Definition/Description
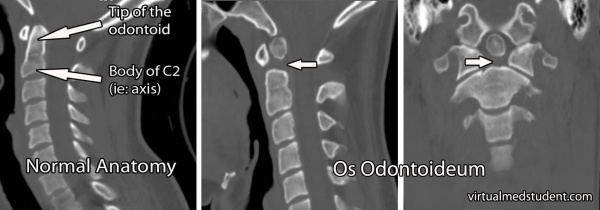
Os odontoideum (OO) is a rare anomaly of the second cervical vertebrae characterised by a separation of a portion of the odontoid process (also called the dens) from the body of the axis. The little bone is marked by a small oval corticated ossicle of which the size can range. The OO can be situated in the position of the odontoid process (orthotropic) or in the vicinity of the base of the occipital bone, more precisely in the area of the foramen magnum (dystopic) with no bony link to the body of the axis.
The classification of the odontoid fractures is known as the Anderson/Alonzo classification:
- Type I : fracture of the upper part of the odontoid peg ; it’s rare and potentially unstable
- Type II : fracture at the base of the odontoid ; unstable, and has a high risk of non-union
- Type III : through the odontoid and into the lateral masses of C2 ; best prognosis for healing because of the larger surface area of the fracture.
Clinically Relevant Anatomy
The dens and the transverse ligaments of the axis are responsible to maintain the diameter of the spinal cord and to stabilise the atlantoaxial joint. The insufficient and unstable dens on which several ligaments are attached to, may render the transverse ligament incapable to stabilise the atlas on the axis which causes cervical instability. This increased atlantoaxial translation potentially leads to upper cervical cord or vertebral artery impingement[1].
Epidemiology/Etiology
The causes of os odontoideum are controversial, and can go from embryological or traumatic causes to even vascular causes[2]. There is evidence that traumatic etiology is the most frequent cause. In this case an atlantoaxial dislocation can possibly appear, which needs a fixation.
The incidence of os odontoideum is unclear and difficult to investigate because symptoms not always occur, but Sankar et al reported that 3,1% of 519 patients with abnormal cervical spine radiographs had os odontoideum[3].The estimated frequency of posttraumatic os odontoideum in combination with atlantoaxial joint dislocation is less than 2% among upper cervical spine injuries[4].
The age at diagnosis varies significantly from the first to the sixth decade of life. Os odontoideum has an increased frequency in patients with Morquio syndrome, Multiple Epiphyseal Dysplasia, and Down syndrome[5].
Characteristics/Clinical presentation
Although the etiology remains controversial over whether os odontoideum is a post-traumatic or congenital condition, the clinical presentation of these two causes remains the same and may vary among persons[6]. As mentioned above, the cervical instability due to the os odontoideum may lead to neurological complaints. Symptoms can include neck, schoulder and/or head pain, pain between the schoulder blades, neck stiffness, headaches and pain radiating in the arms. Serious spinal cord compression might present as weakness, paresthesia or even paralysis in one or all limbs[7]. The patient may also have a decreased cervical spine rotation.
Differential Diagnosis
The os odontoideum is associated with multidirectional instability of C1 on C2[6].
The principal differential diagnosis of os odontoideum is an acute fracture of the odontoid process. Owing to the characteristically smooth cortex of the ossicle and the adjacent C2 vertebral body, the diagnosis of an acute odontoid fracture can be excluded when there is absence of a recent history of acute trauma, without the sclerosis and hypertrophy of the anterior tubercle of the atlas[8].
Diagnostic procedures
The physical examination of a patient with os odontoideum isn’t easy because there is no specific sign accepted as proof of this anomaly. Though there are several symptoms like cervical instability and neurological signs to suspect os odontoideum. Therefore, a neurological screening examination including deep tendon reflexes of the upper and lower extremities, a sensory examination, a myotomal screen and tests for upper motor neurone signs (Hoffman’s sign) should be considered.
Cervical instability can be detected primarily by the following provocative test: a passive upper cervical flexion or extension is performed. While maintaining the end range, a translation is introduced. The test is positive when symptoms are reproduced or excessive translation occurs. Cervical instability is now suspected, and craniovertebral ligamentous stress tests like Alar ligament test, Transverse ligament test (also called Anterior shear test), lateral displacement test, upper cervical flexion test and the Sharp Perser test should be performed to specify the instability[1].
The Sharp Purser test is used to evaluate the anterior stability of the atlantoaxial joint, caused by an insufficiency of the transverse ligament. The patient is sitting down while keeping the head (maximum) in flexion. The therapist fixes C2 with a pinch grip, and gives pressure on the forehead of the patient with the other hand, with the intention to translate the occiput and the atlas to posterior. This results in a positive test when the symptoms are provoked by bending the head, and reduce during the translation.
Examination
There are a few options to examine and to confirm the os odontoideum.
The first possibility is a radiological examination, taking cervical radiographs in different positions:
- Lateral cervical radiograph,
- Neutral position (Figure 1),
- Extension (Figure 2)
- Flexion (Figure 3),
- Anteroposterior open-mouth view
- Neutral position
- Lateral flexion, in both sides: left and right.
- Other medical image used to examine and confirm or exclude os odontoideum is the CT-scan and MRI (Computed tomography and magnetic resonance imaging), taking a coronal and a sagital image or a T2-weighted MR image.
Medical Management
The management starts with a complete history, followed by a physical examination, to end with imagining studies. In general, those damages that are causing or already caused neurologic injury, chronic pain, or spinal deformity or can give the patient a high risk for emerging these necessitate treatment[9].
An alternative to surgical stabilization is conservative treatment, involving rigid or non-rigid immobilization this may result in non-union and prolonged fracture instability, requiring secondary surgery[10][11].
