Definition/Description
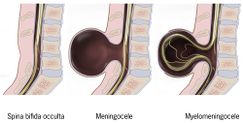
Spina Bifida in general is defined as “a neural tube defect (NTD) that results when the inferior neuropore does not close. Developing vertebrae do not close around an incomplete neural tube, resulting in a bony defect at the distal end of the tube.” [1]
Spina Bifida Occulta is described as a “benign closed NTD posterior vertebral defect only without a meningeal sac; location: lumbar-sacral spine; usually asymptomatic but can be associated with occult spina dyraphism; usually no associated defects.” [3]
Meningocele is described as a “closed NTD without extrusion of spinal cord elements into a meningeal sac; location: cervical, thoracic, lumbar, and/or sacral spine; motor deficits are less likely than with myelomeningocele; structural brain anomalies and Chiari II malformation are less likely.” [3]
Myelomeningocele is described as an “open NTD posterior vertebral defect and extrusion of spinal cord elements into a meningeal sac; location: cervical, thoracic, lumbar, and/or sacral spine, leads to paraplegia and insensitivity below the lesion and neurogenic bowel and bladder; associated defects include structural brain anamolies.[3]
Prevalence
In the United States, spina bifida occurs in less than 1 in 1,000 births. [3]
According to the CDC in 2002, there were approximately 24,860 children and adolescents living with spina bifida in the United States. [4]
The prevalence is higher among caucasion children than black children, however it is most common in hispanic populations. [4]
Characteristics/Clinical Presentation
Spina Bifida Occulta presents with:
- depression or dimple in the lower back
- a small patch of dark hair
- soft fatty deposits
- port-wine nevi (deep red-purple macular lesions). [5]
Spina Bifida Meningocele presents with:
- Saclike cyst that protrudes outside the spine [5]
Spina Bifida Occulta and Meningocele usually do not present with neurological deficits; however bowel and bladder incontinence may be present depending on the level of the lesion.
Spine Bifida Myelomeningocele produces more severe impairments:
- flaccid or spastic paralysis
- bladder incontinence
- musculoskeletal deformities (scoliosis, hip dysplasia, hip dislocation, club foot, hip/knee contracture)
- hydrocephalus, alone with Type I or II Arnold Chiari malformation
- trunk hypotonia
- delayed automatic postural reactions [5]
Associated Co-morbidities
Co-morbidities:
- Osteopenia or Osteopeorosis: due to the decreased level of activities of many of these individuals this will ultimately cause a decrease in bone density that will put them at risk for fractures [6]
- Obesity: due to decreased activity and sedentary lifestyle
Complications:
- Tethered Cord Syndrome: the spinal cord becomes fixated and begins to stretch which can cause further neurological deterioration [7]
- Urinary Tract Infection: often in individuals who have bowel and bladder incontinence will experience recurrent urinary tract infections [6]
- Decubitis Ulcer: these occur due to the altered sensation an individual may experience from the neurological defecit [6]
Medications
No specific medications are prescribed for the treatment of Spina Bifida. Depending on the location of the protruding sac, the individual may require the use of an assistive device to aid in walking- such as braces, walker, crutches, or a wheelchair. [8]
Diagnostic Tests/Lab Tests/Lab Values
Before Birth
- Alpha-fetoprotein blood test when 16-18 weeks pregnant [8] [9] [10]
- Amniocentesis may be done to further determine cause of increase in alpha-fetoprotein [7][9][10]
- Ultra-sound of the spine [8] [9]
After Birth
Etiology/Causes
Pathology:
- Neural groove develops to form the neural tube around day 20 after conception. In normal development the upper end is supposed to close at day 25 and the lower end is supposed to close at day 27. Three opportunities could cause abnormal closure of the neural tube. If the hyaluronic acid matrix or actin microfilaments have abnormalities early on, the neural tube will not close. If an overgrowth occurs over the caudal end the neural tube will not close, but this occurs later in development. The last chance for the tube not to close properly occurs when the glycoproteins that typically hold the cells together during closure fail to adhere the tube together. [5]
There is no exact reason known for the cause of Spina Bifida, but there are a variety of environmental and gentic factors that may be potential risk factors. [10][9]
Mother’s nutrition:
- Folic acid- less than 400 µg of folic acid per day [8][1] [11]
- Increase of: Vitamin A, valproic acid, solvents, lead herbicides, glycol ether, clomiphene, carbamazepine, aminopterin, alcohol [5]
Genetic:
- 3%-8% reoccurrence rate for parents who already conceived a child affecetd with spina bifida [5]
- Incidence rate increases 20x’s if the parents already have a child affected with a neural tube defect [11]
- In comparison to African-Americans, Caucasians more commonly have it, and Hispanics have a higher incidence rate than non-Hispanics [11]
Environmental Factors:
- Radiation and viruses may have an impact on developing fetus [9]
Systemic Involvement
Occulta and Meningocele: no neurological dysfunction typically present [5]
Myelomeningocele: permanent neurological and musculoskeletal deficits present [5]
- Neurological: muscle weakness, bowel and bladder problems, seizures, paralysis, absent reflexes, sensory impairments [5][6][8] [10]
- Musculoskeletal: hip dislocation, syringomyelgia, scoliosis, foot and ankle deformities [9]
Medical Management (current best evidence)
The management of spina bifida varies depending on the degree the individual is affected with the disease.
