Definition/Description
Spondyloarthritis (or spondyloarthropathy, SpA) is a name for a group of diseases that is included in a larger term ‘arthritis’.[1][2][3] It is a diverse group of inflammatory arthritides that share certain genetic predisposing factors and clinical features.
Spondyloarthritis are characterized by involvement of both synovium and entheses (sites where tendons, ligaments or joint capsules attach to the bone) leading to spinal and oligoarticular peripheral arthritis, principally in genetically predisposed (HLA-B27+) individuals.
Inflammation can occur in the spine, sacroiliac and peripheral joints as well near the attachments of tendons and ligaments.[3] This disease provokes to pain, stiffness and fatigue in back, legs and arms as in joints, ligaments and tendons.[4][5]Eruption, eye and intestinal problems may also occur.[1][3]
Spondyloarthritis in adults can be subdivided more specifically:[1][2][6][7][8][1]
Clinically Relevant Anatomy
Spondyloarthritis is the overall name for a family of inflammatory rheumatic diseases. [1][2]
Due to this fact, there is a large complexity. This is because there are several anatomic structures involved. We can assume that the inflammation can occur on all the joints of the spine. The facet joints, endplates, bone marrow, … every part of the spine can be affected by an inflammation. [9] Sacroiliitis in SpA is characterized by involvement of different joint structures. Whereas the iliac and the sacral side of the sacroiliac joints are almost equally affected, the dorsocaudal synovial part of the joint is involved significantly more often than the ventral part, especially in early disease. Sacroiliac enthesitis is not a special feature of early sacroiliac inflammation. There is a difference between axial and peripheral spondyloarthitis, with axial spondyloarthitis back pain and inflammation of the sacroiliac joints are the main complaints. In peripheral spondyloarthritis, the inflammation of peripheral joint and tendons are the main complaints. Further, spondyloarthritis can show an inflammation of peripheral joints (for example, knees and ankles), and tendons (for example, the Achilles tendon).[1][2][3][9]
Epidemiology /Etiology
Spondyloarthritis is a pathology that specifically strikes young people.[10] The symptoms most frequently start before the age of 45. [2] It affects more males than females. [5][4]
Predisposition to spondyloarthritis, especially SpA, is determined largely by genetic factors. The incidence rate is higher in populations with a higher prevalence of HLA-B27.[6] Psoriatic skin lesions and colitis due to inflammatory bowel disease (IBD) have been considered as both basic, subtype-defining entities with their own genetic background (distinct from HLA-B27 genotype), and as manifestations of spondyloarthritis.[6] There is a strong need to diagnose patients with SpA in an earlier stage; currently there is a delay of 5–10 years between onset of the first symptoms and diagnosis.[6][4]
Characteristics/Clinical Presentation
Symptoms that may occur with spondyloarthritis are pain, stiffness and fatigue in the back, legs and arms. There are no typical characteristics, because spondyloarthritis characterises with more than one symptom. We see that significantly more women have knee pain as presenting symptom.[3][10][11][12] and we can assume that severity of symptoms can vary between individuals[13]. Here are the most common characteristics.[2][11][12][12][14]
- back pain
- osteoporosis
- spinal fractures
- peripheral arthritis, usually asymmetric, relatively more in the lower limbs.[2][3][2]
- enteritis
- dactylitis
- inflammation of the heart valve – pneumonia
- extra articular disorders such as uveitis, skin porosiasis or inflammatory bowel disease
- strong familial aggregation of spondyloarthritis, psoriasis, IBD, uveitis
- association with HLA-B27
- no increased CRP and rheumatoid factor
Differential Diagnosis
The disease starts with hip or low back pain. The most common symptom is intermittent pain that progressively gets worse thoughout the day, in the morning, and following intensive activity. [1] Most patients experience back pain in the sacroiliac joints. However, pain can involve all the parts of the spine. Pain relief is sometimes achieved by bending over. It is possible that a patient is not able to fully expand the chest due to the involvement of the joints between the ribs.