Surgery is not necessary when the patient does not have complaints. Only when one of the following characteristics occur:
- Spinal instability: defined when following characteristics are radiographically present[5]:
- Posterior atlantodens interval less than 13mm
- Sagittal plane rotational angle more than 20°
- Instability index more than 40%
- C1-C2 translation more than 5mm
- Neurological symptoms
- Uncontrollable pain
Surgical possibilities:
- Midline wiring and Onlay grafts
- Brooks fusion (the most satisfactory)
A Gardner pin-vise headholder is attached to the patient’s head is needed to maintain a firm traction on the head portion. It must be certain that the head-thorax relationship does not change. Before the operation can start, the shoulders have to maintain the depression. Therefore they use strips of tape and apply counter-traction[12].
To control the alignment, a lateral roentgenogram is made, if there’s no perfect alignment (anterior or posterior misalignment), it can be corrected with extreme care. The operation consists of a midline incision from the occipital protuberance to the third cervical vertebra. A gauge stainless-steel wire is bending back at its midpoint. The wire is twisted clockwise using the needle-holder while an assistant holds the ends with two haemostats about 30 centimetres apart. The wire is twisted to make about 3 turns per centimetre, producing a cable with a smooth loop at the bend end. During this procedure the head is maintained in continuous traction.
Two cortical cancellous bone grafts are removed from the posterior superior iliac spine. They should be slightly larger than the aforementioned dimensions and by careful measurement should be fitted between the lamina of the axis and the posterior ring of the atlas, one on each side of the midline. The grafts are notched to keep the wires from slipping medially or laterally.
A soft collar or head-thorax brace is used during the first postoperative days. The patient is encouraged to sit up in bed the day following surgery and to be up and walking as soon as tolerated.
Physical Therapy Management
Physical therapy is considered when the patient is still young or when there is no radiographic evidence of significant instability, neurological symptoms or uncontrollable pain. The therapy consists of traction and three to six months in a Minerva jacket or a brace. In most patients leads this therapy to fusion of the atlanto-axial joint.
The goal of the physical therapy treatment for cervical instability is to enhance the function of the spinal stabilising subsystems and to decrease the stress on the involved spinal segments. Posture education will decrease the stress on the passive subsystem (which consists of capsules and spinal ligaments) by reducing the loads on the segments in end range and by returning the spine in a biomechanical efficient position. To enhance the active subsystem (muscles and tendons) strengthening exercises are required. In the cervical region, the multifidus (posterior) and the longus coli and capitus provide stability and therefore improve the quality and control of movement occurring within the neutral zone. Exercises should be focused on controlled motion and proprioception[13][14]. It is important to be aware of the fact that os odontoideum is an absolute contraindication to upper cervical manipulation[7][14].
References
- ↑ 1.01.1 Mintken, PE. et al. upper cervical ligament testing in a patient with os odontoideum presenting with headaches. Journal of orthopaedic & sports physical therapy. 2008; 38(8): 465-475.
- ↑ Weng, Chong MD, PhD; Tian, Wei MD, PhD; Li, Zhi-Yu MD; Liu, Bo MD; Li, Qin MD; Wang, Yong-Qing MD; Sun, Yu-Zhen CN, Surgical Management of Symptomatic Os Odontoideum With Posterior Screw Fixation Performed Using the Magerl and Harms Techniques With Intraoperative 3-Dimensional Fluoroscopy-Based Navigation, Spine Issue: Volume 37(21), 01 October 2012, p 1839–1846.
- ↑ Sankar WN, Wills BP, Dormans JP, Drummond DS. Os odontoideum revisited: the case for a multifactorial etiology. Spine. 2006;31:979-984. [level of Evidence 2]
- ↑ Moreau, PE, et al. traumatic atlantoaxial dislocation with odontoid fracture: a case report. Orthop Traumatol Surg Res. 2012 Sep;98(5):613-7.
- ↑ 5.05.1 Truumes, E. et al. Os odontoideum. Medscape 2012.
- ↑ 6.06.1 HENDERSON, S., HENDERSON, D., Os odontoideum with associated multidirectional atlantoaxial instability: imaging and clinical considerations. J Can Chiropr Assoc. 2006 June; 50(2): 111–117.
- ↑ 7.07.1 Crnec, M. et al. Os odontoideum: a case report. J Can Chiropr Assoc. 1986 June; 30(2): 83–85.
- ↑ WANG, X., FAN, C.Y., LIU, Z.H., The single transoral approach for Os odontoideum with irreducible atlantoaxial dislocation. Eur Spine J. 2010 July;19 Suppl 2: 91-95.
- ↑ Klimo, P; Rao, G; Brockmeyer, D, NEUROSURGERY CLINICS OF NORTH AMERICA Pages: 463, JUL 2007.
- ↑ Spierings EL, Braakman R, The management of os odontoideum : Analysis of 37 cases. J Bone Joint Surg Br. 1982;64(4):422-8.
- ↑ Griswold DM, Albright JA, Schiffman E, Johnson R, Southwick W, Atlanto-axial fusion for instability, J Bone Joint Surg Am, 1978 Apr;60(3):285-92.
- ↑ Dai L, Yuan W, Ni B, Jia L, Os odontoideum : etiology, diagnosis and management. Surg Neurol. 2000 Februari 2000 Feb;53(2):106-8; discussion 108-9.
- ↑ Olson, K.A. et al. Diagnosis and treatment of cervical spine clinical instability. JOSPT. 2001;31(4):194-206
- ↑ 14.014.1 ARUN P.S. , “What is os odontoideum”, Bone and Spine, 2012.