This section is dedicated to the rare conditions diagnosed in the pediatric population. 

Kosair Childrens Hospital
Pediatric Rheumatology
Multiple Sclerosis Foundation
Failure to Thrive
National Organization for Rare Diseases
The Global Genes Project
Autism Spectrum Disorder and Autism[1] 


Definition
Group of complex disorders of the brain. Varying degrees of characteristics including: difficulties in social interaction, verbal and nonverbal communication and repetitive behaviors.
- Autism Spectrum Disorder (ASD): can display with intellectual disabilities, difficulties in coordination and attention and physical health issues.
- Autism: most obvious signs and symptoms tend to emerge between 2 and 3 years old
How common is Autism and ASD?
- ASD: Affects over 2 million individuals in the United States
- Autism:
- Effects ~1:88 children
- ~4-5 more times likely in boys than girls
- An estimated 1 out of 54 boys and 1 in 252 girls are diagnosed in the United States
Causes
- No one cause
- Rare gene changes Most cases are a combination of gene changes and environmental factor
- Risk factors (do not cause autism by themselves, but could have an influence when combined with genetic risk factors):
- Clearest evidence involve events before and during birth
- Advance age at conception
- Maternal illness during pregnancy
- Difficulties during birth (i.e. Oxygen deprivation)
- Genetic risk factors (Autism tends to happen more frequently in the following conditions)[2]
- Fragile X Syndrome
- Tuberous sclerosis
- Congenital rubella syndrome
- Untreated phenylketonuria (PKU)
How is ASD/Autism diagnosed?
- No specific medical test
- Administer autism-specific behavioral evaluations
- Parents usually notice:
- Failure to make eye contact
- Not responding to their name
- Playing with toys in unusual or repetitive ways
-


- Typical diagnosis involves a multidisciplinary team
- Genetic testing may be recommended
Resources
Kentucky Autism Training Center
Autism Society of Kentuckiana
- Has news, research and ways to get involved
- Section about living with Autism
Cerebral Palsy (CP)


