Introduction
Scapulohumeral rhythm (also referred to as glenohumeral rhythm) is the kinematic interaction between the scapula and the humerus, first published by Codman in the 1930s. [1]
This interaction is important for the optimal function of the shoulder. [2] When there is a change of the normal position of the scapula in relation to the humerus, this can cause a disfunction of the scapulohumeral rhythm. The change of the normal position is also called scapular dyskinesia. Various studies of the mechanism of the shoulder joint have attempted to describe the global motion capacity of the shoulder refer to that description, can you evaluate the shoulder to see if the function is correct? and explain the complex interactions between components involved in placing the hand in space.[3]
Clinical Relevant Anatomy
Shoulder movements
The interplay of 4 articulations (Sternoclavicular Joint, Acromioclavicular Joint, Scapulothoracic Joint and Glenohumeral Joint) of the shoulder complex, results in an coordinated movement pattern of the arm elevation. The involved movements at each joint are continuous, although occurring at various rates and at different phases of arm elevation. The movement of the scapula can be described by rotations in relation to the thorax. The scapula moves around a dorso-ventral axis, resulting in a rotation in the frontal plane. In this movement the glenoid cavity is turned cranially (upward rotation) or caudally (downward rotation). In the sagittal plane, around a latero-lateral axis the scapula rotates posteriorly (posterior tilting) or anteriorly (anterior tilting). External and internal rotation occurs around a cephalo-caudal (longitudinal) axis. The external rotation brings the glenoid cavity more into the frontal plane, whereas the internal rotation turns the glenoid cavity more to the sagittal plane. [4]
When we perform flexion, the glenohumeral (GH) joint contributes 100°-120°. The scapula on the thorax contributes to elevation (flexion and abduction) of the humerus by upwardly rotating the glenoid fossa 50° to 60° from its resting position.[1] If the humerus were fixed to the fossa, this alone would result in up to 60° of elevation of the humerus. The humerus, of course, is not fixed but can move independently on the glenoid fossa.
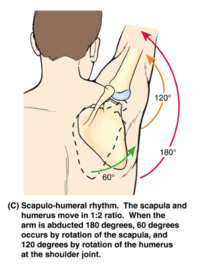
Inman et al. reported an inconsistent amount and type of scapular motion in relation to GH-motion during the initial 60°. [5] In this early phase (0-60°), motion occurs primarily at the GH joint, although stressing the arm may increase the scapular contribution. [6] During abduction of the humerus in the plane of the scapula, an average of 43° of lateral rotation from the resting position has been reported, with peak lateral rotation generally occurring between 90° and 120° of humeral elevation. It must also be recognized, however, that elevation of the arm is often accompanied not only by elevation of the humerus but also by lateral rotation of the humerus in relation to the scapula. [7]
When we perform abduction, the GH-joint contributes 90-120°. The combination of scapular and humeral movement result in a maximum range of elevation of 150-180°. [8][9] Also by abduction Inman et al. reported an inconsistent amount and type of scapular motion in relation to GH-motion this time during the initial 30°. [5] In this early phase, motion occurs primarily at the GH joint, although stressing the arm may increase the scapular contribution. [6]
Scapulohumeral Ratio
Scapulohumeral rhythm or ratio is significantly greater (less scapular motion and more humeral motion) in the sagittal plane than other planes. Consistent with the findings, the dominant side demonstrated significantly higher values for SH rhythm than the non-dominant side but only in the coronal and scapular planes but not in the sagittal plane. [9] By healthy male is a significant difference by hand dominance only in scapular upward rotation during scapular plane arm elevation.[7]
The scapulohumeral rhythm is therefore defined as the ratio of the glenohumeral movement to the scapulothoracic movement during arm elevation. This is most often calculated by dividing the total amount of shoulder elevation (humerothoracic) by the scapular upward rotation (scapulothoracic). [4]
In the literature Scapulohumeral rhythm is descibed like a ratio: humeral elevation:scapulothoracal rotation. The overall ratio of 2:1 during arm elevation is commonly used. According to the 2-to-1 ratio frame-work, flexion or abduction of 90° in relation to the thorax would be accomplished through approximately 60° of GH and 30° of ST motion. In another study of Scapulohumeral rhythm between children and adults, the mean ratio for the scapular plane was 2.4:1 for adults, 1.3:1 for children. [5]
If we compare the scapulohumeral rhythm by children with adults, we see that children showed a higher scapulohumeral rhythm during lowering of the arm than adults. [1] Also during scapular plane rotation from 25° to 125°, children showed greater upward rotation than adults. [5]
Ratios are often described as nonlinear indicating changing ratios during ROM. The 2 to 1 ratio substantially varies in scapular and humeral contributions at different points in the ROM and among individuals.