Spina Bifida Occulta:
- There is generally no medical treatment required
Spina Bifida Meningocele:
- Surgery is often performed early after birth, but severity of defecits after surgery depends on if there is neural tissue in the sac. Further treatment is similar to the management listed below for myelomeningocele. [8]
Spina Bifida Myelomeningocele:
- Generally surgery follows within the first few days of life to close the spinal cord defect. It is crucial during this time period prior to surgery to protect the nerves that are exposed in the protruding sac. It is also important to prevent infection and additional trauma to the exposed tissues. [7][8]
- Additional surgeries may be required to manage other problems in the feet, hips, or spine. The individuals with hydrocephalus will also require subsequent surgeries due to the shunt needing to be replaced. [7][8]
- The level of malformation of the spinal cord and subsequent neurological defects will influence the individual’s ability to ambulate. Assistive devices may be necessary to aid the individual around the community. [7]
- Due to the bowel and bladder problems that are often caused by the neural tube defect, a bowel and bladder program may be necessary. This may include catherterization or a strict bowel and bladder regimen to remain regular. [7]
- The MOMS study is a trial that was done to look at the effectiveness of having fetal surgery to fix the malformation of the fetus’s spine prior to birth in comparison to waiting until after the child is born to have the surgery. The idea behind it was that neurological function tends to decrease as pregnancy progresses, so by performing the surgery in utero the baby would not be exposed to such extensive neurological defecits as it would if the surgery was performed after birth. However, there is a safety concern for both the mother and the fetus when this fetal surgery is performed. The success of the MOMS trial has now made fetal surgery a treatment option in some cases. [12] [13]
Neurogenic bladder is a common complication for people with spina bifida. It is normally treated with pharmaceuticals and intermittent catheterization; however for some patients this treatment does not suffice. New research suggests the idea of tissue engineering and neuromodualation.
Tissue engineering is used to generate new tissue to augment the bladder. Two different theories are utilized: unseeded and seeded. Unseeded “involves the incorporation of a scaffold material (synthetic or biologic) into the host organ, which is used as a template for the ingrowth of native cells that then initiate the regenerative process.” Seeded technology is similar to unseeded; however it adds “cultured cells to the scaffold prior to implantation into the host.”
Neuromodulation modifies the innervation of the bladder so it can potentially function in a normal manner. Neuromodulation includes “non-operative measures such as transurethral electrical bladder stimulation, minimally invasive procedures such as implantation of a sacral neuromodulation pacemaker device, as well as operative measures that reconfigure sacral nerve root anatomy.”
Researchers are still in the early stages of development for this treatment option, however with advancements in technology is could prove to be a promising option for patients with spina bifida.
Physical Therapy Management (current best evidence)
Different factors can affect an individual with myelomeningocele’s ability to ambulate. The most prominent factor found between other socioeconomic and therapeutic factors was the location of the malformation. Individuals who had a higher lesion in the thoracic and upper lumbar spine were more likely to be in wheelchairs in comparison to those with lower lumbar and sacral malformations. Another important factor on an individual’s walking ability is the use of assistive devices, whether it is a brace, crutches or a walker. In order to promote walking capacity an assistive device may be necessary. [6]
In order to properly prescribe exercise training submaximal and maximal testing is necessary. Research has shown that treadmill speed and 6 minute walk distance are the best ways for detecting change. However, heart rate and VO2 peak measures are reliable ways to measure physiological output in ambulatory children with spina bifida especially when combined with functional outcomes such as the treadmill speed and 6 minute walk distance. [15]
There have been benefits shown in individuals with spina bifida that can be attributed to walking such as urinary drainage, bowel function, and peripheral circulation. The use of different assistive devices have been prescribed to individuals with spina bifida. A long term study was done on individuals that were given a ORLAU Parawalker (a Reciprocal Walking Orthosis). Based on past studies the use of these orthosises were higher than other aides, such as conventional KAFOs, that have been studied in the past. This study suggests that ORLAU Parawalker for children may increase their ability to ambulate which can ultimately provide other benefits that were mentioned earlier. [16]
Differential Diagnosis
- Spine segmental dysgenesis: A sporadic disorder characterised by congenital acute-angle kyphosis or kyphoscoliosis that is localised to a spinal segment, usually in the thoracolumbar or upper lumbar spine. [17]
- Caudal regression syndrome (sacral agenesis): A rare disorder associated with maternal diabetes that affects the sacral or lumbosacral spine. [17]
- Multiple Vertebral Segmentation Disorder: Autosomal recessive disorder characterised by short trunk dwarfism, multiple segmentation anomalies of the vertebral column, and costal anomalies.
- VACTERL (vertebral abnormalities, anal atresia, cardiac abnormalities, tracheo-oesophageal fistula and/or oesophageal atresia, renal agenesis, and dysplasia and limb defects): A non-random association of multiple mid-line congenital anomalies including vertebral, anal, and cardiac defects; tracheo-oesophageal fistula; renal anomalies; and limb anomalies. [17]
Case Reports/ Case Studies
Behavioral Treatment of Ambulatory Function in a Child with Myelomeningocele: A Case Report [view in Resources
see adding references tutorial.
References
Ola!
Como podemos ajudar?