Definition
The term ‘shoulder instability’ is used to refer to the inability to maintain the humeral head in the glenoid fossa.[1] The ligamentous and muscle structures around the glenohumeral joint, under non-pathological conditions, create a balanced net joint reaction force. The relevant structures are listed below. If the integrity of any of these structures is disrupted it can lead to atraumatic or traumatic instability. Atraumatic instability commonly results from repetitive overhead movements or congenital joint features. Traumatic mechanisms of injury may result in frank dislocations where there is a loss of joint integrity. Instability can occur anteriorly, posteriorly, or in multiple directions regardless of mechanism of injury.
Common Categorisations of Shoulder Instability
Traumatic
Traumatic instability of the shoulder is a common condition, which, especially in young patients, is associated with high recurrence rates. Among the different types of this joint instability, the anterior dislocation due to trauma is the most common type, corresponding to more than 90% of the cases.[2]
Atraumatic
Atraumatic (non-traumatic) shoulder instability is a subclassification of glenohumeral joint instability, encompassing those for whom trauma is not considered the primary aetiology. [3]
Two main types of atraumatic instabilities:
- Congenital instabilities;
- Laxity of structures in the shoulder which may be present since birth.[4]
- Chronic recurrent instabilities
- May be seen after surgery for shoulder dislocation, due to glenoid rim lesions.[5]
- Over time, microtrauma can lead to instability of the glenohumeral joint.
Clinically Relevant Anatomy
Glenohumeral stability depends on the combination of various factors that can be grouped in capsuloligamentary or static stabilizers and musculotendinous or dynamic stabilizers:
Video
Static Stabilisers
The static capsuloligamentary elements, as these are considered to be the main stabilizers of the glenohumeral joint[6]
- Superior glenohumeral ligament (SGHL) [7] – limits anterior and inferior translation of adducted humerus
- Medial glenohumeral ligament (MGHL) – limits anterior translation in lower and middle range of abduction
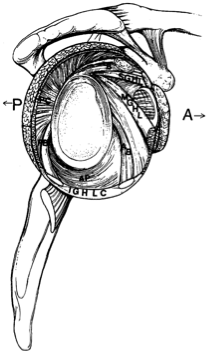
- Inferior glenohumeral ligament (IGHL) – longest glenohumeral ligament and primary static restraint against anterior, posterior and inferior translation when humerus is abducted beyond 45 degrees
- Glenoid labrum – increases depth of glenoid cavity and increases stability up to 50% [4]
- Negative intra-articular pressure [7] – assists in maximizing joint congruency
The proprioception mechanisms of the shoulder joint have been investigated and found to be closely related to the response of the dynamic muscle stabilisers. Various histological studies in anatomical specimens have confirmed the presence of afferent nerve endings (Ruffini corpuscles and Pacini) and their distribution in the shoulder capsuloligamentary complex.[6] Cuellar[6][6]suggests that shoulder instability can be due to injury and/or failure of the static capsulo-ligamentary stabilizing elements, which are supporting the sensitive afferent ending, this alteration of the passive stabilizing elements causes a disturbance or delay in the delivery of the proprioceptive signal causing a delay and/or error of coordination of the corresponding muscle response. The dynamic stabilizing mechanism is thus altered and the loss of joint congruity is facilitated.
Dynamic Stabilisers
Assist with holding the humeral head in the glenoid fossa during movement [4]
1. Primary
- Rotator cuff muscles (supraspinatus,infraspinatus, teres minor, subscapularis)
- Long head of biceps
- Deltoid
2. Secondary
- Teres major
- Latissimus dorsi
- Pectoralis major
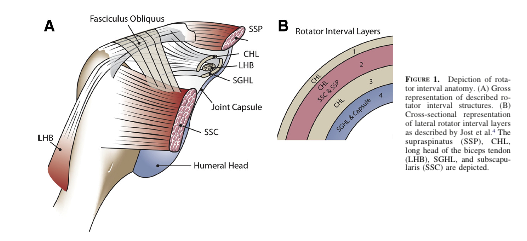
3. Rotator Cuff Interval
This interval is a triangular-shaped area found in the shoulder, with borders noted below. A large rotator interval allows for increased anterior humeral head translation due to the lack of structures supporting the joint capsule anteriorly.[4]
- Superior border: anterior margin of supraspinatus
- Inferior border: subscapularis
- Apex: transverse humeral ligament
- Base: coracoid process
| Anterior | Posterior | Multidirectional |
| SGHL,MGHL, Anterior IGHL | SGHL, Posterior IGHL | Dysfunction of dynamic stabilisers |
| Anterior capsule | Posterior capsule | Joint capsule in 2 or more directions. Inferior capsule is primarily affected. |
| Coracohumeral ligament | Coracohumeral ligament | All structures involved in anterior or posterior instability can be affected |
| Superior anterior labrum | ||
| Long head of biceps | ||
| Subscapularis |
Epidemiology
98% of primary dislocations occur anteriorly.[7] The rate of recurrence is most common in younger populations (see figure 1B3). The incidence of congenital instability is unknown.[4]
Mechanism of Injury
Traumatic
The most common glenohumeral dislocation occurs anteriorly, usually as a result of sporting accidents or falls, particularly when the upper extremity is in 90° abduction and external rotation.
