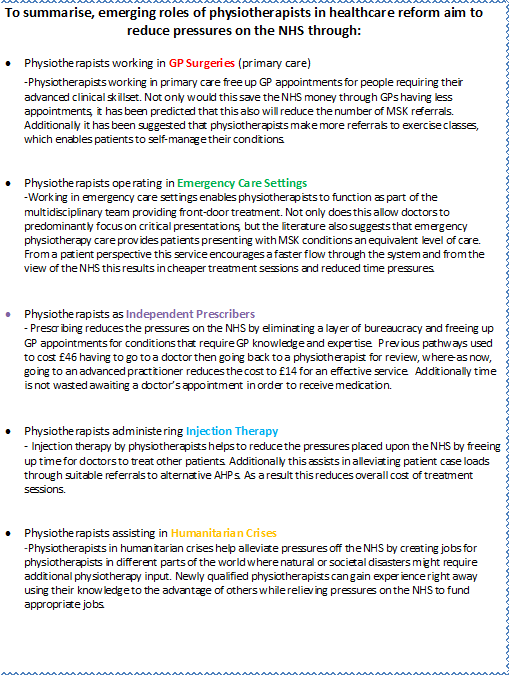
The objective of this learning resource is to provide a developmental tool for students, recent graduates and junior physiotherapists at a time where integration of health and social care is both a priority and necessity to reduce pressures on the National Health Service (NHS). Through the discussion of five emerging roles, this aims to give them the knowledge and confidence to expand their future physiotherapy practice from what was once a traditional ‘mono-role’ into something advanced, exciting and current . Following junior clinical years, allied health professionals inevitably branch into specialisms as their career progresses. This puts them in key positions to explore current emerging roles and alternative physiotherapy pathways to accomodate the ever-changing population and a result physiotherapy practice is being undertaken in a variety of untraditional settings that would have originally been unheard of.
‘Success requires not only the right vision but also the right workforce’ [1]
“The contribution of physiotherapy to the nations health has often been underrated…get data on outcomes, research objectively and show what you do and why it is cost-effective…take physiotherapy over bridges into areas where it hasn’t been traditionally.”
“You are the hope for the future, you can transform healthcare and take it to places that managers, doctors, nurses can’t do on their own. They need you, you’re essential. Go out there and be confident in bringing about changes”.
– Baroness Ilora Finlay – CSP President and consultant in pallative care Founders lecture; CSP annual Conference ; Physiotherapy UK 2015, Liverpool
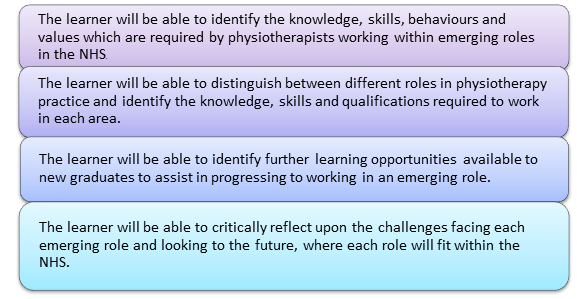
On completion of this page:
This resource is an informative package for current students, recent graduates and junior physiotherapists covering five emerging physiotherapy roles within the NHS. We will explore these roles independently and analyse how these fit into the [2] and the [3]. We will also consider the pressures on the NHS at present and how each of the emerging roles we have decided upon will impact NHS service provision. In order to facilitate the reader’s understanding of the information presented, we have included direct quotes from various professionals working in these roles and also some video interview links in order to gain greater insight into their views and experiences.
Content
We are aware that divergences from traditional clinical practice are extensive and as a result there are many other roles that we will not be covering in this resource. We have therefore put together a lengthy reference list for which the reader to utilise at their leisure.
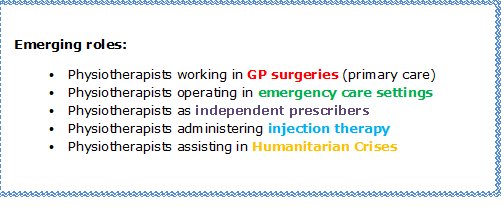
The five following roles have been selected for review as they have all been recent topics of discussion in the physiotherapy magazine”Frontline” and also at the annual physiotherapy UK conference and trade exhibition 2015 in Liverpool. The roles we have selected all direct from the main theme of the resource, which is relieving pressures on the NHS.
