Purpose
The Numeric Pain Rating Scale (NPRS) is a unidimensional measure of pain intensity in adults,[1][2][3] including those with chronic pain due to rheumatic diseases.[3][4]
Content
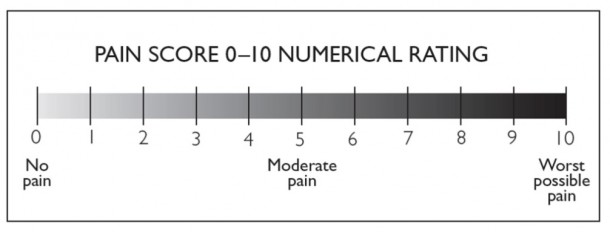
The NPRS is a segmented numeric version of the visual analog scale (VAS) in which a respondent selects a whole number (0–10 integers) that best reflects the intensity of his/her pain.[3] The common format is a horizontal bar or line. Similar to the VAS, the NPRS is anchored by terms describing pain severity extremes.[5]
Number of Items
Although various iterations exist, the most commonly used is the 11-item NPRS.[6]
Response Options/Scale
The 11-point numeric scale ranges from ‘0’ representing one pain extreme (e.g. “no pain”) to ’10’ representing the other pain extreme (e.g. “pain as bad as you can imagine” or “worst pain imaginable”).[2][3]
Recall Period for Items
Recal varies, but respondents are most commonly asked to report pain intensity “in the last 24 hours” or an average pain intensity.[7]
Obtaining the Scale
Available from Administration
The NPRS can be administered verbally (therefore also by telephone) or graphically for self-completion.[4] As mentioned above, the respondent is asked to indicate the numeric value on the segmented scale that best describes their pain intensity.[5] Scores range from 0-10 points, with higher scores indicating greater pain intensity.[5] To improve discrimination for detecting relatively small changes, an NPRS comprised of numbers along a scale was used in a population of 100 patients with a variety of rheumatic diseases. Variations in pain descriptors used as anchors for end points on the NPRS have been reported in the literature. However, the methodology used to develop these various anchor terms is unknown.[10][11] Chronic pain patients prefer the NPRS over other measures of pain intensity, including the VAS, due to comprehensibility and ease of completion.[12] However, focus groups of patients with chronic back pain and symptomatic hip and knee osteoarthritis (OA) have found that the NPRS is inadequate in capturing the complexity and idiosyncratic nature of the pain experience or improvements due to symptom fluctuations.[13][14] High test–retest reliability has been observed in both literate and illiterate patients with rheumatoid arthritis (r = 0.96 and 0.95, respectively) before and after medical consultation.[4] For construct validity, the NPRS was shown to be highly correlated with the VAS in patients with rheumatic and other chronic pain conditions (pain>6 months): correlations range from 0.86 to 0.95.[4] In clinical trials of pregabalin (also known as Lyrica) for diabetic neuropathy, postherpetic neuralgia, chronic low back pain, fibromyalgia, and OA, analyses of the relationships between changes in NPRS scores and patient reports of overall improvement (measured using a standard 7-point patient Global Impression of Change), demonstrated a reduction of 2 points, or 30%, on the NPRS scores to be clinically important.[15] Similar results were found in low back pain patients when changes in NPRS scores were compared to patient improvements in pain after physical therapy using a 15-point Global Rating of Change scale.[16] In another study, the MCID was found to be 2 points in patients with shoulder pain.[17]Scoring and Interpretation
Merits and Demerits
Psychometric Information
Development
Acceptability
Reliability
Validity
Minimal Clinically Important Difference (MCID)
References