Introduction
The goal of any rehabilitation is to restore function to the greatest degree in the shortest time, helping people return to their function with minimal risk of re-injury. While absolute rest and offloading may relieve symptoms, they are associated with negative potentials such as decreased tissue tolerance and increased tissue vulnerability in the future.
Understanding how tissues respond to physical stress and mechanical loading is helpful in achieving a balance between stabilising an injured tissue and avoiding detraining.
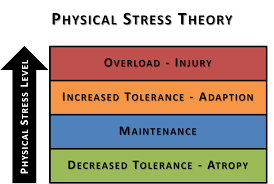
Physical Stress Theory
According to Mueller and Maluf[1], biological tissues adapt to changes in the levels of applied stress. Maintaining tissue tolerance is essential to prevent atrophy, whereas overloading results in hypertrophy. Excessively high levels of stress lead to tissue injury and potential permanent damage. The magnitude, time, and direction of stress application determine the overall level of exposure to physical stress. Injury may occur due to a high-magnitude stress applied for a brief period, a low-magnitude stress applied for a long duration, and/or a moderate-magnitude stress applied to the tissue many times.
Mechanotransduction Hypothesis
Refers to the conversion of mechanical loads on the cellular level resulting in structural changes. Increased bone thickness and width in response to mechanical loading is the classical example of this hypothesis. Regardless of the type of loading, torsional, compressive or tensile, the mechanical stimulus triggers a release of various chemicals which in turn result in building up layers of tissue and improves load tolerance[2].
This hypothesis is aligned with a sub-principle of Wolff’s law that tissues adapt to the specific applied loads. Exposure to compressive loads, for instance, will qualify the tissue to tolerate the same type of applied loads exclusively[3]. This means that before a patient can return to their sport or activity the injured tissue needs to be exposed to that specific level of load. [4]
Physiologically stressing the tissue, below the level of injury, with sufficient time for adaptation causes cellular response that strengthen the tissue and improves its tolerance.
Mobility and Stability
Maintaining mobility while stabilising an injured tissue is required in successful rehabilitation. The key here is to avoid rigidity. Muscular rigidity refers to Co-contraction, occurring in response to pain and/or kinesiophobia. Appropriate level of co-contraction allows mobility to occur once stress is minimised.
The Influence of pain on movement and motor control
Pain has a massive influence on our movement patterns. As a pain avoidance strategy, a person with injured ankle may acquire an antalgic gait. Walking with slight planter flexion and short strides may later develop to a compensatory foot pronation, knee valgus and hip adduction moment, thus affecting tissue loading patterns.
Another example is seen when a person develops a co-contraction of Erector Spinae muscle due to flexion-related LBP. This rigidity results in excessive hip movement to compensate for the loss of lumbar flexion. Additionally, the excessive lumbar extension may cause increased load on facet joint and posterior disc elements.
The fear of movement could possibly develop to catastrophising and complicate the conditions. Therefore, we need to consider the central elements of pain by implementing desensitization in the rehabilitation program.
(See Rehabilitation Considerations
Teaching the movement involves various levels of learning: [4] Instructing patients depends on the stage of learning. In the first stage, clause skill is used to eliminate all external influences and drives the focus internally (Intrinsic focused cues) by asking patient to reflect on the purpose and the mechanism of a simple movement e.g. single leg squat. Repetitions in this stage aids cognition and acquisition. In Retention and Transfer stages, training should be external or goal focused. For example, asking patient to move towards a certain target, or doing a task while keeping trunk ahead of knees. The ultimate aim of motor skill learning is to transfer the skill to performance in sport or activities of daily living. The patient needs to move from closed skill tasks (same movement tasks in stable predictable environments) to open skill where tasks/movements are unplanned.
Teaching motor skill can be done by either training the whole or only a section of the task: [4] Feedback during motor learning:[4] Feedback can be either intrinsic or extrinsic. Intrinsic feedback – seen as the knowledge of performance but in can be limiting to learning when in extreme. Extrinsic (augmented) feedback can be from visual demonstrations, using a mirror, verbal instructions or guidance through touching.
The rehabilitation then should develop complexity to mimic the reality of patient’s occupation or functional aspirations.
Random Skill training can be acquired in this stage, by training patient to deliver function on various surfaces, with different external loads and to react to external stimuli.
Selecting meaningful exercises that relate to patient’s function to improve proprioception. Exercises should also fit patient’s physical outcomes when planning a rehabilitation program. Adaptive and progressively challenging exercises allow tissue stress to occur in accordance with the above mentioned principles.
For task learning to be carried out successfully, it should be built on several pillars: flexibility, stability, work capacity (muscle endurance) and strength. The elements of strength stretch beyond the ability to deliver high force against relatively low repetition to include generating force rapidly (acceleration), force absorption and eccentric force generation.
To deliver the appropriate level of loading, we need to form a baseline of the patient’s functional capacity. Communication is essential to understand the functional needs and goals of our patients. Then we would perform ”Performance Backwards Thinking” by having a certain goal in our minds then go back in stages to retrofit that goal with the patient’s level of activity.