In order to set the scene for the discussion of these roles, we have included information regarding different levels of physiotherapy practice and workforce development. This is aimed at enhancing the reader’s baseline understanding of physiotherapy career pathways.
We intend to facilitate the learner’s deeper understanding of these topics with opportunities for reflection and learning questions throughout. These will be outlined with the symbol:
In order to set the scene for the resource, we have provided the reader with a brief overview of the key levels of physiotherapy practice.Currently there are 51, 044 registered physiotherapists working in the UK[4].
Band 5
To be a band 5 junior physiotherapist, you have to hold a degree or diploma in physiotherapy, be registered with the HPC (Health profession Council) and a member of a relevant professional body (Charted society of Physiotherapy). Clinically, you will be under supervision of a band 6 physiotherapist.
What the role entails
When a applying for a band 5 physiotherapy job, there are many Band 6
To become a band 6 physiotherapist you must specialize in a specific area of physiotherapy, for example paediatric orthopaedics. Requirements for current band 6 positions within the NHS are as follows: qualified physiotherapist registered with the HPC and a relevant professional body (Chartered Society of Physiotherapy), a minimum of 1 year NHS experience.
The following are some examples of the Advanced Practitioner
It was during the Vietnam War that advanced practicioner roles for physiotherapists first emerged in the United States, and for around 20 years have been part of the national health framework for allied health professionals in the United Kingdom[5].
The real contribution of Advanced AHP Practitioners is being innovative in their thinking around service provision, being a role model and mentor to junior practitioners, having excellent communication skills and working productively in new models of service delivery[5].
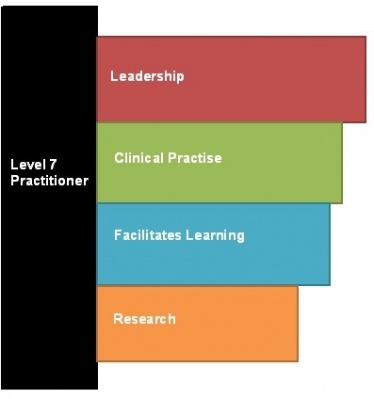
Currently the roles and responsibilities of advanced practitioners are defined by the setting in which they work. Leadership and management are two major responsibilities of practitioners working in AP roles. The following picture on the right shows the 4 pillars of advanced practice.
The career framework of health, as shown above is a 9 level framework whereby roles are grouped according to their level of responsibility and complexity in clinical practice, and the level of education and experience required for the job. Advanced practitioners are required to have a Masters degree according to the Scottish Credit and Qualifications Framework (2009) and they will typically work at level 7 on the Career Framework for Health.
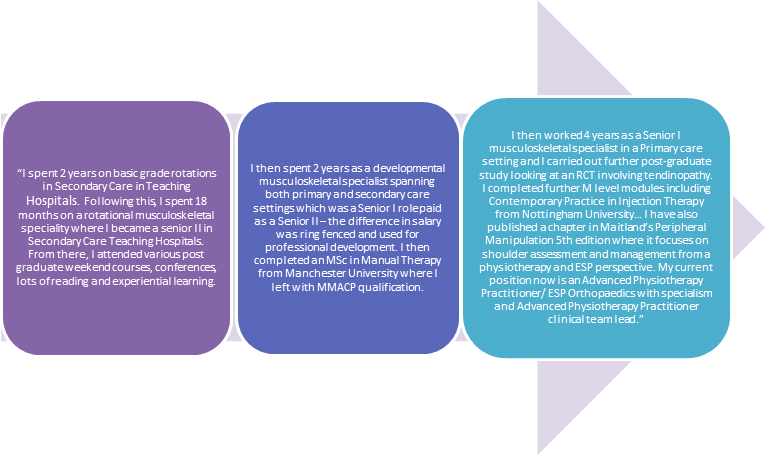
The picture above, on the left shows the journey advanced practitioner Annalisa Newson has taken to get to where she is today[6].
Extended scope practitioners are physiotherapists working at a high level of expertise who have extended their practice and skills in a specialized clinical area. Examples of extended areas of practice will be discussed in this resource, including injection therapy and prescribing rights. ESPs work in primary and secondary care, and they examine patients referred for orthopeadic triage by a GP.