Posterior dislocations most commonly result from seizures, shock and falls.
Atraumatic
Chronic Recurrent
Caused by repetitive extreme external rotation with the humerus abducted and extended (i.e.pitching motion).[4] Instability may be caused by gradual weakening of the anterior and inferior static restraints. The humeral head will tend to move away from shortened structures. For example: posterior shoulder capsular tightness will cause the humeral head to shift anteriorly, resulting in a loss of integrity of all anterior structures. Commonly associated with participation in sports such as gymnastics, baseball, softball, tennis, swimming, and weight training.[4]
Common concomitant features or causes:
- Bankart lesion
- HillSachs lesion
- SLAP lesion (Superior Labrum Anterior Posterior)
- HAGL lesion (Humeral Avulsion of Glenohumeral Ligaments)
- ALPSA lesion (Anterior Labroligamentous Periosteal Sleeve Avulsion)
- Laxity of the joint capsule
Congenital Instability [4]
Congenital instability may be the result of:
- Hypoplastic glenoid
- Decrease anterior-posterior diameter of glenoid
- Increased retroversion of glenoid
- Increased amount and composition of collagen and elastin
- Bony anomalies
Clinical Presentation
Possible signs and symptoms of chronic/recurrent instability
Anterior Instability
- Clicking
- Pain
- Complain of dead arm with throwing
- Pain posteriorly
- Possible subacromial or internal impingement signs
- The patient may have a positive apprehension test, relocation test, and/or anterior release test
- Increased joint accessory motion particularly in the anterior direction
internal impingement
Glenohumeral internal rotation deficit (GIRD) may be present
Pain
Clicking
Increased joint accessory motion particularly in the posterior direction
Multidirectional Instability
- Antero-inferior laxity most commonly presents with global shoulder pain, cannot pinpoint to a specific location
- May have a positive sulcus sign, apprehension/relocation test, anterior release tests
- Secondary rotator cuff impingement can be seen with microtraumatic events caused during participation in sports such as gymnastics, swimming and weight training[4]
- Increased joint accessory motion in multiple planes
Differential Diagnosis
Subjective History
May have history of trauma with or without a previous dislocation
May have history of lax joints (consider elbow, knee, thumb hyperextension[4]; use [4]
Physical Examination
Screen cervical spine and thoracic spine
Observation/Palpation
- Long head of biceps, supraspinatus tendon, AC joint, SC joint, spine, 1st rib, other regional muscles
Posture[8]
- Asymmetry
- Scapular winging
- Atrophy
Active ROM
- Glenohumeral flexion, extension, abduction, adduction, rotation – internal & external, scaption
- Look for apprehensive behavior
Passive ROM
- May have pain,
- May have stiffness
- Again, apprehension will be present
Muscle Length Testing
- Upper trapezius, levator scapulae, scalenes, latissimus dorsi, lower trapezius, pectoralis minor, pectoralis major
Resistive Testing
Functional Testing[9]
- Hand to posterior neck
- Hand to scapula
- Hand to opposite scapula
Joint Accessory Motion Testing
- Increased mobility in the direction of the instability (anterior, posterior, multidirectional)
Scapular/Thoracic Motion[4]
Proprioception
Special Tests
- Possibly sulcus sign, apprehension/relocation and/or anterior release tests depending on suspected form of instability
Special Tests
Provocative tests and laxity examinations may be used to confirm a hypothesis of shoulder instability:
Psychometric Properties of Special Tests
Test
Sensitivity
Specificity
+ LR
-LR
Sulcus
0.17
0.93
2.43
0.89
Anterior
Release Test[10]
0.92
0.89
8.36
0.09
Apprehension[11]
0.53
0.99
53
0.47
Relocation[11]
0.46
0.54
1
1
Laxity Tests
[12] have concluded that this test is entirely reliable (p 80 for instability.
