Definition/Description
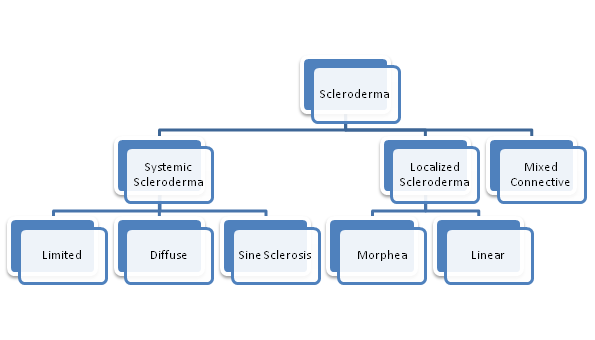
- Scleroderma is a connective tissue disease that involves changes to the skin, and can also involve changes to the blood vessels and internal organs.[1] It is a chronic, progressive autoimmune disorder where inflammation and the overproduction of collagen accumulate in the body.[2] There are two main types of Scleroderma- Systemic and Localized.
Systemic Scleroderma may affect the skin and multiple systems such as the integumentary, cardiopulmonary, vascular, gastrointestinal, genitourinary, or musculoskeletal. There are three forms of Systemic Scleroderma.
- With Diffuse Scleroderma skin thickening occurs more rapidly and involves more skin areas than in limited. In addition, people with diffuse scleroderma have a higher risk of developing “sclerosis” or fibrous hardening of the internal organs.[3]
- Sine Scleroderma involves organ fibrosis with no skin involvement. This is rare. [4]
- With Limited Scleroderma (includes CREST syndrome) skin thickening is less widespread, typically confined to the fingers, hands and face, and develops slowly over years. Internal problems occur, but they are less frequent and tend to be less severe than in diffuse scleroderma.[3] CREST is an acronym using the letters of the conditions involved; Calcinosis, Raynaud’s, Eosophageal dysmotility, Sclerodactyly and Telangiectasia. The video below gives some good examples of these.
Localized Scleroderma usually affects the skin and related tissues in part of the body. [1]Two of the main types of Localized Scleroderma are below [5]
- Morphea is characterized by waxy patches on the skin of varying sizes, shapes and color. The skin under the patches may thicken. The patches may enlarge or shrink, and often may disappear spontaneously within three to five years.[3][1]In some, rare, cases muscle weakness may be associated.
- Linear Scleroderma starts as a streak or line of hardened, waxy skin on an arm or leg or on the head and neck. Linear scleroderma tends to involve deeper layers of the skin as well as the surface layers, and sometimes affects the motion of the joints, which lie underneath.[3]
Mixed Connective Tissue Disease or Scleroderma Overlap syndrome is when Scleroderma is diagnosed when another disease, such as systemic lupus erythematosus and polymyositis, has been previously diagnosed.[1][6]
Prevalence
Estimates vary. Some estimates predict that about 300,000 Americans have scleroderma.[7] Some predict 75,000 to 100,000 [4]It is more common in females than males, and between the ages of 20 to 50 [4]
Thirty percent of those with scleroderma have the systemic form of scleroderma. This type appears to be more common in adults. Localised scleroderma is more common in children.[4][5]
Those with a family member who has scleroderma, or another autoimmune disease such as lupus, may have a slightly higher risk of developing scleroderma. [7]
Race and ethnic background, may influence the risk of getting scleroderma, the age of onset, and the pattern or severity of internal organ involvement. Choctaw Native Americans and African-Americans are more likely than Americans of European descent to develop the type of scleroderma that affects internal organs.[2]
Diagnostic Tests/Lab Tests/Lab Values[1][7]
A diagnosis of scleroderma can be difficult because symptoms may be similar to that’s of other disease. Diagnosis will be based on the
- medical history
- physical examination. See below for symptoms of ‘Systemic Involvement’
- X-rays and CT for bony investigations
- MRI and US for soft tissue examiantion
- Lab tests can also confirm a suspected diagnosis.[8]
-
- Topoisomerase-1 antibody or Scl-70 antibodies is a marker of systemic sclerosis.
- Anticentromere antibodies, or ACA, is a marker of CREST
- ESR is found to be increased in those with disease activity or relapse
- AMF is positive in those with Mixed Scleroderma
Not all people with scleroderma have these antibodies and because not all people with the antibodies have scleroderma, lab test results alone cannot confirm the diagnosis.
A skin biopsy (the surgical removal of a small sample of skin for microscopic examination) can aid in or help confirm a diagnosis.
Diagnosing scleroderma is easiest when a person has typical symptoms and rapid skin thickening. In other cases, a diagnosis may take months, or even years, as the disease unfolds and reveals itself and as the doctor is able to rule out some other potential causes of the symptoms.