Firstly, find out what the end goal is, meaning what is the functional activity the patient want to return to.
Then determine what physical abilities the patient will need to reach this goal. These are components that should be considered:
Evaluating tissue damage, cardiovascular capacity, strength and stability can help prevent detraining. Also, one of the important factors is to eliminate triggers of tissue damage. This includes sources that may not be usually considered as injuring. For example, an individual with an ankle injury who sleeps with a heavy cover on their feet, pushing it into more plantar flexion, need to adapt by either sleeping with socks or put a lighter cover over their feet.
Chronic capacity is the ability to deliver function over multiple occasions. A person with higher chronic capacity on a higher baseline ability to cope with load is less likely to be affected by massive increase in load[6]. In rehabilitation of an injured tissue, special attention should be given to building tolerance and capacity in multiple directions. For example, directing hamstring specific training may lead to reduced adductors capacity if not included in the training[7]. The goal is to make sure that the patient’s chronic capacity is sufficiently increased so that any acute load increase would not overload the tissue. [4]Motor Skill Learning
Re-loading Rehabilitation
Generate a Needs Analysis [4]
Building Chronic Capacity
Identifying Load[4]
How much load can the injured tissues tolerate? (Safe loads)
How to [4]
- Increased swelling of the training muscles indicates inflammation-overload. Circumferential measures: to be taken after the activity, in the morning and in the evening. Ideally swelling should not increase between days. If it was increased after training it should decrease by the evening, if it is still swollen by the next morning then the training load should be decreased.
- Pain: VAS 0-10, rate the score to a specific movement or exercise. Any change in score the day after training >1 that does not reduce by the evening may indicate overload
- Stiffness: especially in the morning, is a good mark of inflammation. Link the stiffness to a specific task or movement for e.g. simply ask the patient if they find difficulties doing a simple full squat in the morning.
- Global loads: technological applications and trackers could be helpful in giving a start point to build up a gradual progressive rehabilitation program without overloading or deloading.
Progressing Load[4]
Load Balance
- It is important that the initial load in a rehabilitation program is not too high as it can lead to injury, but if it is too low it will lead to atrophy. Atrophy occurs within 5-24 days of no activity.
- It is important to understand how the tissue responds under load
- Pain should be well managed as it can negatively impact the rehabilitation
Frequency of load[8][9][4]
- Acute:chronic load ratio is the amount of training the patient has completed during the period of rehabilitation compared with the what is needed for a full training session.
- Acute load is the training done in 1 week and chronic load is the average acute load / training done in the last 4 weeks. The ratio between acute and chronic shows if the acute workload is greater or less than the total workload of the weeks before it
- A acute:chronic workload of 0.5 means that the patient trained/competed half of what was prepared for the 4 weeks prior
- A ratio of 2.0 means the patient did twice as much, anything more than 1.5 is seen as a spike in training and could be seen as an injury risk.
- E.g. a patient with a adductor strain would after time off to recover have an increased risk of injury even though the patient might be able to run pain free.
- E.g. a patient with hip/knee osteoarthritis who were in bed with flu will have an increased risk of acute:chronic load ratio when returning to full activity.Task specific training (example – depending on the patient and the load)
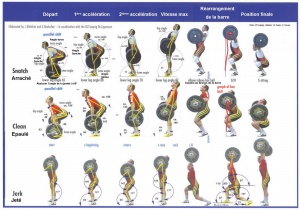
Task specific training [4]
- Avoid global detraining, as it will compromise the patient’s fitness to return to the sport
- Start with controlled exercises like closed-chain exercises depending on the load the patient can take (squats, single leg squats, lunges, step ups etc)
- Progress to increasing the load and change the surface to challenge the patient’s stability
- When the patient is able to accept load on the affected side under multidirectional loads then progress to load acceptance in bilateral and unilateral landing activities moving towards running. Then progress these activities over barriers and then to different directions.
- It is important to reload the patient to fulfil in the needs of their sport or the activities that are important
- Increase the patient’s chronic capacity sufficiently so that any acute load increase would not overload the tissue
Additional Resources
References
- ↑ Mueller MJ, Maluf KS. ↑ Khan KM, Scott A. ↑ Frost HM. ↑ 4.004.014.024.034.044.054.064.074.084.094.10 Chapter 10. Principles of Exercise Rehabilitation. Physical Examination, in: Petty NJ. Neuromusculoskeletal examination and assessment: a handbook for therapists. Elsevier Health Sciences; 2011 Jan 27.
- ↑ Three stages of learning movement. Available from: ↑ Gabbett TJ. ↑ Cook JL, Docking SI. “Rehabilitation will increase the ‘capacity’ of your… insert musculoskeletal tissue here….” Defining ‘tissue capacity’: a core concept for clinicians. Br J Sports Med. 2015 Dec;49(23):1484-5
- ↑ Blanch P, Gabbett TJ. ↑ Bowen L, Gross AS, Gimpel M, Li FX. ↑ Understanding Fear-Avoidance Beliefs and Chronic Pain. Available from: