Definition/Description
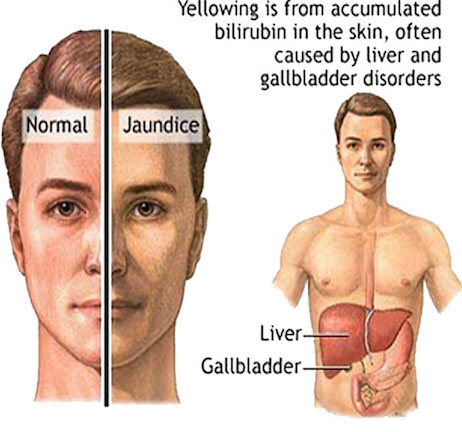
Gilbert’s syndrome is a benign liver condition that is characterized by elevated levels of bilirubin in the blood[1][2]. Bilirubin is produced by the breakdown of red blood cells and is able to be removed from the body after the liver converts it from unconjugated bilirubin to conjugated bilirubin[1][3][4]. In individuals with Gilbert’s syndrome, there is a buildup of unconjugated bilirubin in the liver as a result of a genetic mutation of the enzyme UDP-glucuronosyltransferase 1A isoform 1 (UGT1A1), which is important in bilirubin metabolism[4][5]. The buildup of bilirubin is particularly evident after starvation, exertion, infection, consumption of alcohol, or dehydration[5]. Bilirubin levels fluctuate and rarely increase to levels that cause jaundice[1].
Prevalence
Estimated to affect 3 to 7% of individuals of all races[3][4].
More common among males (2:1) compared to females (7:1)[2][3].
Characteristics/Clinical Presentation
Symptoms of Gilbert’s syndrome may include mild jaundice of the skin and eyes and is more commonly seen when the body is under stress [1]. 30% of individuals will never have any signs or symptoms[1]. In the study published by Radoi et al[4], 74% of the participants presented with recurrent asymptomatic jaundice, 66% nausea, 65% asthenia, 52% vague abdominal distention, and 8% were asymptomatic.
Associated Co-morbidities