Epidemiology / Etiology
It has been reported that scapular dyskinesis occurs in 68 – 100 % of patients with shoulder injuries (including glenohumeral instability, rotator cuff abnormalities, and labral tears. [8] Other studies showed that scapular upward rotation is significantly increased in patients with full-thickness rotator cuff tears compared with controls in both sagittal and scapular plane elevation. Also, an increased scapular component is generally thought to contribute to the scapulohumeral rhythm ratio in frozen or stiff shoulders. [9]
Given the role of the scapula in shoulder function, the ability to monitor the coordinated motion of the scapula and humerus (scapulohumeral rhythm) may have clinical implications when dealing with overhead athletes and patients with shoulder pathologies. [1]
Sports participation results in slight differences in side-to-side motion and in scapular resting position in overhead athletes. [5][4] Overhead athletes have some asymmetry in scapular upward rotation and scapulohumeral rhythm ratio between dominant and non-dominant shoulder. It should not be considered automatically as a pathological sign but rather an adaptation to sports practice and extensive use of upper limb. [9]
People with higher BMI have scapula kinematic patterns different from people with lower BMI. They have increased scapula upward rotation during arm elevation. [6]
Characteristics / Clinical Presentation
Scapulohumeral rhythm is a common metric for assessing muscle function and shoulder joint motion.[7] There is a three-dimensional scapular kinematic pattern during normal arm elevation that include upward rotation, posterior tilting and varying internal/external rotation dependent on the plane and angle of elevation. [1][2] When there is a changement of the normal position of the scapula related to the humerus, the scapulohumeral rhythm is disturbed.
Differential Diagnosis
There isn’t really a differential diagnosis for scapulohumeral rhythm disorders. But there are multiple causes for scapular dyskinesia and scapulohumeral rhythm disorders. [4] Causative factors can be grouped into:
- Joint causes include high grade AC instability, AC arthrosis and instability and GH joint internal derangement.
- Inflexibility causes, for example: inflexibility and stiffness of the pectoralis minor and biceps short head can create anterior tilt and protraction due to their pull on the coracoid. [4] Soft tissue posterior shoulder inflexibility can lead to GH internal rotation deficit (GIRD), which creates a ‘wind-up’ of the scapula on the thorax with reduced humeral internal rotation and horizontal abduction.
- Muscular causes: Serratus anterior activation and strength is decreased in patients with impingement and shoulder pain, contributing to the loss of posterior tilt and upward rotation causing dyskinesis. [8][6] In addition, the upper trapezius/lower trapezius force couple may be altered, with delayed onset of activation in the lower trapezius, which alters scapular upward rotation and posterior tilt. Altered scapular motion or position both decrease linear measures of the subacromial space [7][2], increase impingement symptoms, decrease rotator cuff strength [10], increase strain on the anterior GH ligaments [11]
Alterations in scapular position and control afforded by the scapula stabilizing muscles are believed to disrupt stability and function of the glenohumeral joint [2][10][11], thereby contributing to shoulder impingement, rotator cuff pathology and shoulder instability. [1]
Diagnostic Procedures
Inman, Saunders and Abbott were the first to measure scapulohumeral rhythm using radiography and suggested what became the widely accepted 2:1 ratio between glenohumeral elevation and scapulothoracic (ST) upward rotation (SUR). [8]
Since then imaging modalities (X-ray and magnetic resonance imaging)[9] , cinematography [5] , goniometry [4][6][7], and more recently 3-dimensional tracking systems [2][10][11]
Outcome measures
The Simple Shoulder Test (SST) is an internationally used patient-reported outcome for clinical practice and research purposes. It was developed for measuring functional limitations of the affected shoulder in patients with shoulder dysfunction and contains 12 questions (yes/no). It is a reliable and valid instrument for evaluating functional limitations in patients with shoulder complaints. [10]
Other frequently used questionnaires are: the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire, the [11] These questionnaires are not specific for scapulohumeral rhythm disorders, but may help in the diagnostic proces.