Diagnostic Procedures
Antecedents and physical examination are the major factors leading to diagnosis, although radiologic evidence of sacroiliitis is very helpful [2][7] In the early-1990s, two classification criteria, Amor and the European Spondyloarthropathy Study Group (ESSG), were proposed for diagnosing SpA [2][3] All criteria developed so far (including the ESSG and Amor criteria) were developed as classification criteria, although they are often used as diagnostic criteria [7][8]
Amor criteria for spondyloarthritis [5]:
| Paramters | Scoring | |
|---|---|---|
| Clinical symptoms or past history of | ||
|
Lumbar or dorsal pain at night or morning stiffness of lumbar or dorsal region |
1 | |
| Asymmetric oligoarthritis | 2 | |
|
Buttock pain |
1 2 |
|
| Sausage-like toe or digit | 2 | |
| Heel pain or other well- defined enthesitis | 2 | |
| Iritis | 2 | |
| Non- gonococcal urethritis or cervicitis within 1 month before the onset of arthritis |
1 |
|
| Acute diarrhoea within 1 month befor the onset of arthritis | 1 | |
| Psoriasis, balanitis or inflammatory bowel disease ( ulcerative colitis or chrohn’s disease) | 2 | |
| Radiological findings | ||
| Sacroiliitis (bilateral grade 2 or unilaterale grade 3) | 3 | |
| Genetic background |
||
| Presence of HLA-B27 or family history of ankylosing spondylitis, reactieve arthritis, uveitis, psoriasis or inflammatory bowel disease | 2 | |
| Response to treatment | ||
| Clear- cut improvement within 48 hours after non steroidal anti- inflammatory drug intake or rapid relapse of the pain after their discontinuation | 2 |
A patient is considered to be suffering from spondyloarthritis if the sum is ≥ 6
The need for a standardized, evidence-based approach to spondyloarthritis classification led to the development of the European Spondyloarthropathy Study Group (ESSG) [4] preliminary classification criteria for spondyloarthritis in 1991 [10]:
Inflammatory spinal pain or synovitis (asymmetric, predominantly in lower limbs) and any one of the following: [4]
- Positive family history
- Psoriasis
- Inflammatory bowel disease
- Acute diarrhea or urethritis or cervicitis preceding the arthritis
- Alternate buttock pain
- Enthesopathy
- Radiological sacroilits
Another is the concept of IBP (Low Back Pain), which is defined as the presence of at least four of the following five parameters [1], [6]:
- Age at onset less than 40 years
- Insidious onset
- Improvement with exercise
- No improvement with rest
- Pain at night (with improvement upon getting up).
Studies are under way to define ASAS criteria for nonaxial (peripheral) SpA.
In the ASAS classification criteria, several SpA features are described. These features are called SpA features because they are frequently present in patients with SpA ,[9][6]
The main features of an early diagnosis of any rheumatic disease, including spondyloarthritis, are clinical history, clinical symptoms, clinical examination, laboratory parameters and imaging. [10]
Clinical symptoms:
- Inflammatory back pain
- Arthritis ( swelling, joint effusion, or detected by imaging)
- Accompanying features, including psoriasis, crohn-like colitis and anterior uveitis
Clinical history:
- Family
- Rheumatic symptoms
- Accompanying features
Clinical examination:
- Lateral flexion of the lumbar spine (
- Chest expansion (
- Cervical rotation (
Laboratory parameters:
- HLA-B27
- C- reactive protein
- Erythrocyte sedimentation rate
Imaging:
- Radiography
- MRI
- Ultrasonography
Outcome Measures
Examination
Patients with spondyloarthritis will complain about back pain, fatigue and stiffness. The pain will decrease when the patients exercise, but will persist at they rest. It is common for the patient to have pain at night, this pain can improve when the patients gets out of bed and moves around. (this should improve when they get up).[2][8] The motion of the lumbar spine of the patients will be limited in both the sagittal and the frontal planes. [2]
Psoriasis, finger swelling, Crohn’s disease or ulcerative colitis can be indicative for Spondyloarthritis.
Sacroiliitis grade ≥ 2 bilaterally or grade 3 to 4 unilaterally is suggestive for SpA (grade 0: normal; grade I: some blurring of the joint margins – suspicious; grade II: minimal sclerosis with some erosion; grade III: definite sclerosis on both sides of joint 5 & severe erosions with widening of joint space with or without ankylosis; grade IV: complete ankylosis) [4][5]
There are also active inflammatory and chronic lesions that can be found on a MRI-scan (see images). [3] [6][7]

[3]Sieper et al. The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis
Laboratory testing
- Common presence of human leukocyte antigen-B27
- Elevated C-reactive protein
- Absence of rheumatoid factor [2]
Medical Management
Reliant on your symptoms and how severe your condition is, the doctor can decide what kind of treatment is the best option for the patient.
Medicines such as:
- analgesics (pain-relievers, by example paracetamol)[10]
- non-steroidal anti-inflammatory drugs (NSAIDS, by example naproxen, ibuprofen).[9]
- Anti-rheumatic drugs (DMARDs) have been proven effective in the treatment, but only for the arms and legs, not for the spine and sacroiliac joints.[10]
- Corticosteroids, given by the mouth or injections, can be effective. We must remind ourselves for the side effects, such as osteoporosis and infections.[4]
- Injections of deposteroid in the joints of tendon sheaths are also used for symptomatic relief of the local flares.[4]
- TNF alpha blockers are also effective in both spinal and peripheral joints.[9][10]
- There are three kind of TNF alpha blockers we can use:
- Infliximab (Remicade), given a dose of 5 mg/kg intravenously every sic to eight weeks.