There are no associated co-morbidities for individuals with Gilbert’s syndrome.
Medications
No medication is required for Gilbert’s syndrome. Some medications, such as the cancer therapy drug Irinotecan, may cause diarrhea for individuals with Gilbert’s syndrome. Other drugs such as Gemfibrozil, Atazanavir and indinavir may increase risks of jaundice and should also be avoided in patients with Gilbert’s Syndrome[6]
Diagnostic Tests/Lab Tests/Lab Values
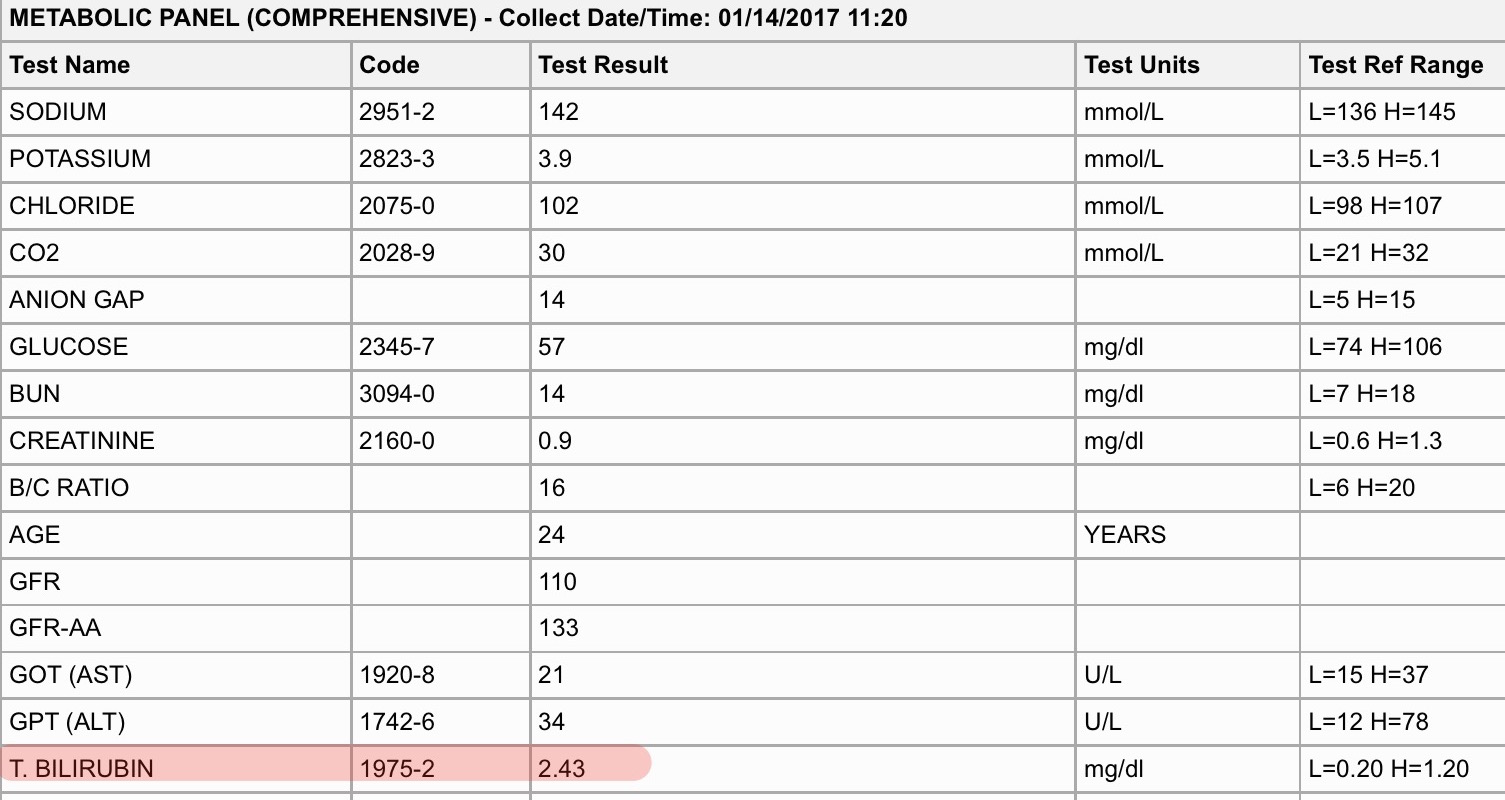
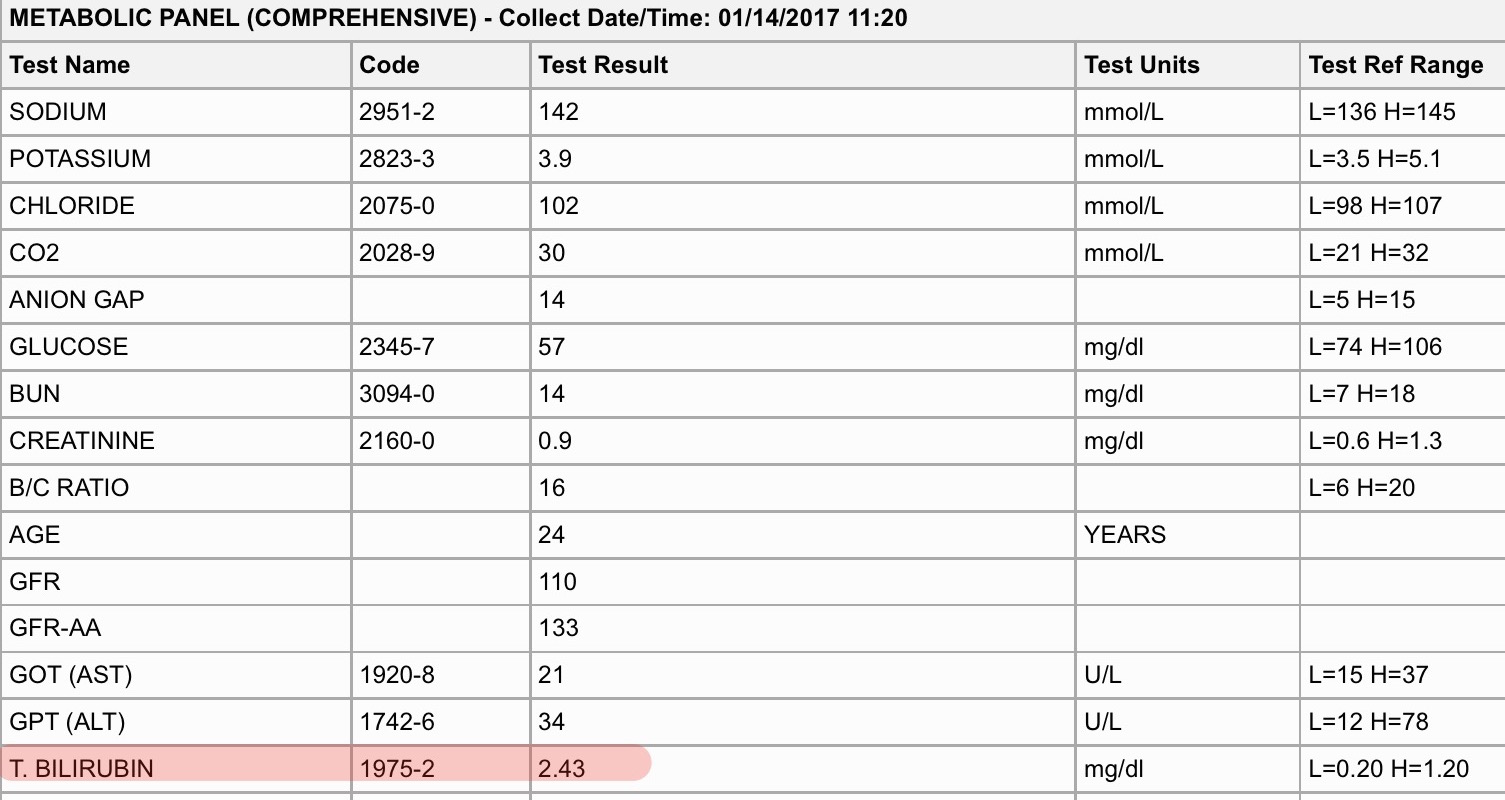
Diagnosing Gilbert’s syndrome can be done by a blood test that detects elevated bilirubin levels. Most often the total level of bilirubin is less than 2 mg/dL, and the conjugated bilrubin level is normal[7]. A complete blood count (CBC) and a liver function test may also be performed to rule out other diseases than can cause elevated bilirubin. The combination of normal blood and liver function tests and elevated bilirubin levels is an indicator of Gilbert’s syndrome[8]. Genetic testing is not needed[1]. Gilbert’s syndrome is generally present at birth but goes unnoticed until the late teens or early twenties[4].
Etiology/Causes
- Inherited gene abnormality of the UGT1A1 gene which is expressed on the 2q37 chromosome[4][8]
- Inherited autosomal recessive gene mutation, both parents must have the gene in order for it to be present[3][8]
