Definition/Description
Is the presence of a radiological finding of calcification on the medial side of the knee as a consequence of trauma, plus clinical symptomatology of pain and diminished range of motion.[1] This calcium deposit develops between the attachment of the medial collateral ligament and medial condyle.[2][3][4]
The radiographic finding of the lesion is termed Pellegrini–Stieda phenomenon/lesion/sign, whereas the combination of the radiographic anomaly at the designated location with pain at that site is known as Pellegrini–Stieda syndrome.
PS lesion might not entail one entity but represent a spectrum of traumatic lesions resulting in an ossification on the medial side of the distal femur.[5] The origin of calcification remains under debate but proposed origins are[6]:
- deep medial/tibial collateral ligament
- superficial medial/tibial collateral ligament
- medial patellofemoral ligament
- medial gastrocnemius
- adductor magnus
- vastus medialis.
Although the MCL was most often coined as the origin of the lesion (54% overall, 25% on MRI, and 57% during surgery), many cases remained undecided (50% on MRI) or no specific structure was found to be the origin (29% during surgery).[6]
Clinically Relevant Anatomy
The medial/tibial collateral ligament (MCL) is a broad, flat band that extends from the medial femoral epicondyle to the medial meniscus, tibial plateau, and adjacent shaft. It consists of superficial and deep components. The superficial component attaches distally to the medial aspect of the tibia and proximally to the medial femoral epicondyle. The deeper component originates from the medial joint capsule and attaches to the medial meniscus.
The superficial component is about 10 cm long and flat. The bursae separate the capsule and the medial meniscus of the superficial component. It may be one or more bursae. The superficial component of the medial collateral ligament crosses, in his way down to the medial site and posterior medial surface of the tibial, the tendons of the sartorius, gracilis and, semitendinosus, also separated by a bursa. Below the ligament runs the medial inferior geniculi vessels and nerve and the anterior section of the semimembranosus tendon. The deeper component is shorter than the superficial and descends posteriorly to the medial tibial plateau, proximal to the groove for the semimembranosus.
The medial collateral ligament is an important ligament, it has an important role in stabilizing the knee joint. The long fibers of the MCL primarily stabilize the medial side of the knee against valgus and external rotatory stress. The deeper part of this ligament also helps the anterior cruciate ligament in avoiding an anterior translation of the tibia on the femur.[7][8][9]
Epidemiology /Etiology
The Pellegrini-Stieda syndrome is a relatively infrequent phenomenon and is commonly associated with sporting injuries.[5, 6] PSS Is more frequently in the male gender between 25 and 40 years of age.[1]
Direct trauma or in a distant site (skull or spine), repetitive trauma, or after an overstretching injury to the medial collateral ligament and joint capsule can result in an avulsion of the medial femoral condyle or a tear of ligaments, tendons. This injury develop a hematoma or inflammatory edema of soft tissue as a result of tearing and shredding fibers at their femoral attachment [2][10]. The soft tissues degenerate and become affected and subsequent deposition of hydroxyapatite or calcium pyrophosphate produces the calcification in the month following the trauma[1]
Ossification could happen within 11 days to 6 weeks after post trauma. A network of the new bone formation around the periphery of the mass of the medial condyle is formed in 6 to 8 weeks. Duration of the condition is usually about 5 to 6 months.
After a while, the phenomena could occur: the inflammation subsides with partial or complete resorption of the calcium salts, or the mass becomes ossified and may be connected by a pedicle to the femoral condyle. The last is called Pellegrini-Stieda syndrome. [10][11]
Characteristics/Clinical Presentation
Pain and local swelling in the medial aspect of the knee are the two first symptoms following an injury like traumatic synovitis. The pain and disability will increase after a few weeks or months.[1]
The knee will be stiff with the limitation of flexion–extension movements of the joint. The stiffness in the knee will mainly hamper the stretching of the knee but also twisting of the knee will be rather difficult. In addition to the limitation of motion, it is possible that a tender lump can be seen on the inside of the knee.[1][12]
The majority of patients are asymptomatic.[1]
Prognosis
When a full range of motion in the knee is attained, and the athlete does not feel any form of pain, he can resume his activities. It is also important that the range of motion is symmetric on both sides. Also, the muscles, Quadriceps, and Hamstrings, have fully recovered. This means full power recovery.[4]
Diagnostic Procedures
The combination of Pellegrini–Stieda phenomenon/lesion/sign, plus localized pain on medial side of the knee and diminished range of motion is enough to diagnose this Syndrome.[1]
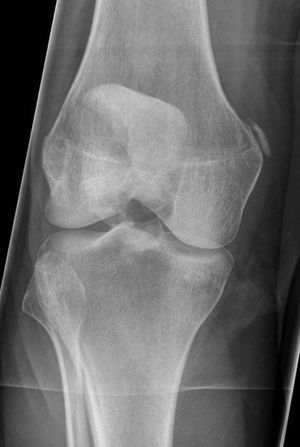
Secondary to the mechanism of injury swelling or hematoma may displace the injured ligament or tendon and subsequently the calcification that can be viewed on conventional X-ray.[5] It can be observed a linear or curved calcification from the origin the medial collateral ligament and that may extend almost to the insertion. A new classification is proposed based on the location[2][13]:
- I: beak-shaped with inferior orientation and union to the femur: the ossification arises from the femur and extends inferiorly in the TCL
- II: drop-shaped with inferior orientation and parallel to the femur: located in the TCL, without attachment to the femur.
