Introduction
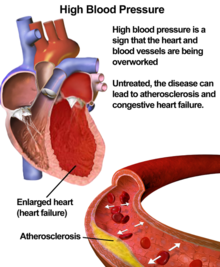
According to the American Heart Association, hypertension or high blood pressure, is when the force of blood flowing through your blood vessels is consistently too high. For standardized blood pressure ranges see the [1]
Hypertension can be classified as either essential hypertension or secondary hypertension. Essential hypertension does not have a known cause and can be linked to a plethora of pathophysiologic factors. Factors associated with essential hypertension include: increased SNS activity, long term high sodium intake, diabetes mellitus, and obesity.[2] Secondary hypertension is often the result of a separate pathophysiological condition such as: renal disease, primary aldosteronism, and obstructive sleep apnea.[3]
Hypertension is one of the most prevalent diseases in the United States, according to the [4] Due to the high prevalence of hypertension, a physical therapist will routinely encounter patients with the disease. It is vital that a clinician understands the general mechanism of action and adverse effects surrounding hypertension medications. This article serves to outline the major medications used in the treatment of hypertension as well as the implications they may have for physical therapy practice.
Drug Classes in the Treatment of Hypertension
Beta-blockers in the Treatment of Hypertension
Diuretics in the Treatment of Hypertension
Renin-Angiotensin Drugs in the Treatment of Hypertension
Vasodilators in the Treatment of Hypertension
Implications for Physical Therapy
According to the American Physical Therapy Association, “Physical therapist patient/client management integrates an understanding of a patient’s/client’s prescription and nonprescription medication regimen with consideration of its impact upon health, impairments, functional limitations, and disabilities. The administration and storage of medications used for PT interventions is also a component of patient/client management and thus within the scope of PT practice”.[5] Considering the prevalence of hypertension, therapists will undoubtedly work with many patients taking antihypertensive medications and should factor the effects of antihypertensives in their plan of care. A few important considerations for the physical therapist when treating hypertensive patients include: ensuring efficient scheduling in correspondence with therapy schedule, monitoring side effects, ensuring patient adherence to medications, and also selecting appropriate therapeutic exercises for each individual patient.
In regards to monitoring side effects, orthostatic hypotension is of the utmost concern for patients currently taking antihypertensives. Clinicians should be cautious when their patient changes posture suddenly or engages in activities that may lower blood pressure. In addition, patients need to educated on the significant impact that uncontrolled high blood pressure can have on their health. When hypertension is left uncontrolled it has the ability to become a “silent killer” which serves reason as to why adherence should be continuously reinforced. Exercise is an imperative component of evidence-based treatment for many conditions treated in PT settings, however it is an essential aspect of improving health in those diagnosed with hypertension.[6] Regular exercise has been shown to drastically decrease blood pressure and can potentially eliminate the need for antihypertensive medications when it is accepted as a lifestyle. Exercise may present health risks to patients with hypertension, making it crucial for physical therapists to identify which exercise interventions are appropriate and safe for individual patient.[7]
Patient Education Recommendations
Physical therapists should contribute to educating patients to monitor and manage their blood pressure, as early as childhood, before it becomes a serious health problem. The incidence of pediatric hypertension is increasing as a result of the obesity epidemic. Diet and exercise implemented at a young age is crucial in the prevention of hypertension.[8] When medications are implicated, adherence is crucial in long-term management. It has been shown that approximately 50% of patients don’t take medications as prescribed.[9] According to the WHO, “lack of adherence is the most important cause of failure to achieve BP control”.[9] While medication adherence is important, physical activity should be equally emphasized, especially because it’s a primary prevention technique. Aerobic exercise is universally implemented for hypertensive treatment because it lowers BP 5-7 mmHg among adults. Thirty minutes or more per day of moderate intensity exercise combined with resistance exercise 2-3 days per week is recommended.[10]
Conclusion
Hypertension can be treated by a myriad of drugs, all using different mechanisms of action to effectively treat this common disease. While antihypertensive drugs are beneficial, they may cause clinically relevant side effects such as hypotension and/or orthostatic hypotension. In order to provide the best quality of care, a clinician should be aware of how these previously listed antihypertensive medications work and how it will impact the rehabilitation session.
References
- ↑ The Facts About High Blood Pressure. American Heart Association . http://www.heart.org/en/health-topics/high-blood-pressure/the-facts-about-high-blood-pressure. Accessed November 29, 2018.
- ↑ Oparil S, Zaman MA, Calhoun DA. Pathogenesis of hypertension. Annals of Internal Medicine. 2003;139(9):761. doi:10.7326/0003-4819-139-9-200311040-00011
- ↑ Puar T, Mok Y, Debajyoti R, Khoo J, How C, Ng A. Secondary hypertension in adults. Singapore Medical Journal. 2016;57(05):228-232. doi:10.11622/smedj.2016087
- ↑ High Blood Pressure Fact Sheet. Centers for Disease Control and Prevention. https://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_bloodpressure.htm. Accessed November 29, 2018.
- ↑ American Physical Therapy Association. The Role of Physical Therapists in Medication Management. https://www.apta.org/uploadedFiles/APTAorg/Payment/Medicare/Coding_and_Billing/Home_Health/Comments/Statement_MedicationManagement_102610.pdf.
- ↑ Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. Can Med Assoc J. 2006;174:801–809.
- ↑ Scherer S. Addressing Cardiovascular Risk as Part of Physical Therapist Practice-What about Practice Recommendations for Physical Therapists?. Cardiopulm Phys Ther J. 2009;20(3):27–9. Accessed November 14, 2018.
- ↑ Misurac, J, Nichols, KR, Wilson, AC. Pharmacologic management of pediatric hypertension. Pediatric Drugs. February, 2016; 18(1), 31-43. doi:http://dx.doi.org/10.1007/s40272-015-0151-3. Accessed November 29, 2018.
- ↑ 9.09.1 Brown, MT, Bussell, JK. Medication Adherence: WHO Cares? Mayo Clinic Proceedings. April, 2011; 86(4), 304–314. http://doi.org/10.4065/mcp.2010.0575. Accesed November 29, 2018.
- ↑ Pescatello, LS, MacDonald, HV, Lamberti, L, Johnson, BT. Exercise for Hypertension: A Prescription Update Integrating Existing Recommendations with Emerging Research. Current Hypertension Reports. November, 2015; 17(11), 87. http://doi.org/10.1007/s11906-015-0600-y. Accessed November 29, 2018.