Subjective
Patient Intake
- History of present condition (HPC) (Was there trauma or was it insidious onset? Mechanism of Injury?)
Special Questions (Region‐specific historical examination)
- Any back or leg pain? (Is pain in a dermatomal region – pain in the knee can be referred from the back)
- Is there hip or ankle pain? (Knee pain can be referred from the hip or biomechanically affected by the ankle)
- Did the patient hear a pop/click at time of injury?
- Does the knee give way? (instability/rupture of ligaments)
- Does the knee lock? (meniscus)
- Did the knee swell? How quickly? Where is the swelling? (Intra articular/ extra articular; immediate swelling usually indicates trauma within the knee such as ligament damage)
- Was there bruising? (Immediate bruising indicates significant trauma
- Cough/sneeze cause pain?
- Does the patient experiencing locking (may indicate a bucket handle meniscal tear).
- Age – The following conditions are not exclusive to these age groups but a higher prevalence is noted in these populations (elderly – OA?, young – osgoods schlatters, middle aged- meniscal).
- Type of shoes ( wear patterns/age of shoes/proper design)
Additional Information
- Past Medical History (PMH) (Pre-existing medical conditions)
- Drug history (DH) (Any relevant medications?)
- Social History (SH) (Work/sports/hobbies affected?)
Investigations
- Radiological Considerations – any previous X-Rays or scans
- Other investigations – any recent blood tests
Red Flags
These are the special questions which may indicate that something more sinister may be going on. If you suspect that the problem is not musculoskeletal and/or something sinister may be going on patients should be referred immediately back to their doctor with your concerns noted.
- Bilateral pins and needles or numbness in the LL.
- Problems with bowel and bladder function where the patient is unable to feel themselves going to the toilet.
- Incontinence.
- Paraesthesia in the groin region.
- Loss of pulses in the LL (Vascular compromise).
- Obvious deformity.
If nothing sinister but the symptoms are more severe than you might expect ask a seniors advice on whether and A&E referral is more appropriate. Mechanism of Injury is important here, what force was exerted through the leg? Was it enough for a tibia/femur fracture? Loss of pulses in the foot may indicate vascular compromise.
Clinical Reasoning – What does the History tell you?
Knowing the history gives clues as to the structures affected. Mechanism of injury is extremely important. If you can work out the force of the injury this gives you clues on likely stretched/ damaged structures (Valgus force may indicate an MCL sprain, varus force may indicate an LCL sprain, foot planted and twisted may indicate an ACL sprain/rupture).
Make sure you rule out the back and hip unless there is a clear mechanism of injury as the knee can be a referred site of pain for both these areas. Immediate swelling and bruising usually indicates significant trauma and may require X-Ray to rule out tibial plateau fractures, bone bruises or an MRI to investigate the integrity of the ligaments.
Go into your objective examination with a working hypothesis. Use your physical examination to identify dysfunction and special tests to prove or disprove your hypothesis.
Objective
The objective examination gives you quantifiable measures to rule out what structures are involved and to reassess after treatment to determine improvement/deterioration.
General Observation
- Posture
- Movement Patterns
Functional Tests
- Small knee bend
- Sit to stand
- Squat
- Jump
- Hop
- Run
Inspection & Palpation
Inspection
- Effusion
- Poor Alignment
- Muscle Wasting
Palpation
- MCL
- LCL
- Joint Line
- Patella
- Retinaculae
- Patellar Tendon
- Hamstrings Tendons
- Popliteus.
Neurologic Assessment
If neurological deficits or referral from lumbar spine are suspected you should perform a neurological assessment:
Reflexes
- Patella Ligament (L3/L4)
- Achilles Tendon (S1/S2)
Dermatomes
Myotomes
- L2 Hip Flexion
- L3 Knee Extension
- L4 Dorsiflexion
- L5 Big Toe Extension OR 4 Lesser Toes Extension
- L5/S1 Knee Flexion
- S1 Plantarflexion OR Foot Eversion
- S2 Toe Flexion
Other neurological testing includes: Babinski and Clonus
Movement Testing
- AROM, PROM, and Overpressure
- Muscle Strength and length
- Clear hip and ankle with full AROM + overpressure
- If lumbar spine suspected add passive intevertebral mobilisations (PA spinous processes, PA transverse processes).