Etiology/Causes
The cause of scleroderma is unknown, but it cannot be transmitted from person to person. Several factors that may increase a person’s risk of getting scleroderma include:
Abnormal immune or inflammatory activity: In scleroderma, the immune system is thought to stimulate cells called fibroblasts so they produce too much collagen. People who already have rheumatic or autoimmune disorders are at increased risk due to previous abnormal autoimmune activity[5]
Genetic makeup: Although genes seem to put certain people at risk for scleroderma and play a role in its course, the disease is not passed from parent to child like some genetic diseases. Research indicates that variations in genes relating to the the body’s immune system, such as those in the HLA-complex, IRF5 and STAT4, may increase the risk of developing scleroderma. [3][1][6]
Environmental triggers: Research suggests that exposure to some environmental factors may trigger scleroderma-like disease in people who are genetically predisposed to it. Suspected triggers may include viral or bacterial infections [5][1][6]
Hormones: Women develop scleroderma more often than men. Scientists suspect that hormonal differences between women and men play a part in the disease. However, the role of estrogen or other female hormones has not been proven.[1][2]
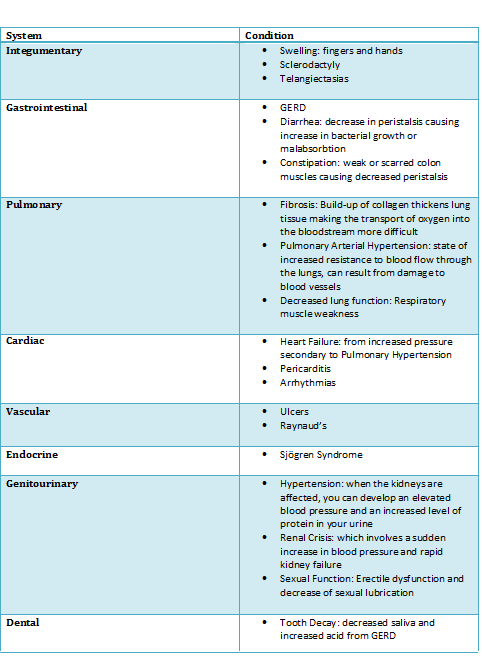
Systemic Involvement [2][3]
Medical Management [1][2]
Currently, there is no treatment that controls or stops the underlying problem—the overproduction of collagen—in all forms of scleroderma. Treatment and management focus on relieving symptoms and limiting damage.
Several different specialists may be involved in the care of one person since scleroderma can affect many different organs and organ systems. Typically, care will be managed by a rheumatologist, who may refer the patient to other specialists, depending on the specific problems they are having.
These specialists can include:
• Dermatologist for the treatment of skin symptoms
• Nephrologist for kidney complications
• Cardiologist for heart complications
• Gastroenterologist for problems of the digestive tract
• Pulmonary specialist for lung involvement
Medications used to treat scleroderma may include : [7][9]
- Anti-inflammatory medicines esuch as corticosteroids
- Immune-suppressing medications such as methotrexate and cytoxan.
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
Scleroderma can affect many different organs and organ systems. Additional medications are based on the symptoms that the individual experiences.
Examples of other treatments for specific symptoms include:[7][9]
- Medicines for heartburn or swallowing problems – antacid drugs, especially proton- pump inhibitors
- Blood pressure medications (particularly ACE inhibitors) for high blood pressure or kidney problems
- Light therapy to relieve skin thickening
- Cyclophosphamide and mycophenolate can be effective in treating interstitial lung disease
- Medications to treat pulmonary hypertension include prostacyclin-like drugs, endothelin receptor antagonists and PDE-5 inhibitors. These work to open up the blood vessels in the lungs.
- Medications to treat Raynaud’s phenomenon- calcium channel blockers, PDE-5 inhibitors to open up narrowed blood vessels and improve circulation.
- Intestinal dysfunction
- Medicines to increase saliva secretion in the mouth to reduce effects of Sjogren’s Syndrome (a chronic autoimmune disease in which a person’s white blood cells attack their moisture-producing glands)
Physical Therapy Management/Other[1][2]
Physical therapy can be very beneficial in the treatment of scleroderma. Physical therapists/ Physiotherapists, together with other health professionals such as Occupational Therapists, can design a program of regular stretching and gentle exercise to help:
• Manage pain
• Improve strength
• Improve/maintain mobility
• Minimize joint contractures
• Improve circulation. Education re protecting vulnerable skin areas and keeping them warm
• Enhance/maintain performance of activities of daily living in order to encourage independence
Other health professionals such as psychologists, and social workers may play a role in patient care.[1][3]
Dentists, orthodontists, and speech therapists may be involved in the management of complications that arise from thickening of mouth and face tissues. [1]
Research about the most effective management and treatment is ongoing.
Differential Diagnosis[10]
A number of other diseases have symptoms similar to those seen in scleroderma.
These include:
Eosinophilic fasciitis (EF): This rare disease involves the fascia, the thin connective tissue around the muscles. The fascia becomes swollen, inflamed and thick. The skin on the arms, legs, neck, abdomen or feet can be involved. Unlike scleroderma, the fingers are not involved. A skin biopsy distinguishes between the two diseases.
Nephrogenic Systemic Fibrosis: An uncommon disease of fibrosis of the skin and organs, caused by gadolinium exposure ( used in imaging) in those patients with renal insufficiency.
Generalized scleroderma-like skin thickening: This may occur with scleromyxedema, graft-versus-host disease, porphyria cutanea tarda, and human adjuvant disease
Raynauds phenomena: This may occur in isolation, as well as part of the scleroderma disease process.
Case Reports/ Case Studies
References
Careta MF, Romiti R. Localized scleroderma: clinical spectrum and therapeutic update. Anais Brasileiros de Dermatologia. 2015;90(1):62-73. doi:10.1590/abd1806-4841.20152890 ( accessed 18 March 2018)
Ola!
Como podemos ajudar?