Introduction
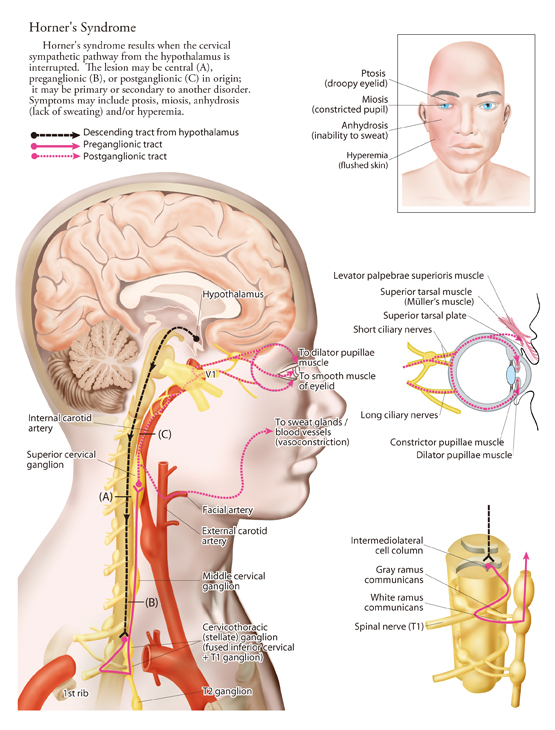
Horner’s syndrome results from an interruption of the sympathetic nerve supply to the eye and is characterized by the classical triad of miosis (ie, constricted pupil), partial ptosis, and loss of hemifacial sweating (ie, anhidrosis).
Other names of Horner’s syndrome are Bernard-Horner syndrome and Von Passow syndrome. [1]
Causes
Horner’s syndrome can be caused by any of the following:
- Lesion of the primary neuron
- Brainstem stroke or tumor or syrinx of the preganglionic neuron – In one study, 33% of patients with brainstem lesions demonstrated Horner syndrome [2]
- Trauma to the [3]
- Carotid artery ischemia
- Major Findings
Horner syndrome may develop from lesions at any point along the sympathetic pathway. Abnormalities found in all patients, regardless of the level of interruption, include the following:
- Mild-to-moderate ptosis, owing to denervation of the sympathetically controlled Müller muscle
- Slight elevation of the lower lid (upside-down ptosis), owing to denervation of the lower lid muscle (analogous to the denervation of the Müller muscle in the upper lid)
- Miosis and dilation lag, where pupillary dilation after psychosensory stimuli is slower in the affected pupil than in the unaffected pupil [4]
Additional Findings
Other findings that may be noted include the following:
- Partial ptosis
- Apparent enophthalmos – Assertions to the contrary notwithstanding, true enophthalmos does not occur; the ptosis merely gives an illusion created by narrowing of the palpebral fissure, which results from weakness of the muscle of Müller in both the upper lid (causing partial ptosis) and the lower lid (causing slight elevation of lower eyelid)
- Increased amplitude of accommodation
- Iris heterochromia (heterochromia iridis) – The affected iris may remain blue when the other iris changes to brown; this may be present if the lesion is in a child younger than 2 years but is uncommon in older patients; iris pigmentation is under sympathetic control during development, which is completed by the age of 2 years
- Paradoxical contralateral eyelid retraction
- Transient decrease in intraocular pressure and changes in tear viscosity
- Absence of a horizontal eyelid fold or crease in the ptotic eye, especially in patients with congenital Horner syndrome
- Red conjunctivae
Management
Appropriate treatment of Horner syndrome depends on the underlying cause. The goal of treatment is to eradicate the underlying disease process. In many cases, however, no effective treatment is known. Prompt recognition of the syndrome and expedient referral to appropriate specialists are vital.
Whether surgical care is indicated and what type is appropriate depend on the particular cause of Horner syndrome. Potential surgical interventions include neurosurgical care for aneurysm-related Horner syndrome and vascular surgical care for causative conditions such as carotid artery dissection or aneurysm.
Specialized Consultations
For optimal management of the underlying cause, the following specialist consultations may be required:
Pulmonology, Internal medicine, Neurology or neuro-ophthalmology
Interventional radiology (in cases of suspected carotid artery dissection)
Surgery or oncology (as warranted by the particular etiology)
Neurosurgery (in cases of suspected aneurysm)References
- ↑ von Passow A. Okulare Paresen im Symptomenbilde des “Status dysraphicus”, zugleich ein Beitrag zur Ätiologie der Sympathikusparese (Horner-Syndrom und Heterochromia iridis). Münchener Medizinische Wochenshrift. 1934;74:1243-9.
- ↑ Krasnianski M, Georgiadis D, Grehl H, Lindner A. [Correlation of clinical and magnetic resonance imaging findings in patients with brainstem infarction]. Fortschr Neurol Psychiatr. May 2001;69(5):236-41.
- ↑ Biousse V, Touboul PJ, D’Anglejan-Chatillon J, Lévy C, Schaison M, Bousser MG. Ophthalmologic manifestations of internal carotid artery dissection. Am J Ophthalmol. Oct 1998;126(4):565-77.
- ↑ Reede DL, Garcon E, Smoker WR, Kardon R. Horner’s syndrome: clinical and radiographic evaluation. Neuroimaging Clin N Am. May 2008;18(2):369-85,