Definition/Description
Sacroiliitis is an inflammation of one or both sacroiliac joints, which can lead to inflammatory low back pain, although some patients remain asymptomatic. Sacroiliitis is linked to spondyloarthropathies (a group of diseases) and it can be defined as a sacroiliac joint dysfunction, which seems to be in a state of altered mechanics. Sacroiliitis is a hallmark of ankylosing spondylitis and may also be seen in the course of other rheumatic and non-rheumatic disorders, such as psoriatic arthropathy, familial Mediterranean fever, Bechet’s disease, hyperparathyroidism and others. Pain caused by sacroiliitis can be related to either too much or not enough motion in the SI joint. That makes it less a pathological diagnosis and more a patho-mechanical diagnosis.[1][2] [3](level 1A and 2 B)
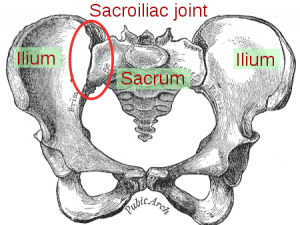
Clinically Relevant Anatomy
The sacroiliac joint (SIJ) forms the lowest segment of the spinal axis and distributes the forces coming from the upper body. Movements occurring in the sacroiliac joint play an important role in distributing forces and is influenced by the movement of the lumbosacral spine.[4] (level 1A)
The sacroiliac joint has been implicated as the primary source of pain in 10% to 27% of patients with mechanical low back pain below L5, utilizing controlled, comparative local anesthetic blocks.
The sacroiliac joint is a true diarthrodial joint, the articular surfaces are separated by a joint space containing synovial fluid and enveloped by a fibrous capsule. It has unique characteristics not typically found in other diarthrodial joints. The sacroiliac joint consists of fibrocartilage in addition to hyaline cartilage and is characterized by discontinuity of the posterior capsule, with ridges and depressions that minimize movement and enhance stability. The sacroiliac joint has been described as a synovial joint only in the anterior portion in contrast to the posterior portion. The posterior connection is a syndesmosis, consisting of the ligament sacroiliaca, the gluteus medius and minimus, and the piriformis muscles.
The sacraoiliac joint is well provided with nociceptor and proprioceptors. The innervation pattern is the subject of considerable discussions. The sacral plexus innervates the anterior portion whereas the spinal nerves innervate the posterior portion. It has been proposed that the predominant innervation is by L4 to S1 nerve roots with some contribution from the superior gluteal nerve.[5](level 1A) It has been variously described that the sacroiliac joint receives its innervation from the ventral rami of L4 and L5, the superior gluteal nerve, and the dorsal rami of L5, S1 and S2 or that it is almost exclusively derived from the sacral dorsal rami. (Level 1A) [6]
Epidemiology /Etiology
Spondyloartropathies: Ankylosing spondylitis, reactive arthritis, psoriatic arthritis, arthritis of chronic inflammatory bowel disease and undifferentiated spondyloarthropathy. Symmetrical sacroiliitis is found in more than 90% of ankylosing spondylitis and 2/3 in reactive arthritis and psoriatic arthritis. It is less severe and more likely to be unilateral and asymmetrical in reactive arthritis, psoriatic arthritis, arthritis of chronic inflammatory bowel disease and undifferentiated spondyloarthropathy. Also traumatic injuries, infections and inflammatory conditions like rheumatoid arthritis, degenerative joint diseases, metabolic conditions like gout and even pregnancy, sacroiliitis can cause sacroiliitis.[1][7] (level 1A and 1C)
The hospital prevalence of sacroiliac diseases is 0,55%, the female sex predominates( 82,35%) and the mean age of 25,58 years. Gyneco-obstetric events are the predominant risk factors (47,05%). The etiologie found are bacterial arthritis (82,3%) mainly pyogenic (70,58%), osteoarthritis(11,7%) and ankylosing spondylitis (5,9%) . (Level 2B)
Characteristics/Clinical Presentation
Patients report low back pain (below L5), pain in the buttocks and/or pelvis and postero-lateral on the thigh, which may extend down to one or both legs. The pain mostly occurs unilateral, inferior to the PSIS and above the knee with possible numbness, tingling and weakness. Pain may also radiate to the hip and groin region. Patients may report intolerance with lying or sitting and increasing pain while climbing stairs or hills. They experience poor sleep habits and unilateral giving way or buckling. Pain also occurs with position changes or transitional motions (i.e., sit to stand, supine to sit). [8]
Differential Diagnosis:
The diagnosis of acute sacroiliitis is often challenging because of both the relative rarity of this presentation and diverse character of acute sacroiliac pain, frequently mimicking other, more prevalent disorders