ESPs work alongside medical professionals due to growing demands on doctors and medical consultants. They are able to order scans, x-rays and blood tests, basically encompass tasks that may have previously been undertaken by the medical profession.[7] They are also able to do injection therapy and prescribing with the accredited training and courses. The patient’s management is also determined by the ESP through a series of investigations. Referrals can also be made to physiotherapy or other disciplines such as podiatry or orthotics.[8] The UK is a world-leader in physiotherapy, with physiotherapists working with greater autonomy and challenging practice. According to the GNC the UK has more specialist than most and it has been suggested that other countries such as Australia look to the UK service for innovation in the development of their own practice [9]. Back in 2002, the first consultant Physiotherapist, Dr Paul Watson was appointed at University Hospitals Leicester Trust.
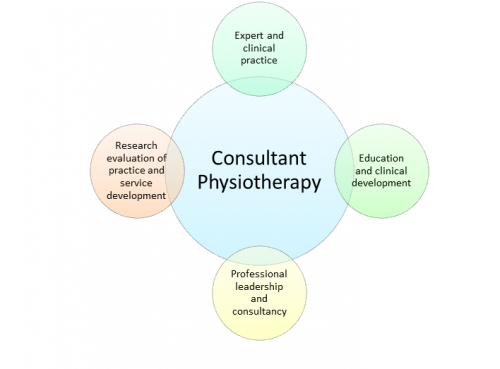
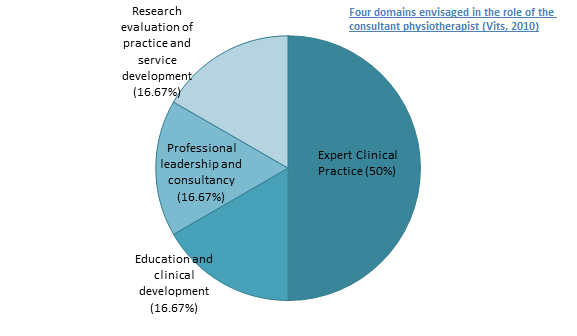
Consultant Physiotherapists go beyond the boundaries of the profession, providing leadership and strategic vision through four main domains[10]: expert and clinical practice, education and clinical development, professional leadership and consultancy, and research evaluation of practice and service development. These areas were envisaged as being fundamental in the development of an allround professional, providing post-holders with opportunities to develop their career pathways, impacting clinical protocols and service provision. It was viewed that these consultants could operate as primary practitioners, shifting care from hospitals into the primary care setting helping to cut waiting times[11].
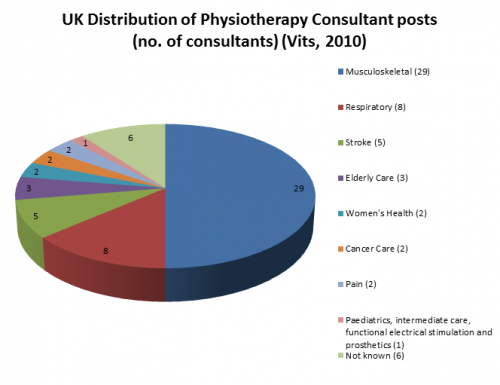
Challenging The Department of Health’s 2001 target of 250 new consultant allied health professional (AHP) posts by 2004 was the lack of allocation of appropriate funding to support these new posts. In 2009 it was calculated that approximately 123 consultant AHP posts were occupied nationwide, 64 of which were thought to be registered consultant physiotherapists, the largest of all AHPs[10]. The distribution of consultant physiotherapists to this point is dominated by the musculoskeletal speciality with 29 consultants in this area registered in 2009[10]. Consultant physiotherapists are usually salaried equivalent to a grade 8a-d on approximately £35,232 to £73, 281 (2006 rates).
Training
Becoming a consultant physiotherapist is a career goal high on the list of many aspiring physiotherapist, graduates and current students. However this pathway requires utmost commitment. Vits[10] analysed that all registered physiotherapy consultants in 2009 had been educated at least to Master’s degree level, with many possessing doctorates. Back in 2002 following Dr Paul Watson’s appointment, he made his beliefs of the position known, suggesting that in order to use your skills as a consultant usefully, you must take a step back and look at what is important to the service through appraising existing information and proposing advancing service provision [11]. Watson defined the role as being more about strategic planning than administration, sussing out what is important for the area and challenge the existing evidence. However, the role of the consultant physiotherapist varies considerably between settings, depending largely on individual preference and methods of working. For instance, managerial roles can take presence over research and vice versa [11]. A major challenge facing these professionals is achieving a a balance between clinical practice and academic effort.