Special Tests
Special tests are used to prove or disprove your working hypothesis and identify the dysfunctional structures. See full list of knee special tests
ACL
PCL
MCL/LCL
LCL
Meniscus
Patellofemoral
ITB
Osteochondritis Dissecans
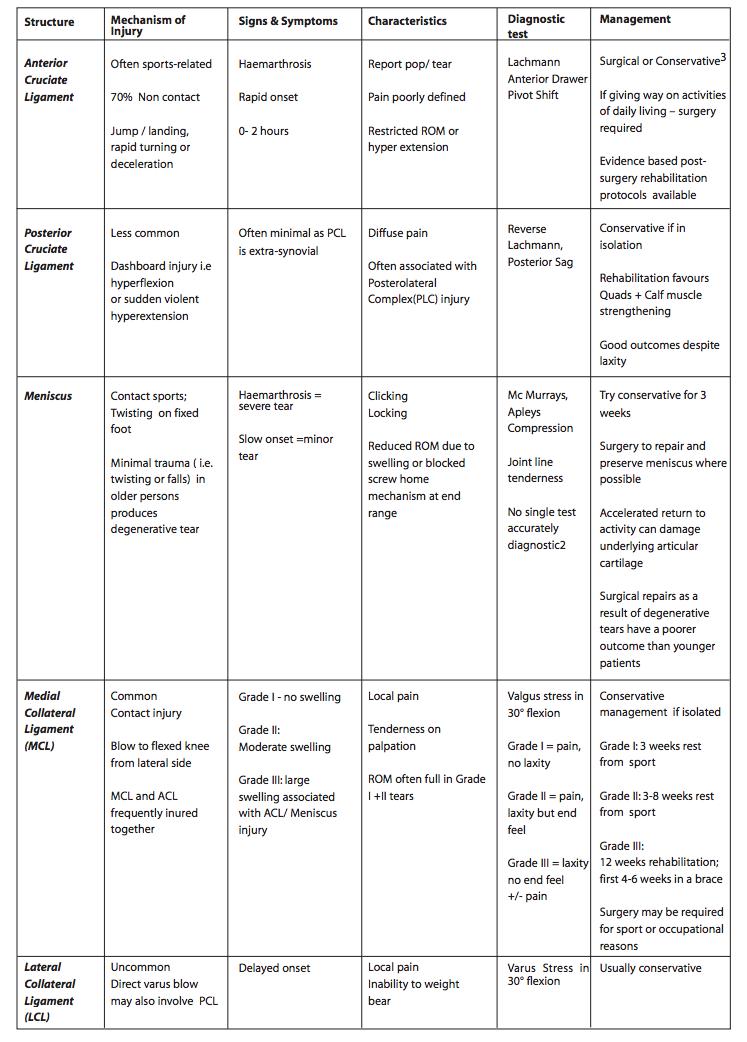
Assessment and Management of common knee injuries[28]
References
- ↑ BJSM Videos. Knee Exam (1 of 27): Introduction. Available from: ↑ BJSM Videos. Knee Exam (2 of 27): Inspection: standing. Available from: ↑ BJSM Videos. Knee Exam (3 of 27): Walking. Available from: ↑ BJSM Videos. Knee Exam (4 of 27): Balance. Available from: ↑ BJSM Videos. Knee Exam (9 of 27): Inspection & palpation: supine. Available from: ↑ BJSM Videos. Knee Exam (5 of 27): Neurovascular evaluation: supine. Available from: ↑ BJSM Videos. Knee Exam (6 of 27): Hip examination: supine. Available from: ↑ BJSM Videos. Knee Exam (7 of 27): Range of Motion Part 1. Available from: ↑ BJSM Videos. Knee Exam (8 of 27): Range of Motion Part 2. Available from: ↑ BJSM Videos. Knee Exam (10 of 27): Effusion. Available from: ↑ BJSM Videos. Knee Exam (11 of 27): Effusion (subtle). Available from: ↑ BJSM Videos. Knee Exam (12 of 27): Lachman test. Available from: ↑ BJSM Videos. Knee Exam (13 of 27): Posterior drawer. Available from: ↑ BJSM Videos. Knee Exam (14 of 27): MCL. Available from: ↑ BJSM Videos. Knee Exam (15 of 27): LCL. Available from: ↑ BJSM Videos. Knee Exam (16 of 27): Posterolateral corner. Available from: ↑ BJSM Videos. Knee Exam (17 of 27): Meniscal assessment: palpation & bounce home test. Available from: ↑ BJSM Videos. Knee Exam (18 of 27): McMurray’s test. Available from: ↑ BJSM Videos. Knee Exam (19 of 27): Apley’s test. Available from: ↑ BJSM Videos. Knee Exam (20 of 27): Acute patellofemoral joint injuries. Available from: ↑ BJSM Videos. Knee Exam (21 of 27): Standing McMurray’s test. Available from: ↑ BJSM Videos. Knee Exam (22 of 27): Pivot shift. Available from: ↑ BJSM Videos. Knee Exam (23 of 27): ACL assessment Part 1. Available from: ↑ BJSM Videos. Knee Exam (24 of 27): ACL assessment Part 2. Available from: ↑ BJSM Videos. Knee Exam (25 of 27): ACL assessment Part 3 (“Ladies’ Lachman”). Available from: ↑ BJSM Videos. Knee Exam (26 of 27): ACL case examination. Available from: ↑ BJSM Videos. Knee Exam (27 of 27): Pearls & Pitfalls. Available from: ↑ Wilson, L and Blaney, A. Physiotherapy management of common knee conditions in the primary care setting. Irish Society of Chartered Physiotherapists. [Accessed 26 jan 2015]