- Etanercept (Enbrel), 25 mg given under de skin twice a week
- Adalimumab (Humira), 40 mg injected, every other week
TNF treatment is expensive and is not without complications, therefore, NSAIDs and DMARD should be tried first.
Surgery:
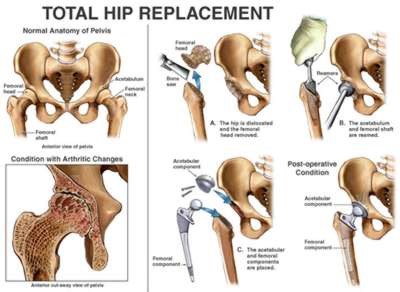
- Total hip replacement is also commonly done[5]
(Example of a total hip replacement, ehealthmd.com/content/what-hip-replacement)
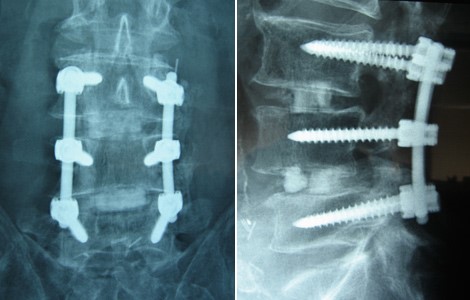
- Surgical spine fusion (when spinal cord or nerve function are compromised) [8]
(Postoperative x-rays anterior-posterior (A) and lateral (B) views demonstrate good pedicle screw placement and fusion at the patient’s six month follow-up., https://www.bnasurg.com/patient-resources-back-pain.php)
( Example of a osteotomy on a women of 40, who has spinal deformities caused by spondyloarthritis,
http://www.scoliosisjournal.com/content/6/1/6/figure/F4)
No specific drugs is considered more superior than another for the treatment of spondyloartritis.
Physical Therapy Management
Apart from a medication treatment, physiotherapy is recommended in spondyloarthritis. [9][3] This physical therapy generally focuses on the exercise regimens whose purpose is to maintain mobility and strength, relieve symptoms, prevent or decrease spinal deformity, and improve overall function and quality of life. [1] The physiotherapy treatment consists mainly of exercise therapy. Evidence level of this therapy? The patients should perform daily special stretching and strengthening exercises to maintain the strength and mobility in the joints and reduce pain and stiffness.[3][3][10] The strengthening exercises help to support and take pressure off sore joints. They also strengthen bones and improve balance. One can use weights or dumbbells for strengthening exercises.
Flexibility training can maintain or even improve mobility of muscles and joints. Therefore major muscle groups such as erector spine, shoulder muscles, hip flexors, hamstrings and quadriceps should be stretched. This can also be done by partaking in yoga.[1][9]
Spa-exercise and balneotherapy programmes have short-term benefits in QoL outcomes; spa-exercise is superior in pain relief, while balneotherapy further improves disease activity.The balneotherapy interventions consist of mineral baths plus mud packs, radon-carbon dioxine baths, carbon dioxine baths, Dead Sea baths and tap water of 36°C. [10]
Unfortunately these benefits diminish or disappear over a period of 6 to 15 months. [1] An addition of aerobic exercise to conventional stretching and mobility home exercise programmes results in superior functional fitness. Walking and swimming are examples of such aerobic exercise. [1][9]
- Swimming: three times a week for six weeks:
- 10 min warm-up + 5 min stretching
- 30 min of swimming at a moderate intensity (60-70% heart rate [HR] reserve – 12 beats/minute)
- 10 min cooling down + 5 min stretching
- Walking: 30 minutes, three times a week for six weeks – Walking exercise should be performed at 60-70% of the pVO2, at a level of 13-15 on the Borg scale and 60-70% heart rate reserve.
Supervised group exercise programs have better short-term outcomes than unsupervised home exercises.The chronic nature of SpA requires ongoing, regular exercise. [1][1][3]
Special attention should be given to a good posture of the patient.[3] RAPIT (Rheumatoid Arthritis Patients In Training) is a training program for patients with rheumatoid arthritis. It is a biweekly, supervised groupsession that consists of bicycle training, an exercise circuit, and a sport or a game. The duration of each session varies from 60 to 75 minutes.
Cycle ergometer training (duration: 20 minutes)
- 1-2 minutes warm-up of at 40 watts (women) and 50 watts (men)
- 60–80 rounds per minute (rpm) and 60-80 % of maximum heart rate (MHR=220/[226-age]) to increase aerobic capacity. Ratings of perceived exertion (0=“not at all exhausting” to 10=“maximal exhaustion”) should be at values of 5 to 6.
Exercise circuit (duration: 20-30 minutes) – The circuit training is a sequential training exercise to enhance muscle strength, strength endurance, mobility and coordination. Over 20 minutes a circuit of eight to ten single exercises is completed twice, each exercise lasting 60 to 90 seconds with 30-60 seconds resting time between each one.