Drawer Test
Application:
The patient is positioned supine. The examiner holds the patients scapula with his left hand while grasping the patient’s upper arm and drawing the humeral anterior head with his right hand. You can hold the shoulder in a different position.
Conclusion:
The test tells you more about the laxity. The test is positive when the thumb was felt to slide past the coracoid.
Clinical Bottom Line:
Tzannes and Murell [13] have concluded that this test is still to be assessed as to its validity and reliability.
Sulcus Sign
Application:
The patient’s elbow is pulled inferiorly while the patient is relaxed
Conclusion:
This manoeuvre tests the superior glenohumeral ligament. The test is positive when there is a sulcus of more than 2 cm between the acromion and caput humerus.
Clinical Bottom Line:
Tzannes and Murell[14] also evaluate this test as being completely reliable (p
Provocative Tests
Anterior Release Test
Application:
In this test, the examiner applies posteriorly directed force to the humeral head, with the patient being in abduction and external rotation.
Conclusion:
The test is positive in case of pain or apprehension when easing the pressure.
Clinical Bottom Line:
In the light of the results of Tzannes and Murell [15](p[16] we can conclude that it is a reliable test for the detection of the unstable shoulder. Gross et al report a sensitivity of 0.92 and a specificity of 0.89, making this test useful to rule out shoulder instability with a negative result.
Apprehension/Augmentation Test
Application:
The apprehension test is being applied when the patient is lying or sitting with the shoulder in a neutral position (90° abduction). The examiner holds the patient’s wrist with one hand and with the other hand he applies anteriorly directed force to the humeral head.
Conclusion:
Signs of glenohumeral anterior instability are: pain, a feeling of subluxation or clear defence. If a relocation test is being applied almost immediately after the apprehension test and if this relocation test results to be negative, than we can decide that there is anterior instability.
Clinical Bottom Line:
Based on the results of Levy et al. [17]; Ian et al. [18] (sensitivity = 53 & specificity = 99), Tzannes and Murell [19] (p= 0,0004 pain and/or apprehension and a LR 8-100 for anterior instability) and Marx et al.[20], we are able to conclude that there is not sufficient clinical proof to detect or exclude instability. Lo et al report a specificity of 0.99.
Relocation Test
Application:
The patient is in the starting position of the apprehension test and the examiner now applies posteriorly directed force to the humeral head.
Conclusion:
When this test results to be negative, there is glenohumeral anterior instability.
Clinical Bottom Line:
The article by Ian et al. [21] (sensitivity = 45 & specificity = 54) states that the relocation test is not clinically evident. However, other articles by Tzannes and Murell[22] (p= 0,0003 pain and/or apprehension) and Liu et al.[23] provide evidence to the contrary. Lo et al report poor psychometric properties on this test.
Outcome Measures
Disabilities of Shoulder, Arm, and Hand (DASH)
Quick DASH
Diagnosis specific questionnaires[24]
- Western Ontario Shoulder Instability Index
- Oxford Shoulder Instability Questionnaire
- Melbourne Instability Shoulder Scale
Medical Management
Medical management will hinge on the specifics of the patient presentation including the mechanism of injury, severity, patient goals, etc. In some cases, particularly those with a traumatic mechanism, surgical intervention may be warranted to restore joint stability.