- Occurs in the absence of liver disease or hemolysis[4]
- Liver does not properly dispose of bilirubin due to the mutation of UGT1A1[4]
- Usually goes unnoticed until after puberty[8]
- Elevated bilirubin and jaundice can come after dieting, starvation, consumption of alcohol, dehydration, increases in stress, intense physical exercise, infection or a lack of sleep[3][5][6]
Systemic Involvement
Individuals with Gilbert’s Syndrome were found to have reduced risk for endothelial dysfunction. Elevated bilirubin levels were found to reduce the prevalence of vascular complications and atherosclerosis in individuals with Gilbert’s Syndrome. This occurs by reducing the development of atherosclerosis by inhibiting the molecule responsible for intracellular adhesion. Dysfunction of the coronary microvasculature is also reduced due to the elevated levels of serum bilirubin[2].
Medical Management (Current Best Evidence)
Gilbert’s syndrome does not require any treatment. Mild jaundice may occur but does not require medical intervention. Jaundice caused from Gilbert’s Syndrome can be managed with rest, a healthy diet, and adequate fluids[6]. Gilbert’s syndrome is considered a mild condition and life expectancy is not affected[3].
Physical Therapy Management (Current Best Evidence)
No physical therapy management is required.
Differential Diagnosis
The following are conditions that could present similiar to Gilbert’s syndrome[9].