Sport/games (duration: 20 minutes) – This section of the program consists of impact-delivering sporting activities such as badminton, volleyball, indoor soccer, and basketball.
Clinical Bottom Line
Spondyloarthropathy is a group of multisystem inflammatory disorders affecting various joints including the spine, peripheral joints and periarticular structures. They are associated with extra-articular manifestations (for example a fever). The majority are HLA B27 positive (serological test) and Rheumatoid Factor (RF) negative.
There are 4 major seronegative spondyloarthropathies:
- Ankylosing Spondylitis (AS): is the prototype and effects more men than women
- Reiter’s Syndrome
- Psoriatic Arthritis
- Arthritis of Inflammatory Bowel Disease
Sacroiliitis is a common manifestation in all of these disorders.
Although a triggering infection and immune mechanisms are thought to underlie most of the spondyloarthopathies, their pathogenesis remains obscure.
Physical examination of the spine involves the cervical, thoracic and lumbar region. The physician may ask the patient to bend the back in different ways, check the chest circumference and also may search for pain points by pressing on different portions of the pelvis. In doubt the physician effects different diagnostic procedures such as X-ray imaging, HLA B27 presence, CRP levels in blood samples.
The treatment for AS can be divided into:
- Medication
- Non steroid anti inflammatory drugs (NSAIDs)
- Anti – TNF therapy
Physiotherapy is the best known non surgical therapeutic way of treating AS improving flexibility and physical strength. Surgery is only recommended in patients with chronic cases Most cases can be treated without surgery.
References
see adding references tutorial.
- ↑ 1.001.011.021.031.041.051.061.071.081.091.101.111.121.131.141.151.161.171.18 Braun J. et al, Spondyloarthritides, Internist., 2011 May 19: 5: 2C
- ↑ 2.002.012.022.032.042.052.062.072.082.092.102.112.122.13 Braun J., Sieper J., Spondyloarthritides., Z Rheumatol. 2010 Jul; 69(5):425-32 :4: 2C
- ↑ 3.003.013.023.033.043.053.063.073.083.093.103.113.123.133.14 Reveille J.D., Americain college of Rheumatology, 2005 Jun 5: 5
- ↑ 4.04.14.24.34.44.54.64.7 Rudwaleit M .Et al. The Assessment of SpondyloArthritis International Society classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Ann Rheum Dis. 2011;70(1):25.: 4
- ↑ 5.05.15.25.35.45.5 Burgos-Vargas R.The assessment of the spondyloarthritis international society concept and criteria for the classification of axialspondyloarthritis and peripheral spondyloarthritis: A critical appraisal for the pediatric rheumatologist. Pediatric Rheumatology 2012, 10:14 : 2C
- ↑ 6.06.16.26.36.46.56.66.7 Braun J, Sieper J. Early diagnosis of spondyloarthritis. Nature clinical practice rheumatology. october 2006 vol 2 no 10 : 2C
- ↑ 7.07.17.27.37.4 Jürgen Braun* and Joachim Sieper†, Early diagnosis of spondyloarthritis , 2006 : 2C
- ↑ 8.08.18.28.38.4 ozgur akgul, Classification criteria for spondyloarthropathies, , World J Orthop. 2011 December 18; 2(12): 107-115 : 2A
- ↑ 9.09.19.29.39.49.59.69.7 Walter P. Maksymowych, Frpc, Magnetic Resonance Imaging for Spondyloarthritis — Avoiding the Minefield (https://jrheum.com/subscribers/07/02/259.html) 4
- ↑ 10.010.110.210.310.410.510.610.710.8 Sieper J. Et al. Concepts and epidemiology of spondyloarthritis. Elsevier Ltd. 2006 : 2C
- ↑ 11.011.1 Wesseling J, Dekker J, Van den Berg WB, Bierma-Zeinstra SM, Boers M, Cats HA, Deckers P, Gorter KJ, Heuts PH, Hilberdink WK, Kloppenburg M. CHECK (Cohort Hip and Cohort Knee): similarities and differences with the Osteoarthritis Initiative. Annals of the rheumatic diseases. 2009 Sep 1;68(9):1413-9.
- ↑ 12.012.112.2 Slobodin G., Recently diagnosed axial spondyloarthritis: gender differences and factors related to delay in diagnosis., Clin Rheumatol., 2011 Mar 1
- ↑ Roussou E, Sultana S. Spondyloarthritis in women: differences in disease onset, clinical presentation, and Bath Ankylosing Spondylitis Disease Activity and Functional indices (BASDAI and BASFI) between men and women with spondyloarthritides. Clinical rheumatology. 2011 Jan 1;30(1):121-7.
- ↑ Colbert R.A., Early axial spondyloarthritis., Curr Opin Rheumatol., 2010 Sep;22(5):603-7