Definition/Description
Pelvic organ prolapse is the descent of a pelvic organ into or outside of the vaginal canal or anus. It mainly results from pelvic floor dysfunction.[1]
There are several types:
- Cystocele: prolapse of the bladder into the vagina [2]
- Urethrocele: prolapse of the urethra
- Uterine prolapse [2]
- Vaginal vault prolapse: prolapse of the vagina [3]
- Enterocele: small bowel prolapse
- Rectocele: rectum prolapse [2]
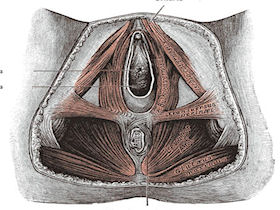
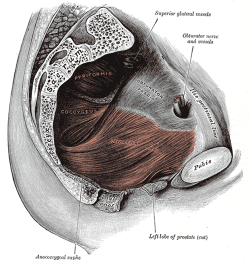
Clinically Relevant Anatomy
Please see this page for a detailed overview of pelvic floor anatomy.
Etiology
Pelvic organ prolapse has a multifactorial etiology. It is likely caused by a combination of physiological, anatomical, reproductive, genetic and lifestyle factors that interact and contribute to dysfunction of the pelvic floor. [3]
Symptoms
A variety of symptoms may be present including:
- Vaginal bulging [4]
- Feeling of pelvic pressure or heaviness [4]
- Pelvic pain [4]
- Urinary or fecal incontinence or obstruction [4]
- Altered daily activities, sexual function and quality of life [4]
Risk Factors
The factors causing pelvic organ prolapse are different between patients.[3] Risk factors include the following:
Primary Pelvic Organ Prolapse
- Pregnancy and labour [2]
- Obesity/BMI [1] [3]
- Respiratory problems involving a chronic, long-term cough [2]
- Cancer of the pelvic organs [2]
- Hysterectomy (surgical removal of the uterus) [2]
- Genetics (possibly) due to weaker connective tissues [2]
- History of vaginal delivery increases the risk 5.56 times [3][1]
- Hypertension and Diabetes Mellitus combined increase the risk by 1.9 times [1]
- Increased birth weight [1]
- Age [3]
- Parity [3] (i.e. the number of times a woman has given birth to a fetus with a gestational age of greater than or equal to 24 weeks, alive or stillborn) [6]
Pelvic Organ Prolapse Recurrence (after native tissue repair)
- Preoperative stage 3 or 4 pelvic organ prolapse (i.e. a more severe prolapse) [3]
Treatment/Management
Treatment for pelvic organ prolapse usually involves either conservative management (for mild prolapse or women who are not good surgical candidates) or surgery. Conservative treatments include pelvic floor muscle training and the use of devices (pessaries). [4]
In a study by Panman et al in 2016, examining the two-year effects of pelvic floor muscle retraining, it was demonstrated that in women aged 55 and greater with symptomatic mild pelvic organ prolapse, pelvic floor muscle retraining results in a significant decrease in pelvic floor symptoms when compared to watchful waiting (note: statistically significant but below the minimal clinically important difference). [4]Additionally, it was found that pelvic floor muscle retraining was more effective in women who experienced increased pelvic floor symptom distress at baseline. [4] Conversely, the same study found no difference in sexual functioning, quality of life, function of the pelvic floor muscles or degree of prolapse. [4]
Pelvic floor muscle retraining included:
- Explanation and description of the pelvic floor [4]
- Instruction regarding how to contract and relax pelvic floor muscles [4]
- If unable to perform this task, use feedback through digital palpation [4]
- If insufficient control demonstrated, use myofeedback or electrical stimulation [4]
- General exercise program provided, subsequently modified for individual needs [4]
- Taught correct technique for contracting pelvic floor muscles before and during increases in abdominal pressure [4]
- Received information about washroom habits and lifestyle [4]
- If pelvic floor muscles were overactive, focus was on relaxation rather than contraction [4]
- Face-to-face contact with physiotherapist as well as encouragement to maintain practice at home 3-5 times per week, 2-3 times per day [4]