Types of surgical procedures for traumatic glenohumeral dislocations[4]
- Open capsular shift
- Arthroscopic thermal capsulorraphy
Physical Therapy Management
Non-operative physical therapy management will vary in a case-by-case situation and each patient’s care should be individualised to target their specific goals. Physical therapy management is largely impairment-based and response-driven as there is little high-level evidence to assist decision making but commonly includes:
- Education to prevent recurrence
- Postural re-education
- Motor control training of specific muscles during functional activities (rotator cuff muscles, scapular stabilisers)
- Strengthening in particular the deltoid, rotator cuff muscles and scapular stabilisers
- Stretching in particular posterior shoulder structures, pectoralis major and minor and any other muscles with flexibility impairments
Manual therapy targeting impairments of mobility in the glenohumeral, acromioclavicular, sternoclavicular joints and cervico-thoracic spine [25](LoE4)
Exercise therapy
In one studie participants undertook the Watson multi directional instability rehabilitation program that focused on regaining stability and control of muscles acting on the glenohumeral joint and scapulothoracic joints and gradually progressing the shoulder into functional positions and activities.The program, which has been published in detail was advised and monitored by the author (L.W.) and required participants to attend rehabilitation once weekly for 12 weeks.
Results of all of the muscle strength tests evaluated in the current study demonstrated significant improvements at follow up, with the standard mean differencecs demonstrating moderate to large effects. [26] (LOE: 4).
Two studies described excercise therapy after Bankart and reverse Bankart.
In one studie patients were operated with two biodegradable anchor sutures (artroscopic Bankart). after surgery, the patients wore a shoulder immobilizer for 3 weeks. Isometric exercise in the sling was started at 1 day postoperatively. Increasing range of motion exercises were prescribed for 2 weeks after surgery. The shoulder immobilizer was removed, and active flexion exercise in the supine position and passive external rotation exercise were started at 3 weeks postoperatively. Rotator cuff exercise was started using a rubber band at 4 weeks postoperatively, and unlimited activities of daily living were allowed at 6 weeks postoperatively. Upper limb muscle training was permitted using a
Arthroscopic Bankart repair is less invasive to the muscles around the shoulder joint, and sufficient stability can be obtained using the suture anchor technique. In the current study, favorable progress was obtained during the postoperative rehabilitation program after arthroscopic Bankart repair. Shoulder rotational muscle strength after arthroscopic Bankart repair recovered to preoperative levels by 6 months for external rotation and 4.5 months for internal rotation. Because dislocations of the glenohumeral joint occurred during external rotation, the apprehensive feeling would create external muscle strength loss. Moreover, the infraspinatus muscle was passed through by an arthroscope during surgery; on the other hand, the subscapularis muscle was not damaged. These would explain why muscle strength for external rotation recovered later than that for internal rotation.[27] (LOE 4)
Posterior shoulder instability can be further divided dimensionally: unidirectionally (posterior), bidirectionally (posteroinferior), and multidirectionally (posterior, inferior, and anterior). Bidirectional and multidirectional instability are much more common than unidirectional instability. Specific pathoanatomic lesions, such as a reverse Bankart lesion, are often observed in patients with posterior instability caused by trauma. Multidirectional instability may have an inciting traumatic event, but it is due to preexisting global capsular laxity. Glenohumeral instability is a multifaceted disorder with varying causes, degrees, and directions of instability. Conservative physiotherapy management is recommended as the primary option for treatment. If conservative treatment is unsuccessful after a 6-month course, surgery may be considered. For the first month, the shoulder should be kept in relative external or neutral rotation to relax the posterior capsule and antevert itself. Between the first and second months’ postsurgery, passive and active assisted range of motion can begin in a protected fashion while still limiting end ranges of motion in positions that maximally stress the posterior capsule. The sling use may be discontinued around 6 weeks.
Between 2 and 5 months, strengthening can begin with isometrics for the rotator cuff and periscapular muscles. Full motion should be achieved between 2 and 3 months. Between months 5 and 8, patients may begin gradual return to previous sports, activities, and work duties but under controlled conditions. Full return depends on full functional range of motion, no pain or tenderness, good strength, and satisfactory clinical examination..[28] (LOE 1A)
Post-Op Physical Therapy Management
Depends on:
- Surgical procedure
- Surgeon’s protocol
- Mechanism of injury
- Concomitant injuries
- Tissue quality
- Impairments noted at evaluation
Clinical Bottom Line
Shoulder instability may have a traumatic or atraumatic cause. There is a high recurrence rate after a primary shoulder dislocation, which is greatest in individuals
References
- ↑ Tzannes A, Murrel, GAC. An assessment of the interexaminar reliability of tests for shoulder instability. The journal of Shoulder and Elbow Surgery 2004; 13:18-23.
- ↑ Rosa JR, Checchia CS, Miyazaki AN. Traumatic Anterior Instability of the Shoulder. Revista Brasileira de Ortopedia. 2017;52(5):513-20.
- ↑ Barrett C. The Clinical Physiotherapy Assessment of Non-Traumatic Shoulder Instability. Shoulder & Elbow. 2015 Jan;7(1):60-71.
- ↑ 4.004.014.024.034.044.054.064.074.084.094.104.114.12 Guerrero P, Busconi B, Deangelis N, Powers G. Congenital instability of the shoulder joint: assessment and treatment options. JOSPT. 2009;39(2):124-134.
- ↑ Charousset C, Beauthler V, Bellaïche, Guillin R, Brassart N, Thomazeau H. Can we improve radiological analysis of osseous lesions in chronic anterior shoulder instability? Orthop. Traumatol. Surg. Res. 2010;96:88-93.
- ↑ 6.06.16.26.3 Cuéllar R, Ruiz-Ibán MA, Cuéllar A. Suppl-6, M10: Anatomy and Biomechanics of the Unstable Shoulder. The open orthopaedics journal. 2017;11:919.
- ↑ 7.07.17.2 Hayes K, Callanan M, Walton J. Shoulder instability: Management and rehabilitation. JOSPT 2002;23(10):497-509.
- ↑ Jaggi A. Rehabilitation for shoulder instability. Br J Sports Med 2010;44(5):333.
- ↑ Yang J, Lin J. Reliability of function-related tests in patients with shoulder pathologies. JOSPT. 2006;36: 572-576.
- ↑ Gross M, Disefano M. Anterior release test: A new test for occult shoulder instability. Clinical Orthopaedics and Related Research. 1997;339:105-108.
- ↑ 11.011.1 Lo IK, Nonweiler B, Woolfrey M, Litchfield R, Kirkley A. An evaluation of the apprehension, relocation, and surprise tests for anterior shoulder instability. Am J Sports Med.2004;32:301-7
- ↑ Tzannes A, Murrel, GAC. An assessment of the interexaminar reliability of tests for shoulder instability. The journal of Shoulder and Elbow Surgery 2004; 13:18-23.
- ↑ Tzannes A, Murell GAC. Clinical examination of the unstable shoulder. Sports Medicine 2002; 32: 447-457.
- ↑ Tzannes et al. 2004
- ↑ Tzannes et al. 2002
- ↑ Ian KY, Lo IKY, Nonweiler B, et al. An evaluation of the apprehension, relocation, and surprise test for anterior shoulder instability. American Journal of Sports Medicine 2004; 32:301-307.
- ↑ Levy AS, Lintner S, Kenter K, et al: intra- and interobserver reproducibility of the shoulder laxity examination. The American Journal of Sports medicine 1999; 4: 460-463.
- ↑ Ian et al.
- ↑ Tzannes A, Murrel, GAC. An assessment of the interexaminar reliability of tests for shoulder instability. The journal of Shoulder and Elbow Surgery 2004; 13:18-23.
- ↑ Marx RG, Bombardier C, Wright JG. What do we know about the reliability and validity of physical examination tests used to examine the upper extremity? Journal of Hand Surgery 1999; 24A:185-193.
- ↑ Ian et al.
- ↑ Tzannes et al. 2004
- ↑ Liu SH, Henry MH, Nuccion S, et al. Diagnosis of glenoid labral tears. A comparison between magnetic resonance imaging and clinical examinations. The American Journal of Sports Medicine 1996; 2:149-154.
- ↑ Rouleau D, Faber K, MacDermin J. Systematic review of patient-administered shoulder functional scores on instability. J Shoulder Elbow Surg. 2010;19:1121-1128.
- ↑ Mintken. Some Factors Predict Successful Short-Term Outcomes in IndividualsWith Shoulder Pain Receiving Cervicothoracic Manipulation: A Single-Arm Trial. PTJ 2010;26-42.
- ↑ WATSON, Lyn, et al. The effects of a conservative rehabilitation program for multidirectional instability of the shoulder. Journal of shoulder and elbow surgery, 2018, 27.1: 104-111.
- ↑ AMAKO, Masatoshi, et al. Recovery of Shoulder Rotational Muscle Strength After Arthroscopic Bankart Repair. Orthopaedic journal of sports medicine, 2017, 5.9: 2325967117728684.
