grade: A)
Clinicians should consider the following as risk factors for hip osteoarthritis:
- Age over 50 years
- Hip developmental disorders
- History of previous hip injury
Pathoanatomical Features (Grade: B)
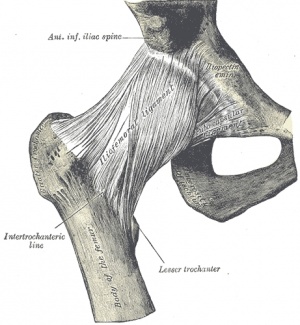
Clinicians should assess for impairments in mobility of the hip joint and strength of the surrounding muscles, especially the hip abductor muscles, when a patient present with hip pain.
Differential Diagnosis (Grade: E)
Clinicians should consider diagnostic classifications other than osteoarthritis of the hip when the patient’s history, reported activity limitations, or impairments of body function and structure are not consistent with those presented in this guideline –or– when the patient’s symptoms are not diminishing with interventions aimed at normalization of the patient’s impairment of body function.
Examination Recommendations
Outcome Measures (Grade: A)
Clinicians should use validated functional outcome measures, such as the Western Ontario and McMaster Universities Osteoarthritis Index, the Lower Extremity Functional Scale, and the Harris Hip Score before and after interventions intended to alleviate the impariments of body function and structure, activity limitations, and participation restrictions associated with hip osteoarthritis.
Activity Limitation and Participation Restriction Measures (Grade: A)
Clinicians should utilize easily reproducible physical performance measures, such as the 6-minute walk, self-paced walk, stair measure, and timed up-and-go tests to assess activity limitation and particpation restrictions associated with their patient’s hip pain and to assess the changes in the patient’s level of function over the episode of care.
Intervention & Treatment Recommendations
Patient Education (Grade: B)
Clinicians should consider the use of patient education to teach activity modification, exercise, weight reduction when overweight, and methods of unloading the arthritic joint.
Manual Therapy (Grade: B)
Clinicians should consider the use of manual therapy procedures to provide short-term pain relief and improve hip mobility and function in patients with mild hip osteoarthritis.
Flexibility, Strengthening, and Endurance Exercise (Grade: B)
Clinicians should consider the use of flexibility, strengthening, and endurance exercises in patients with hip osteoarthritis.
Functional, Gait, and Balance Training (Grade: C)
Functional, gait, and balance training, including the use of assistive devices such as canes, crutches, and walkers, can be used in patients with hip osteoarthritis to improve function associated with weight-bearing activities.
References
- ↑ Guyatt G, Sackett D, Sinclair J, Hayward R, Cook D, Cook R. Users’ guides to the medical literature. IX. A method for grading health care recommendations. Evidence-Based Medicine Working Group. JAMA. 1995;274:1800-1804.
- ↑ Cibulka MT, White DM, Woehrle J, et al. Hip pain and mobility deficits–hip osteoarthritis: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2009;39(4):A1-25.