- III: elongated with superior orientation: ossification lying in the distal adductor magnus tendon
- IV: beak-like with superior orientation and inferior attached to the femur: ossification attached to the femur, extending into both the TCL and the adductor magnus tendon
MRI seems to be a noninvasive and more accurate imaging[5] than conventional X-ray[5][6]
Examination
The patient complains about a severe, recurrent pain in the inner aspect of the knee.[12] Most of the patients sustained an injury years, months or weeks earlier.[2][12]The gait of the patient is normal with mild tenderness over the medial border of the knee.[12]In most of the cases, on examination, no swelling can be observed.[2]The patient has some difficulty with full passive extension or twisting of the knee. There is no ligamentous laxity.[2][12]
Medical Management
The treatment of the PSS is usually conservative.[1][2]
The use of Aspirin or non-steroidal anti-inflammatory preparations could be prescribed in the treatment of this condition. And if pain persists is infiltration of a corticosteroid agent to the tender medial collateral ligament attachment useful. [3][14]
If severe movement restriction because of damage of the medial collateral ligament, surgical excision of the calcification and ligament repair have been performed with good outcomes.[1][15] The pain is gone and the knee again has his full range of motion. Their removal in the early stages of the disease is not recommended because of the high risk of relapse.[1]
Measures such as rest, physical therapy, steroids, and lidocaine injections have been successfully used.[1]
Physical Therapy Management
First conservative work, with emphasis on avoiding overload and microtrauma, therefore forced rehabilitation or early sports resumption is to be avoided.
Ice therapy is useful, as well as local and general antiinflammatory.[16](level of evidence 5) Even conservative rehabilitation and mobilization of the knee joint are necessary.
The different steps of the functional rehabilitation can be completed, only in a more controlled and slow manner.[16]
Some examples of knee bending exercises are:
- heel slides
- seated knee bending
- seated chair slides
- knee bending on the stomach.
To increase the stretch is useful to use a strap around the ankle and pull or pulling with contralateral leg. Knee straightening exercises could be performed in lying or sitting position with a towel roll under the ankle so that the calf clears the table and increase of the stretch can be done. Another option could be knee straightening on stomach, putting the towel roll under the thigh and the feet off the edge of the table[16][12][14][17][18]
References
- ↑ 1.001.011.021.031.041.051.061.071.081.091.10 Restrepo, J. P., & del Pilar Molina, M. ↑ 2.02.12.22.32.42.52.6 Brukner P. and Khan K. Clinical Sports Medicine. Sydney: McGraw-Hill Australia. 2006
- ↑ 3.03.1 Kogon, P. L., Tchoryk, J., & Fleming, O. ↑ 4.04.1 Shanker, V. S., Gadikoppula, S., & Loeffler, M. D. ↑ 5.05.15.25.3 Somford, M. P., Janssen, R. P. A., Meijer, D., Roeling, T. A. P., Brown Jr, C., & Eygendaal, D. The Pellegrini–Stieda Lesion of the Knee: An Anatomical and Radiological Review. The journal of knee surgery. 2018
- ↑ 6.06.16.2 Somford, M. P., Lorusso, L., Porro, A., Van Loon, C., & Eygendaal, D. The Pellegrini–Stieda Lesion Dissected Historically. The journal of knee surgery.2018; 31(06): 562-567.
- ↑ Agranoff A. Medial collateral and lateral collateral ligament injury. Abailable from:↑ Knee guru. Anatomy of the collateral ligaments. Available from: ↑ Schunke M. Schulte E. Schumacher U. Rude J. Voll M. Prometheus: Anatomische Atlas. Houten: Bohn Stafleu van Loghum, 2010
- ↑ 10.010.1 Turner, J. W., Syed, I. B., & Spencer, R. P. ↑ Challans A. Pellegrini-Stieda disease. Available from: ↑ 12.012.112.212.312.412.5 Akinkunmi, S Vijayvargiya, C Prakash, M Kayode, G Awosanya. ↑ Ridley, L. J., Han, J., Ridley, W. E., & Xiang, H. B↑ 14.014.1 Altschuler, E. L., & Bryce, T. N. ↑ Theivendran, K., Lever, C. J., & Hart, W. J. Good result after surgical treatment of Pellegrini–Stieda syndrome. Knee Surgery, Sports Traumatology, Arthroscopy. 2009; 17(10):1231-1233. Level of evidence: 3b
- ↑ 16.016.116.2 Prof. Dr. R. Meeusen , Vrije universiteit brussel, cursus 488, (2011).
- ↑ Kaiser Permanente. Tips and exercises for your knee stiffness and pain. Available from: ↑ Lephart, S. M., & Henry, T. J. Functional rehabilitation for the upper and lower extremity. The Orthopedic Clinics of North America.1995; 26(3): 579-592.