- ↑ TANNENBAUM, Eric; SEKIYA, Jon K. Evaluation and management of posterior shoulder instability. Sports Health, 2011, 3.3: 253-263.
0.17
Anterior
Release Test[10]
Drawer Test
Application:
The patient is positioned supine. The examiner holds the patients scapula with his left hand while grasping the patient’s upper arm and drawing the humeral anterior head with his right hand. You can hold the shoulder in a different position.
Conclusion:
The test tells you more about the laxity. The test is positive when the thumb was felt to slide past the coracoid.
Clinical Bottom Line:
Tzannes and Murell [13] have concluded that this test is still to be assessed as to its validity and reliability.
Sulcus Sign
Application:
The patient’s elbow is pulled inferiorly while the patient is relaxed
Conclusion:
This manoeuvre tests the superior glenohumeral ligament. The test is positive when there is a sulcus of more than 2 cm between the acromion and caput humerus.
Clinical Bottom Line:
Tzannes and Murell[14] also evaluate this test as being completely reliable (p
Provocative Tests
Anterior Release Test
Application:
In this test, the examiner applies posteriorly directed force to the humeral head, with the patient being in abduction and external rotation.
Conclusion:
The test is positive in case of pain or apprehension when easing the pressure.
Clinical Bottom Line:
In the light of the results of Tzannes and Murell [15](p[16] we can conclude that it is a reliable test for the detection of the unstable shoulder. Gross et al report a sensitivity of 0.92 and a specificity of 0.89, making this test useful to rule out shoulder instability with a negative result.
Apprehension/Augmentation Test
Application:
The apprehension test is being applied when the patient is lying or sitting with the shoulder in a neutral position (90° abduction). The examiner holds the patient’s wrist with one hand and with the other hand he applies anteriorly directed force to the humeral head.
Conclusion:
Signs of glenohumeral anterior instability are: pain, a feeling of subluxation or clear defence. If a relocation test is being applied almost immediately after the apprehension test and if this relocation test results to be negative, than we can decide that there is anterior instability.
Clinical Bottom Line:
Based on the results of Levy et al. [17]; Ian et al. [18] (sensitivity = 53 & specificity = 99), Tzannes and Murell [19] (p= 0,0004 pain and/or apprehension and a LR 8-100 for anterior instability) and Marx et al.[20], we are able to conclude that there is not sufficient clinical proof to detect or exclude instability. Lo et al report a specificity of 0.99.
Relocation Test
Application:
The patient is in the starting position of the apprehension test and the examiner now applies posteriorly directed force to the humeral head.
Conclusion:
When this test results to be negative, there is glenohumeral anterior instability.
Clinical Bottom Line:
The article by Ian et al. [21] (sensitivity = 45 & specificity = 54) states that the relocation test is not clinically evident. However, other articles by Tzannes and Murell[22] (p= 0,0003 pain and/or apprehension) and Liu et al.[23] provide evidence to the contrary. Lo et al report poor psychometric properties on this test.
Outcome Measures
Disabilities of Shoulder, Arm, and Hand (DASH)
Quick DASH
Diagnosis specific questionnaires[24]
- Western Ontario Shoulder Instability Index
- Oxford Shoulder Instability Questionnaire
- Melbourne Instability Shoulder Scale
Medical Management
Medical management will hinge on the specifics of the patient presentation including the mechanism of injury, severity, patient goals, etc. In some cases, particularly those with a traumatic mechanism, surgical intervention may be warranted to restore joint stability.
Types of surgical procedures for traumatic glenohumeral dislocations[4]
- Open capsular shift
- Arthroscopic thermal capsulorraphy
Physical Therapy Management
Non-operative physical therapy management will vary in a case-by-case situation and each patient’s care should be individualised to target their specific goals. Physical therapy management is largely impairment-based and response-driven as there is little high-level evidence to assist decision making but commonly includes:
- Education to prevent recurrence
- Postural re-education
- Motor control training of specific muscles during functional activities (rotator cuff muscles, scapular stabilisers)
- Strengthening in particular the deltoid, rotator cuff muscles and scapular stabilisers
- Stretching in particular posterior shoulder structures, pectoralis major and minor and any other muscles with flexibility impairments
Manual therapy targeting impairments of mobility in the glenohumeral, acromioclavicular, sternoclavicular joints and cervico-thoracic spine [25](LoE4)
Exercise therapy
In one studie participants undertook the Watson multi directional instability rehabilitation program that focused on regaining stability and control of muscles acting on the glenohumeral joint and scapulothoracic joints and gradually progressing the shoulder into functional positions and activities.The program, which has been published in detail was advised and monitored by the author (L.W.) and required participants to attend rehabilitation once weekly for 12 weeks.