New-onset intense pain is a major clinical manifestation of acute sacroiliitis, pointing to the diagnosis. However, the character of acute SIJ pain may be variable in different individuals without a specific diagnostic pattern. Thus, the diagnosis of acute sacroiliitis is frequently overlooked at presentation. While the classic distribution of SIJ pain involves the ipsilateral buttock and paramidline lower lumbar area (in 94 and 72 %, respectively), its radiation to the groin (14 %), lower abdomen (2 %), upper lumbar area (6 %), and/or lower extremity (up to 50 %)—including thigh and trochanteric pain, lower leg pain, and even foot pain—may lead to confusion, suggesting alternative diagnoses, such as intervertebral disk disruption, hip joint disease, or even an abdominal event. [9] [10] (Level 1B)
The differential diagnosis of sacroiliitis on plain film[11]
– Ankylosing spondylitis
– Inflammatory bowel disease
– Hyperparathyroidism – tends to cause sacroiliac joint widening due to bone reabsorption
– Rheumatoid arthritis
– Gout
– Psoriatic arthropathy
– Reiter’s syndrome
– Osteoarthritis (OA)
– Infection – TB
There is even another way to differentiate sacroiliitis[12]
– Unilateral septic sacroiliitis
– Unilateral seronegative sacroiliitis
– Ewing’s sarcoma and lymphoma
Low grade radiographic sacroiliitis is a prognostic factor for ankylosing spondylitis in patients with undifferentiated spondyloarthritides (SpA).[13](level 2A)
Diagnostic Procedures
The diagnosis of sacroiliitis in clinical practice is based mainly on imaging techniques. It can be difficult to diagnose sacroiliitis in the early and acute stages because conventional radiographs may be normal, although other techniques, to be discussed, might detect sacroiliac inflammation. The radiographic images of the sacroiliac joint changes in advanced disease, sclerosis and may cause erosions. However, this might no longer be visible on the radiograph because of ankylosis.
Inflammatory back pain (IBP) can be a result of sacroiliitis. Because IBP is not a highly specific indicator of sacroiliitis, there is a need for valuable imaging techniques.
Techniques currently used to diagnose sacroiliitis:
– Radiography
– Scintigraphy
– Conventional tomography
– Computed tomography
– Magnetic resonance imaging
Scintigraphy lacks specificity. Computed tomography (CT) is a very good method to demonstrate already established bony changes and magnetic resonance imaging (MRI) has the ability to localize edema and differentiate degrees of inflammation. The MRI gives a good visualization of the complex anatomy of the sacroiliac joint. This testing can prove a possible spread to muscles as it occurs in septic sacroiliitis, an important differential diagnosis.[14](level 1A)
Devauchelle-Pensec et al compared computed tomography scanning and radiographs for the diagnosis of sacroiliitis. The conclusion of this study was that definite sacroiliitis was underestimated by radiography, as compared to CT scanning.[15](level 2B)
Blum et al determined the specificity and sensitivity for the diagnosis of active sacroiliitis, for each imaging method (plain radiography, scintigraphy, and contrast enhanced MRI). They used a reference standard, based on the clinical symptoms of inflammatory low back pain with or without laboratory signs, and clinical and radiographic findings. They performed a follow up during 1.5-2.5 years to confirm diagnosis. According to the results, MRI was most sensitive for the detection and confirmation of active sacroiliitis (95%) and superior to quantitative SI scintigraphy (48%) or conventional radiography (19%). MRI also had a higher specificity (100%) than scintigraphy (97%) or plain radiography (47%) for the assessment of inflammatory signs. There were persistent pathological signal intensities in the subchondral bone area despite clinically successful anti-inflammatory drug therapy, at repeat MRI testing after 2-30 months.[16](level 2B) ) It’s also possible to differentiate the diagnosis between infection and spondyloarthritis using the MRI features of bone lesions, soft-tissue lesions and joint space enhancement in unilateral sacroiliitis. Among various findings, periarticular muscle edema was the single most important predictor of infectious sacroiliitis. [17](Level 2B)
Sacroiliitis of seronegative spondyloarthropathy may sometimes show on pelvis plain films findings indistinguishable from those of osteitis condensans ilii. Computed tomography (CT) can differentiate earlier than plain radiography. There are criteria proposed by the European Spondlylarthropathy Study Group (EESG) that you can use to differentiate the two conditions. There is proof that the criteria are useful. It is right to differentiate clinically between the two diseases.
Outcome Measures
Outcome measures such as the Oswestry Disability Index (ODI) is most effective for persistent, severe disability, while the Roland-Morris is more appropriate for mild to moderate disability.[18](level 1A)
The Short-form McGill Pain Questionnaire (link) and The Assessment of Pain and Occupational Performance may also be appropriate.