Following qualification as a physiotherapist and working in a specialist area, originating at The Wessex Deanery, Otterbourne, Hampshire, is a 3-6 year training programme for consultant practitioners. The course syllabus consists of clinical practice in addition to academic research, teaching and service development[12], thereby offering training across all four physiotherapy pillars at consultant level. Also included are independent prescribing and phlebotomy components leading to a Master’s, PhD or professional doctorate. Throughout the course, AHPs are also given the opportunity to attend conferences and shadow senior consultants, instigating great trust in other medical professionals [9] [10]).
Prior to application, applicants must exhibit clinical fineness and leadership potential, they must have a minimum of one year’s experience at the equivalent of Agenda for Change band 6 level. However, following training there is no guarantee of a consultant post becoming available to qualification holders meaning often returning to lower posts initially [10] [11].
Clews[11] describes managerial skills as often being developed on the job, learnt from various medical consultant colleagues. Consultant physiotherapists tend to spend part of their time in clinics however often find the bulk of the job lies within managing physiotherapy services. Future trainees are encouraged to get involved in national clinical networks and to consolidate their clinical knowledge in order to position themselves for such a position. As a consultant, physiotherapists should be confident in demonstrating a wide range of skills, be assertive and have good prioritisation skills [11] The effectiveness of the role
The effectiveness of consultant posts in clinical practice and patient care was studied by Guest et al. in 2004[13]. They explored leadership and how current consultants modify and craft the role in order to remain motivated and committed. It was found that consultant practitioners tend to adjust how they spend their time, with evidence of least time being spent in actual clinical practice. Reasons for these differences are likely to be because prior to taking up the consultant post, clinical practice had been their main priority. Most of the consultants analysed by Guest et al.[13] described their jobs as busy but satisfying and believed they were having a positive impact on patient care. Despite this, budgets inclusive of this post are being reduced across NHS boards and without succession planning; it is likely that the consultant post will disappear as the NHS evolves to accommodate changing patient needs[10].
Since 1948, the NHS workforce has erupted from approximately 144, 000 staff to a current 1.4 million in England alone with over 300 organisations [14] . By 2033 over one quarter of the population will be aged over sixty-five.
Demographically the health service will require future changes such as more first point of contact practitioners, increases in rehabilitation services, established prescribing abilities, and a higher need for surgical procedures and as a result, AHPs have recently been called upon to provide such services. Too often the range of knowledge, skills and competencies of AHPs is not fully and widely understood [1]. Educational opportunities and training programmes therefore must be integrally linked into current and emerging models for care in addition to scientific and technological advances to support allied Health Professionals (AHPs) who have the talenst and capacity to look beyond individual clinical practice. Such professionals re looking to maximise their contributions by getting involved in partnerships, leadership roles and scientific research [1] It is widely known that staff employed by the NHS intend to provide patient-centred care of the utmost quality. In 2008 the Department of Health’s NHS next stage review[1] intended to provide a vision for NHS staff to maintain this degree of excellence and outline a bottom-up approach to service provision. This report also summarised the proposition made by the NHS to ensure that students and recent new trainees, gain the depth and breadth of knowledge and experienced they need for adequate progression in clinical practice.
In most health organisations AHP career pathways are well established with junior practitioners progressing into clinical specialists, extended scope or advanced practitioners with a consultant role often being the pinnacle career goal. However, 2008 saw the launch of a UK-wide ‘Modernising Allied Health Professions Careers’ project, more recently known as [15]This web-based tool was constructed to target AHPs planning more flexible and alternative career pathways to ensure breath and depth of expertise and maximise future employment opportunities. This resource provides professionals with a framework of competencies and includes a web-based resource documenting AHP and support worker roles. The Chartered Society of Physiotherapy (CSP) furthered this by providing a physiotherapy specific online resource for members to keep their knowledge and skills updated. This includes a set of learning and development principles, the code of professional values and behaviour and a framework of physiotherapy knowledge and skills hoped to be of use to current practicioners. It has been suggested that by offering greater clarity of accountability, responsibility and primary roles at all levels, this will lead to enhanced future workforce planning and training commissioning, ensuring that the in the future, patients will have access to a paramount level of care for their needs.In support of the [2] to achieve a first class integrated workforce in the UK by 2020, this is hoped to aid planning and service redesign paying particular attention to leadership and the capacity and capability of AHPs. In addition to training, from a commissioner’s perspective these tools help to develop services by maximising the potential of AHPs to play a larger role in transforming care, having the competency to work across organisational boundaries . Academia, research and management job opportunities have shifted the focus from effective clinical practice to ensuring this practice is evidence-based and up-to-date and is able to respond efficiently and effectively to accommodate changing service requirements. According to [16] attracting and recruiting the right people into training programmes will benefit workforce planning for the future. Each year Health Education England (HEE) invests £4.8 billion of it’s £5 billion budget on education and training of this prospective workforce [16] to drive healthcare changes. However this said, 60% of this is spent on doctors making up 12% of the workforce while AHPs account for 40% of this population.