Results of all of the muscle strength tests evaluated in the current study demonstrated significant improvements at follow up, with the standard mean differencecs demonstrating moderate to large effects. [26] (LOE: 4).
Two studies described excercise therapy after Bankart and reverse Bankart.
In one studie patients were operated with two biodegradable anchor sutures (artroscopic Bankart). after surgery, the patients wore a shoulder immobilizer for 3 weeks. Isometric exercise in the sling was started at 1 day postoperatively. Increasing range of motion exercises were prescribed for 2 weeks after surgery. The shoulder immobilizer was removed, and active flexion exercise in the supine position and passive external rotation exercise were started at 3 weeks postoperatively. Rotator cuff exercise was started using a rubber band at 4 weeks postoperatively, and unlimited activities of daily living were allowed at 6 weeks postoperatively. Upper limb muscle training was permitted using a
Arthroscopic Bankart repair is less invasive to the muscles around the shoulder joint, and sufficient stability can be obtained using the suture anchor technique. In the current study, favorable progress was obtained during the postoperative rehabilitation program after arthroscopic Bankart repair. Shoulder rotational muscle strength after arthroscopic Bankart repair recovered to preoperative levels by 6 months for external rotation and 4.5 months for internal rotation. Because dislocations of the glenohumeral joint occurred during external rotation, the apprehensive feeling would create external muscle strength loss. Moreover, the infraspinatus muscle was passed through by an arthroscope during surgery; on the other hand, the subscapularis muscle was not damaged. These would explain why muscle strength for external rotation recovered later than that for internal rotation.[27] (LOE 4)
Posterior shoulder instability can be further divided dimensionally: unidirectionally (posterior), bidirectionally (posteroinferior), and multidirectionally (posterior, inferior, and anterior). Bidirectional and multidirectional instability are much more common than unidirectional instability. Specific pathoanatomic lesions, such as a reverse Bankart lesion, are often observed in patients with posterior instability caused by trauma. Multidirectional instability may have an inciting traumatic event, but it is due to preexisting global capsular laxity. Glenohumeral instability is a multifaceted disorder with varying causes, degrees, and directions of instability. Conservative physiotherapy management is recommended as the primary option for treatment. If conservative treatment is unsuccessful after a 6-month course, surgery may be considered. For the first month, the shoulder should be kept in relative external or neutral rotation to relax the posterior capsule and antevert itself. Between the first and second months’ postsurgery, passive and active assisted range of motion can begin in a protected fashion while still limiting end ranges of motion in positions that maximally stress the posterior capsule. The sling use may be discontinued around 6 weeks.
Between 2 and 5 months, strengthening can begin with isometrics for the rotator cuff and periscapular muscles. Full motion should be achieved between 2 and 3 months. Between months 5 and 8, patients may begin gradual return to previous sports, activities, and work duties but under controlled conditions. Full return depends on full functional range of motion, no pain or tenderness, good strength, and satisfactory clinical examination..[28] (LOE 1A)
Post-Op Physical Therapy Management
Depends on:
- Surgical procedure
- Surgeon’s protocol
- Mechanism of injury
- Concomitant injuries
- Tissue quality
- Impairments noted at evaluation
Clinical Bottom Line
Shoulder instability may have a traumatic or atraumatic cause. There is a high recurrence rate after a primary shoulder dislocation, which is greatest in individuals
References
- ↑ Tzannes A, Murrel, GAC. An assessment of the interexaminar reliability of tests for shoulder instability. The journal of Shoulder and Elbow Surgery 2004; 13:18-23.
- ↑ Rosa JR, Checchia CS, Miyazaki AN. Traumatic Anterior Instability of the Shoulder. Revista Brasileira de Ortopedia. 2017;52(5):513-20.
