Description
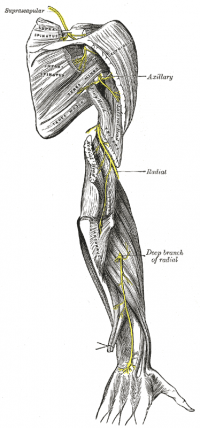
The radial nerve is one of the terminal branches of the posterior cord. In the axilla, it lies behind the axillary and upperbrachial arteries and passes anterior to the tendons of teres minor, latissimus dorsi and subscapularis. It enters the posterior compartment of the arm passing through a triangular space, formed by the lateral humerus, long head of triceps and teres minor. Through this space, the nerve enters the spiral groove of the humerus and descends obliquely between lateral and medial heads of triceps where it reaches the lateral border of the humerus in the distal third of the arm. The nerve enters the anterior compartment by piercing through the lateral intermuscular septum where it continues between brachialis and brachioradialis. Anterior to the lateral epicondyle the nerve splits into its terminal superficial and deep branches.[1]
The posterior cutaneous nerve of the arm arises in the axilla, piercing the deep fascia near the posterior axillary fold. The lower lateral cutaneous nerve of the arm arises before the radial nerve, pierces the intermuscular septum and becomes cuntaneous below the deltoid.[1]
The superior branch of the radial nerve continues on from the radial nerve anterior to the lateral epicondyle. It travels along the anterolateral side of the forearm. It is only function is sensory. In the distal third of the forearm, the nerve rises posteriorly from below the tendon of brachioradialis and pierces the deep fascia to become superior. It the further divides into the digital nerves.[1]
The deep branch of the radial nerve or posterior interosseous nerve, is entirely motor. It begins anterior to the lateral epicondyle of the humerus and enters the posterior compartment of the forearm through the two heads of supinator where it curves around the lateral and posterior surfaces of the radius. It descends between the deep and superficial extensor muscles and lies on the interosseous membrane and ends in a flattened expansion.[1]
=== Root ===[1]
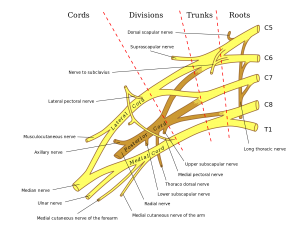
C5, 6, 7, 8 (T1)
=== From ===[1]
Posterior cord of brachial plexus
=== Branches ===[1]
Superficial branch of the radial nerve
Deep branch of the radial nerve (posterior interosseous nerve)[1]
Function
=== Motor ===[1]
Deep branch
=== Sensory ===[1]
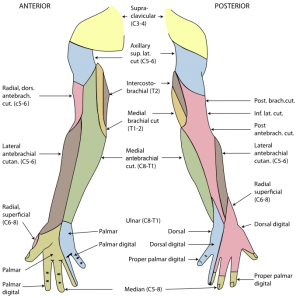
Cutaneous braches supply the skin on the back of the arm and forearm
Posterior cutaneous nerve of the arm
- Posterior surface of the proximal third of the arm
Lower lateral cutaneous nerve of the arm
- Lower lateral part of the arm
- Small area of skin on the forearm
Superficial branch
- Dorsum of the wrist
- Lateral dorsal surface of the hand
- Dorsum of the thumb
- Dorsum of the index and middle fingers
- Dorsum of the lateral aspect of ring finger[1]
Video
Clinical relevance
Radial nerve injuries are associated with the path it travels close to the humerus. Mechanisms of injury can be humerus fracture, a direct blow or sustained pressure (i.e. from incorrect use of a crutch). Motor function of the triceps are usually preserved as they are innervated superiorly whereas wrist and digit extensors are often paralysed leading to the dropped wrist deformity.[1]
A loss of synergic action between wrist flexors and extensors causes excessive and unwanted wrist flexion. This can be observed in a simple gripping task or asking the individual to make a fist. Both tasks will be difficult to complete as movement will be ineffective. Interphalangeal joints can be extended by the lumbricals and interossei due to their attachments at the dorsal digital expansion.[1]
Due to overlapping cutaneous nerves, there is only a small patch exclusive to the radial nerve on the dorsum of the thumb web.[1]
Assessment
Neuro exam
Conduct your standard neurological examination. Look out for these signs[2]:
Weakness:
- Wrist extension
- Abduction of thumb
Deminished sensation:
- Back of thumb, index, middle, and 1/2 ring finger
- back of forearm
Abnormal reflexes
Neurodynamics
The upper limb neurodynamic test for the radial nerve (ULNT2b) is performed with the patient in supine. The joints are moved sequentuailly and to the end of range or until symptoms are produced. Patients are to be instructed to report the onset of any sensation such as stretch, tingling or pain anywhere in the arm or neck.
ULNT2b sequencing:
- Shoulder girdle depression
- Elbow extension
- Shoulder internal rotation
- Pronation
- Wrist flexion
- Shoulder abduction
If a sensation is provoked, differentiation between neurogenic and non-neurogenic sources of pain should be performed. This is achieved by the addition of sensitising movements distant to the pain such as:
- Ipsilateral and contralateral cervical lateral flexion
- Wrist extension or flexion
- Shoulder girdle elevation
It is good practice to perform the test on the unaffected arm first, to establish what is ‘normal’ for the patient. An ULNT is considered positive if it reproduced the patient’s symptoms and a neurogenic source of pain is identified.[3]
Treatment
Manual techniques
Exercises
See also
References
- ↑ 1.001.011.021.031.041.051.061.071.081.091.101.111.121.13 Palastanga, N. P., Soames, R. W., & Nigel Palastanga MA BA FCSP DMS DipTP (2011). Anatomy and human movement: Structure and function (Physiotherapy essentials) (6th ed.). Edinburgh: Churchill Livingstone.
- ↑ A practical guide to clinical medicine. (2015). Retrieved August 30, 2016, from ↑ Schmid, A. B., Brunner, F., Luomajoki, H., Held, U., Bachmann, L. M., Künzer, S., & Coppieters, M. W. (2009). Reliability of clinical tests to evaluate nerve function and mechanosensitivity of the upper limb peripheral nervous system. BMC Musculoskeletal Disorders, 10(1), 11. doi:10.1186/1471-2474-10-11