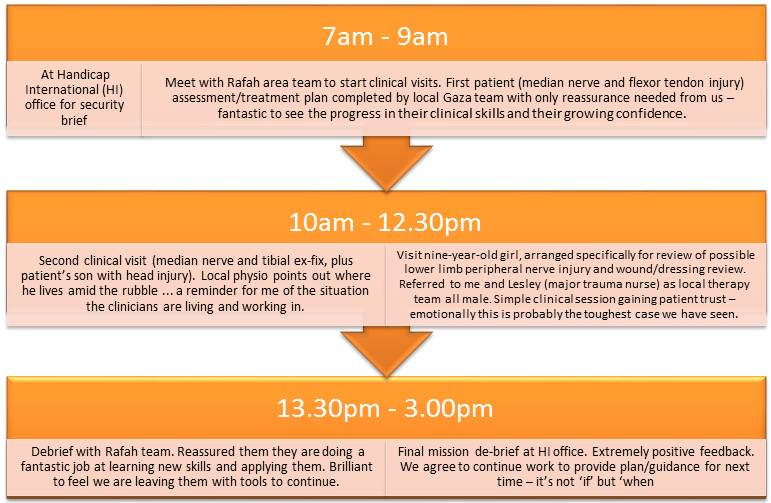
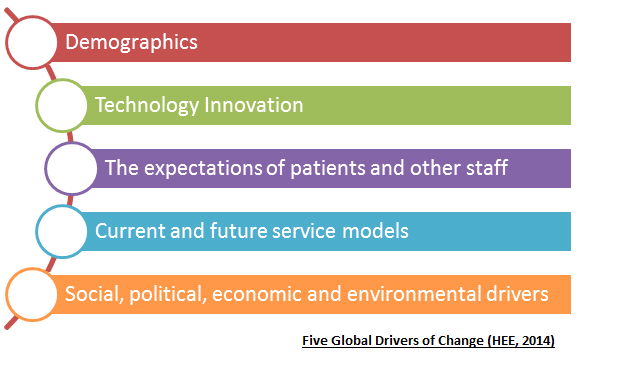
The Department of Health anticipate that in 10 years time, 60% of the current healthcare workforce will still be providing NHS services[1]. Thus supporting them through career frameworks will help to fulfil their individual potentials. In the [17] document there are five global drivers of change. These are demographics; technology innovation; social, political, economic and environmental drivers; current and future service models and finally the expectations of patients and other staff. Workforce planners will utilise these factors when balancing an expected demand with an efficient demand [1]. Primary care is defined as the first point of contact for someone seeking medical care, typically a general practitioner or a family doctor. Primary care acts to coordinate any other specialists that the patient may need [18]
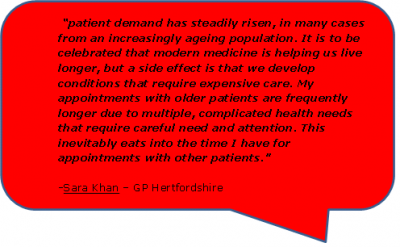
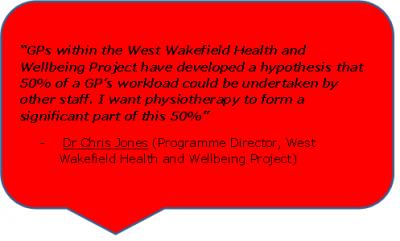
General Practitioners in the UK are suffering from an unstainable workload, which is negatively impacting appropriate appointment times with patients. Despite this, the government continues to push for GP surgeries to be open 7 days a week. If these plans go ahead, the strain placed on them will continue to grow. If drastic changes are not made to the way care is delivered, it is highly likely the NHS will reach breaking point.
What the role entails
What the role entails
Extended Scope Practitioner
What the role entails
Consultant Physiotherapist
What the role entails
Training and Career Pathways
Description
The quote on the right is taken from the CSP leaflet: physiotherapy works for primary care [19]. A link to the leaflet can be found