- ↑ Barrett C. The Clinical Physiotherapy Assessment of Non-Traumatic Shoulder Instability. Shoulder & Elbow. 2015 Jan;7(1):60-71.
- ↑ 4.004.014.024.034.044.054.064.074.084.094.104.114.12 Guerrero P, Busconi B, Deangelis N, Powers G. Congenital instability of the shoulder joint: assessment and treatment options. JOSPT. 2009;39(2):124-134.
- ↑ Charousset C, Beauthler V, Bellaïche, Guillin R, Brassart N, Thomazeau H. Can we improve radiological analysis of osseous lesions in chronic anterior shoulder instability? Orthop. Traumatol. Surg. Res. 2010;96:88-93.
- ↑ 6.06.16.26.3 Cuéllar R, Ruiz-Ibán MA, Cuéllar A. Suppl-6, M10: Anatomy and Biomechanics of the Unstable Shoulder. The open orthopaedics journal. 2017;11:919.
- ↑ 7.07.17.2 Hayes K, Callanan M, Walton J. Shoulder instability: Management and rehabilitation. JOSPT 2002;23(10):497-509.
- ↑ Jaggi A. Rehabilitation for shoulder instability. Br J Sports Med 2010;44(5):333.
- ↑ Yang J, Lin J. Reliability of function-related tests in patients with shoulder pathologies. JOSPT. 2006;36: 572-576.
- ↑ Gross M, Disefano M. Anterior release test: A new test for occult shoulder instability. Clinical Orthopaedics and Related Research. 1997;339:105-108.
- ↑ 11.011.1 Lo IK, Nonweiler B, Woolfrey M, Litchfield R, Kirkley A. An evaluation of the apprehension, relocation, and surprise tests for anterior shoulder instability. Am J Sports Med.2004;32:301-7
- ↑ Tzannes A, Murrel, GAC. An assessment of the interexaminar reliability of tests for shoulder instability. The journal of Shoulder and Elbow Surgery 2004; 13:18-23.
- ↑ Tzannes A, Murell GAC. Clinical examination of the unstable shoulder. Sports Medicine 2002; 32: 447-457.
- ↑ Tzannes et al. 2004
- ↑ Tzannes et al. 2002
- ↑ Ian KY, Lo IKY, Nonweiler B, et al. An evaluation of the apprehension, relocation, and surprise test for anterior shoulder instability. American Journal of Sports Medicine 2004; 32:301-307.
- ↑ Levy AS, Lintner S, Kenter K, et al: intra- and interobserver reproducibility of the shoulder laxity examination. The American Journal of Sports medicine 1999; 4: 460-463.
- ↑ Ian et al.
- ↑ Tzannes A, Murrel, GAC. An assessment of the interexaminar reliability of tests for shoulder instability. The journal of Shoulder and Elbow Surgery 2004; 13:18-23.
- ↑ Marx RG, Bombardier C, Wright JG. What do we know about the reliability and validity of physical examination tests used to examine the upper extremity? Journal of Hand Surgery 1999; 24A:185-193.
- ↑ Ian et al.
- ↑ Tzannes et al. 2004
- ↑ Liu SH, Henry MH, Nuccion S, et al. Diagnosis of glenoid labral tears. A comparison between magnetic resonance imaging and clinical examinations. The American Journal of Sports Medicine 1996; 2:149-154.
- ↑ Rouleau D, Faber K, MacDermin J. Systematic review of patient-administered shoulder functional scores on instability. J Shoulder Elbow Surg. 2010;19:1121-1128.
- ↑ Mintken. Some Factors Predict Successful Short-Term Outcomes in IndividualsWith Shoulder Pain Receiving Cervicothoracic Manipulation: A Single-Arm Trial. PTJ 2010;26-42.
- ↑ WATSON, Lyn, et al. The effects of a conservative rehabilitation program for multidirectional instability of the shoulder. Journal of shoulder and elbow surgery, 2018, 27.1: 104-111.
- ↑ AMAKO, Masatoshi, et al. Recovery of Shoulder Rotational Muscle Strength After Arthroscopic Bankart Repair. Orthopaedic journal of sports medicine, 2017, 5.9: 2325967117728684.
- ↑ TANNENBAUM, Eric; SEKIYA, Jon K. Evaluation and management of posterior shoulder instability. Sports Health, 2011, 3.3: 253-263.