Examination
Some individual pain provocation tests show sufficient inter-rater reliability. The following tests seem to have sufficient diagnostic accuracy:(Patrick-) FABER = Flexion, ABduction, External Rotation test , thigh thrust test*, Gaenslen test, Mennell’s test**, sacral thrust test***, compression test**** and distraction test. [2][7] [19] [20]
Combinations of these tests give a better accuracy to differentiate sacroiliitis from low back pain. We can use a combination of 3 tests (ex. Gaenslen, Mennell, and thigh thrust tests) or 5 tests (ex. Gaenslen, Patrick-Faber, Mennell, thigh thrust, and sacral thrust tests), which give favorable results respectively, if 2 or 4 tests are positive. A positive test means it provokes pain. [19] [21] [20]
A complete physical examination with an excellent accuracy to diagnose sacroiliac joint related pain should involve a cluster of sacroiliac joint tests and a McKenzie evaluation. [2] [7]
MRI and CT are also uses in the early stage to diagnose sacroiliitis. [19]
Thigh thrust test*:
Subject: Supine, contralateral leg extended
Examiner: Stands next to the subject
Technique: The examiner flexes the affected leg (contralateral), approximately hip at 90°, knees remain relaxed and graded force pressure is applied through the long axis of the femur (=posterior shearing stress), one hand underneath the sacrum, the other one around the knee to give pressure
Mennell’s test**:
Subject: Side-lying position, affected side is down, back towards the edge of the table. Affected (table contacting) side hip flexed to the abdomen, knee is flexed
Examiner: Stands behind the patient
Technique: Examiner puts one hand over the ipsilateral gluteal region and iliac crest, other hand grasps the semi flexed ipsilateral knee and lightly forces the leg to extension
Sacral thrust test***:
Subject: Prone, legs relaxed, semi abducted
Examiner: Stands behind the subject, close to the feet at the lower edge of the table
Technique: Puts hands over the sacrum applies anterior pressure to the sacrum
Compression test****:
Subject: Compression Side-lying position, affected side is up, close to the side of the table and back towards the edge of the table. Hips
flexed approximately 45°, knees are flexed approximately 90° degrees
Examiner: Stands behind the subject
Technique: Examiner’s Folded hands over the anterior edge of the iliac crest and applies downward pressure [19]
Distraction test:
The SIJ (Sacroiliac joint) Distraction (Colloquially know as Gapping) test is used to add evidence, positive or negative, to the hypotheses of an SIJ sprain or dysfunction when used in the Laslett SIJ Cluster testing. This test stresses the anterior sacroiliac ligaments This test has also been described as the Transverse Anterior Stress Test or the Sacroiliac Joint Stress Test.
1. The patient lies supine and the examiner applies a vertically orientated, posteriorly directed force to both the anterior superior ilac spines (ASIS) (Cook and Hegedus 2013, Laslett et al 2008, Laslett et al 2005, Laslett et al 2003).
Note: Cook and Hegedus (2013) suggest applying a sustained force for 30 seconds before applying a repeated vigorous force in an attempt to reproduced the patient’s symptoms. However, Laslett (2008) does not suggest any timings or changes in force.
Because of the lack of standardisation in the technique it is quite feasible different therapists will practise this test different ways, giving rise to variability in response and lowering the inter-tester reliability (Laslett et al 2005, Levin et al 2005). No evidence to suggest either method is preferable (Levin et al 2005), therefore, more evidence needed.
2. The presumed effect is a DISTRACTION of the anterior aspect of the sacroiliac joint. (Laslett et al 2005, Laslett et al 2003)
3. A test is positive if it reproduces the patient’s symptoms. This indicates SIJ dysfunction or a sprain of the anterior sacroiliac ligaments (Cook and Hegedus 2013, Cook et al 2007, Laslett 2008, Laslett et al 2005, Laslett et al 2003)
However, this test should be used in concordance within a SIJ testing cluster to ensure maximum reliability and validity when confirming hypotheses (Albert et al 2000, Kokmeyer et al 2002, Laslett 2008, Laslett et al 2005,Laslett et al 2003, Ozgocmen et al 2008, Robinson et al 2007). [22][23][24]
The sacroiliac joint can be examined by Special tests.