Definition
Disorder of movement, muscle tone or posture that is caused by injury or abnormal development in the immature brain.[3]
How common is CP? [4]
- Usually not diagnosed until the age of 2 or 3
- ~2-3:1,000 children over the age of three have the condition
- ~500,000 children and adults have CP in the United States
Types[4]
- Spastic:
- ~70-80% of cases
- Associated with stiff muscles, making movement difficult
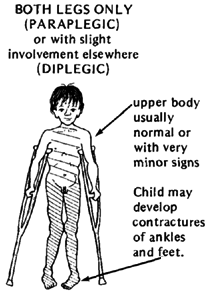
- Spastic diplegia:
- Both legs are affected
- Causes tight muscles in the hips and legs
- Inward turned legs leading to crossed knees (scissoring)
-
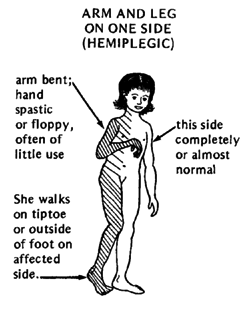
- Spastic hemiplegia:
- One side of the body affected
- Arm often more affected than the leg
- Spastic hemiplegia:
-
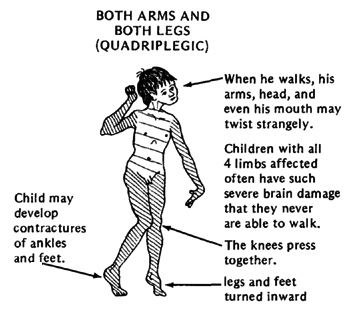
- Spastic quadriplegia:
- Most severe
- All four limbs and the trunk are affected
- Often also affect muscle of tongue and mouth
- Spastic quadriplegia:
- Athetoid or Dyskinetic:
- 10-20% of cases
- Affects entire body
- Fluctuations in muscle tone
- Uncontrolled movements
- Difficulty with:
- Learning to control body
- Sucking
- Swallowing
- Speech
- Ataxic
Causes[3]
- Abnormality or disruption in brain development
- Random mutations in genes
- Infections of the mother that would affect the developing baby
- Disruption of blood supply to the developing brain
- Lack of oxygen to the baby’s brain
- Infant infections leading to inflammation around the brain
- Traumatic head injury
Risk factors[3]
- Mother’s health:
- Certain infections or health problems significantly increase the chance to giving birth to a baby with CP:
- Infant’s health:
- Certain illnesses in a newborn significantly increase the chance of the baby developing CP:
- Bacterial meningitis
- Severe or untreated jaundice (yellowing of the skin)
- Viral encephalitis
- Certain illnesses in a newborn significantly increase the chance of the baby developing CP:
- Other factors:
- Premature birth
- Low birth weight
- Breech births
- Multiple babies
How is CP diagnosed?[3]
- Signs and symptoms usually appear during infancy or preschool years:
- Impaired movement associated with:
- Brain scans:
- MRI: usually the preferred test to use, will usually be given a mild sedative to remain still
- Cranial ultrasound: can provide a preliminary assessment, placed over the soft spot (fontanel) of the baby’s head
- CT scan: will likely be given a mild sedative to remain still
- Electroencephalogram (EEG):
- Done if the child has a history of seizures
- Records the electrical activity of the brain
- Used to determine if child has epilepsy
- Lab tests:
- Blood is checked to rule out other conditions
- May also screen for metabolic or genetic problems
- Additional tests:
- If diagnosed with CP, may go through these other tests to screen for other associated conditions:
- Vision impairment
- Hearing impairment
- Speech delays or impairments
- Intellectual disabilities or mental retardation
- Other developmental delays
- If diagnosed with CP, may go through these other tests to screen for other associated conditions:
Resources
Definition
Genetic disorder occurring when the individual has full or a partial copy of chromosome 21. This extra genetic material causes an alteration in the development of the child.
How common is Down’s Syndrome?
- Most common genetic disorder
- ~1:691 babies are born each year with Down’s Syndrome
- ~6,000 babies are born each year with Down’s Syndrome
Types
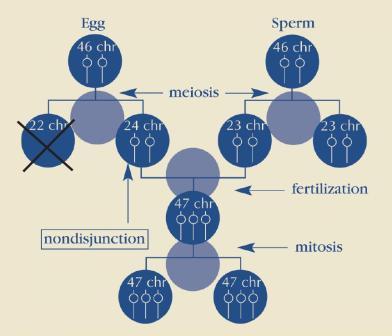
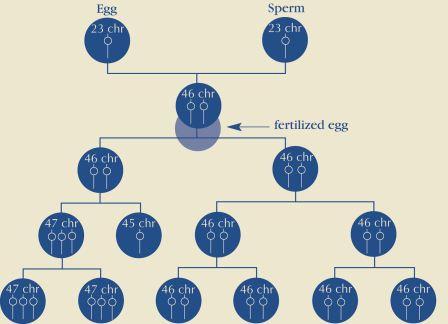
- Trisomy 21 (Nondisjunction):
- The pair of the 21st chromosome fails to separate
- Extra chromosome is replicated in every cell in the body
- Accounts for ~95% of cases
-
- Mosaicism:
- Nondisjunction takes place in chromosome 21 in one cell but not all cells
- Accounts for ~1% of cases
- May have fewer characteristics than other types of Down’s Syndrome
- Mosaicism:
-
- Translocation:
- Part of chromosome 21 breaks off during cell division and attaches to another chromosome, typically chromosome 14
- Accounts for ~4% of cases
- Translocation:
Causes
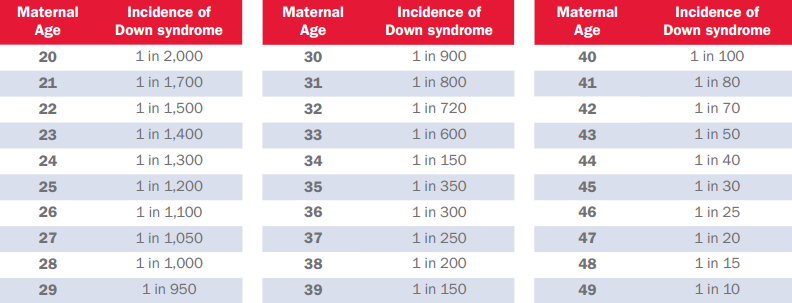
- Cause of non-disjunction is currently unknown:
- Research suggests the likelihood increases as women age
- No definitive research suggesting environmental factors of the parents before or during pregnancy
-
- Note: Age 34 is not accurate. NDSS has noted the error but has yet to find out the correct information.
How is Down’s Syndrome Diagnosed?
Prenatally
- Screening tests:
- Most only provide a probability
- Blood test: measures quantities of various substances in the mother’s blood
- Ultrasound: checks for “markers”
-
- Diagnostic tests:
- Can provide a definite diagnosis with almost 100% accuracy
- Carry up to a 1% risk of causing a spontaneous termination
- Chorionic villus sampling (CVS): usually performed in first trimester between 9 and 11 weeks
- Amniocentesis: usually performed in the second trimester after 15 weeks
- Diagnostic tests:
At birth
- Usually identified by certain physical traits:
- Low muscle tone
- Single deep crease across the palm of the hand
- Slightly flattened facial profile
- Upward slant to the eyes
- Chromosomal analysis may also need to be done to confirm the diagnosis:
- This is done by drawing a sample of the baby’s blood
Resources
Activities and Equipment Sites for the Pediatric Population
Below are websites for you to look around for fun activities to enjoy outside of therapy sessions:Below is a list of equipment sites for you to look around:
References
- ↑ Autism Speaks. It’s Time to Listen. Available from:↑ Autism Society. Improving the Lives of All Affected by Autism. Available from: ↑ 3.03.13.23.3 Mayo Clinic. Cerebral Palsy. Available from:↑ 4.04.1 American Pregnancy Association: Promoting Pregnancy Wellness. Cerebral Palsy. United Cerebral Palsy. Available from:↑ National Down Syndrome Society. Down Syndrome. National Down Syndrome Society. function gtElInit() { var lib = new google.translate.TranslateService(); lib.setCheckVisibility(false); lib.translatePage('en', 'pt', function (progress, done, error) { if (progress == 100 || done || error) { document.getElementById("gt-dt-spinner").style.display = "none"; } }); }
Ola!
Como podemos ajudar?