- Acute and chronic liver disease
- Crigler-Najaf syndrome
- Medication-induced hyperbilirubinemia
- Rhabdomyolysis
- Biliary tract disease
- Hemolysis
- Thyrotoxicosis
Case Reports/ Case Studies
[10]
Authors: Mohan M, Sailaja LP, Narasimha PV
Journal: Journal of Clinical & Diagnostic Research
Date, Volume, Pages: 2014Jun;8(6):1-2
History
Patient was a female who presented to the emergency room with severe vomiting, myalgia, headache and jaundice. Patient was 32 weeks pregnant upon arrival to the ER. Jaundice had been present for 3 days. Patient had similar complaints at 16 and 24 weeks of gestation. She had no similar signs or symptoms prior to her pregnancy. Treatment included IV fluids and the issues resolved.
Examination
Pt was conscious, dehydrated, and had icterus without pallor
BP – 90/60 mmHg
Fetal HR – 148/mt
Urine ketone bodies 4+
RBS 54 mg/dL
Liver Function test normal with exception of serum bilirubin – 6mg/dL
Hepatitis test – negative
Liver – normal with no signs of obstruction
Treatment
Treated with IV fluids to correct dehydration
Jaundice resolved spontaneously
Serum bilirubin decreased to 2mg/dL within 48 hours
Symptoms improved and patient was discharged
Results
Patient was diagnosed with Gilbert’s Syndrome. The diagnosis was made due to constitutional symptoms present, hypoglycemia, and jaundice which was determined to be aggravated due to dehydration. The baby was born at 38 weeks following emergency Caesarian section. Both baby and mother were healthy at birth, five days and six weeks postnatal and showed no further signs of jaundice or elevated bilirubin levels.
Resources NIH/National Institute of Diabetes, Digestive and Kidney Diseases Extension:RSS — Error: Not a valid URL: addfeedhere
Phone: (301) 496-3583
Website: Recent Related Research (from
References
- ↑ 1.01.11.21.31.41.5 Genetics Home Reference. Gilbert syndrome [Internet]. Genetics Home Reference. 2017 [cited 5 April 2017]. Available from: ↑ 2.02.12.2 Sertoğlu E, Tapan S, Doğru T, Acar R, Doğan T, Ince S, et al. Gilbert’s syndrome: protective effect on endothelial dysfunction. Turkish Journal of Biochemistry. 2016Dec;41(6):451-8.
- ↑ 3.03.13.23.33.43.5 Gilbert Syndrome – NORD (National Organization for Rare Disorders) [Internet]. NORD (National Organization for Rare Disorders). 2017 [cited 2017 April 5]. Available from: ↑ 4.04.14.24.34.44.54.64.7 Radoi VE, Ursu RI, Poenaru E, Arsene C, Bohiltea CL, Bohiltea R. Frequency of the UGT1A1*28 polymorphism in a Romanian cohort of Gilbert syndrome individuals. Journal of Gastrointestinal and Liver Diseases. 2017Mar;26(1):25–8.
- ↑ 5.05.15.2 Melissa Conrad Stöppler, MD. Gilbert Syndrome: Symptoms, Diagnosis, Treatment & Alcohol [Internet]. MedicineNet. 2017 [cited 5 April 2017]. Available from: ↑ 6.06.16.2 Dr Ananya Mandal M. Gilbert’s Syndrome Treatment [Internet]. News-Medical.net. 2017 [updated 2014 January 8; cited 2017 April 5]. Available from: ↑ Gilbert disease: MedlinePlus Medical Encyclopedia [Internet]. Medlineplus.gov. 2017 [updated 2017 March 9; cited 2017 April 5]. Available from: ↑ 8.08.18.28.3 Mayo Clinic Staff. Gilbert’s syndrome – Mayo Clinic [Internet]. Mayo Clinic. 2017 [cited 5 April 2017]. Available from: ↑ Olivera-Martinez, MA. Gilbert Syndrome [Internet]. epocrates. 2016. [updated 6 April 2016; cited 5 April 2017]. Available from: ↑ Mohan M, Sailaja LP, Narasimha PV. Pregnancy with Gilbert Syndrome – A Case Report. Journal of Clinical & Diagnostic Research. 2014Jun;8(6):1-2