Medical Management
Reducing inflammation in the SI-joint and increasing the flexibility of the lumbosacral spine and SI areas are the main goals of treatment. NSAIDs (non-steroidal anti-inflammatory drugs) and anti-rheumatic drugs are the primary treatment for spondyloarthropathy. Global pain decreased significantly following treatment with naproxen (NSAID). Sulfasalazine is believed to reduce the erythrocyte sedimentation rate and morning stiffness. [25] Research revealed that a continuous treatment with NSAID’s reduces radiographic progression in symptomatic patients with AS. [26] (level 2A)
The patient must be referred to a physiotherapist. Suggest 3 to 4 days bed rest for severe acute cases. For persistent cases (2 to 4 weeks) with severe pain, a sacroiliac joint injection may be recommended to confirm the sacroiliac joint as the source of the pain and to introduce the anti-inflammatory medication directly into the joint. Advise 3 to 4 days of bed rest after the injection. Next it is recommended to continue with the restrictions and begin with flexion strengthening exercises after the pain and inflammation have been controlled. These exercises include side-bends, knee chest pulls and pelvic rocks.[27](level 1B)
Therapeutic solutions include intra-atricular injections with short-term pain relief and surgical fusion, which appears ineffective. Radiofrequency of the joint capsule or lateral branches has been previously reported with variable successes. The majority of patients with chronic SI joint pain experienced a clinically relevant degree of pain relief and improved function following cooled radiofrequency of sacral lateral branches and dorsal ramus of L5 at 3-4 months follow-up. [28]
If the condition persists (6 to 8 weeks) with no improvement of at least 50 percent, repeat corticosteroid injections. Subsequently begin strengthening exercises including sit-ups and weighted side bends. Start with general conditioning of the back and increase slowly to low-impact walking or swimming. Take up normal activities with proper care of the back.
Physical Therapy Management
Reducing inflammation in the SI-joint and increasing the flexibility of the lumbosacral spine and SI areas are the main goals of treatment. Give advice on proper lifting techniques involving the knees. The patient should also avoid movements such as tilting, twisting and extremes of bending. Maintaining correct posture is necessary, therefore a lumbar support for the office chair and vehicle is advised.[29](level 1A)
In the early treatment stages heat, cold or alternating cold with heat are effective in reducing pain.[30] (level 1A) Cryotherapy can be used to control the inflammation and pain. This form of treatment can be applied by ice massage or the application of ice packs. Cryotherapy should be applied for no more than 20 minutes, with at least one hour between applications. Ice massages will usually require a shorter treatment time. Thermotherapy can also be used by applying hot packs for a maximum of 20 minutes. This form of therapy is used to control pain, increase circulation and to increase soft tissue extensibility. With the aim of reducing pain, conventional TENS (Transcutaneous electrical nerve stimulation) can also be applied.[31][32][33](level 1B-1A- 1A)
In the early stage, we can also use a pelvic belt or girdle during exercise and activities of daily living. These SI belts provide compression and reduce SI mobility in hypermobile patients. The belt should be positioned posteriorly across the sacral base and anteriorly below the superior anterior iliac spines. This belt may also be used when this condition becomes chronic (10-12 weeks).[34][35][36](level 1B-1A-1A)
Once the acute symptoms are under control, the patient can start with flexibility exercises and specific stabilizing exercises. To maintain SI and lower back flexibility, stretching exercises are principal. These exercises include side-bends, knee chest pulls, and pelvic-rocks with the aim of stretching the paraspinal muscles, the gluteus muscles and the SI joint. After hyperacute symptoms have resolved these kinds of exercises should be started. Each stretch is performed in sets of 20. These exercises should never surpass the patient’s level of mild discomfort.[37](level 1A)
Specific pelvic stabilizing exercises, postural education and training muscles of the trunk and lower extremities, can be useful in patients with sacroiliac joint dysfunctions. The transversus abdominis, lumbar multifidi muscles and pelvic floor are the muscles that will need most training. Training of transversus abdominis independently of other abdominal muscles is effective to provide more stabilization of the sacroiliac joints and prevent laxity, which can cause low back pain. Therefore it is necessary to teach the patient how to contract the transversus abdominis and multifidus. During this learning process it is necessary to give the patient feedback. Also the specific co-contraction of the transversus abdominus and the multifidus should be included in the revalidation program. The best position to teach the patient to co-contract these muscles is in four point kneeling. When the patient can properly perform this exercise, it is time to increase the intensity by changing the starting position,…
Other examples of exercises may include: modified sit-ups, weighted side-bends and gentle extension exercises.
Strengthening of the pelvic floor muscles is also important because they oppose lateral movements of the coxal bones, which stabilizes the position of the sacrum. Activation of the transversus abdominis and pelvic floor muscles will reduce the vertical sacroiliac joint shear forces and increase the stability of the sacroiliac joint.
After rehabilitation, low-impact aerobic exercises such as light jogging and water aerobics are designated to prevent recurrence.[38][39][40][41][42](level 1B-2B-1A-1A-1A)
If the patient has a leg length discrepancy or an altered gait mechanism, the most reliable treatment would be to correct the underlying defect. Sacroiliitis is also a feature of spondyloarthropathies. In this case, this condition should also be treated.[43][44][45][46][47](level 1C-1A-1C-1A)
Key Research
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
add appropriate resources here
Clinical Bottom Line
add text here