Examination
Observation and examination of the scapulohumeal rhythm is commonly performed by physical therapists during postural and shoulder examinations. The notion of a proper “rhythm” is routinely used to describe the quality of movement at the shoulder complex.[2]
Clinical measures (inclinometer, tape measure) are only capable of measuring scapular kinematics 2-dimensionally.
The inclinometer is capable of measuring angles (in degrees) from a horizontal reference to assess static positions of scapular upward rotation, this upward rotation can easily be used by clinicians when evaluating the scapular motion. Different authors have demonstrated that these clinical assessments give valid and accurate information regarding scapular kinematics. [6][7][2]
Linear assessment using tape measures can be used to examine possible asymmetries and patterns of abnormal motion between the pathological and healthy scapula. This examination is based on simple bilateral visual observation of scapular position. [11] Although this method is a subjective approach, research gave evidence that it is a qualitative method. [1]
Quantitative measurement of scapular positioning can also be achieved with LSST (lateral scapular slide test). This test evaluates the scapular symmetry while varying loads are placed on the supporting musculature. Three positions of the upper extremities are proposed:
- Position 1, the subject’s arm is relaxed at the side (0° of humeral elevation);
- Position 2, the subject places his or her hand on the lateral iliac crest;
- Position 3 corresponds to an internally rotated and abducted arm to 90°.
Two measurements are performed using a tape in each position (between the inferior angle of the scapula and the closest spinous process) in order to allow calculation of an average value. [6]
A 1.5-cm asymmetry in any of the positions is established as a threshold for an abnormal pattern.
Intratester reliability of the Kibler LSST method ranged from good to high, although the intertester reliability was poor. [10] Nijs et al. observed coefficients of >0.70 (interobserver reliability in intraclass correlation coefficients). The clinical importance of the tests’ outcomes, however, is questionable. [6][11]
Another test is the SDT (scapular dyskinesis test). The SDT is a visually based test for scapular dyskinesis that involves a patient performing weighted shoulder flexion and abduction movements while scapular motion is visually observed. This test consists of characterising scapular dyskinesis as absent or present and each side is rated separately. Dyskinesis is defined as the presence of either winging (prominence of any portion of the medial border or inferior angle away from the thorax) or dysrhythmia (premature, or excessive, or stuttering motion during elevation and lowering). [9] Good inter-rater reliability of this test (75–82% agreement; weighted κ=0.48–0.61) was achieved. [5]
Medical management
Optimal rehabilitation of scapulohumeral rhythm disorders requires addressing all of the causative factors that can create the dyskinesis and then restoring the balance of muscle forces that allow scapular position and motion. [7]
Physical therapy management
It is essential to make a diagnosis about the cause of the scapulohumeral rhythm disfunction before starting physical therapy. For example ‘Winged scapula’ of the scapula may be caused by a paresis of the m. Serratus Anterior or by a disfunction of the m. Trapezius.
Both passive and active movement disturbances can cause a scapulohumeral rhythm disfunction. Causes may be: shortening of muscles like m. Pectoralis Minor, m. Latissimus Dorsi and m. Levator Scapulae, shortening of the posterior joint capsule and/or lack of coordination between essential muscles like the m. Serratus Anterior, m. Trapezius and Rotatorcuff muscles. [2]
It may be clear that every therapy should be individualized.
Lengthening of muscles or connective tissue must be done by stretching and/or active and passive mobilisations. It’s important that the patient gets a home exercise program to continue stretching and mobilizations. [1] Middle thoracic manipulations in seated position have no influence on the scapulohumeral rhythm and scapular kinematics during arm flexion and thus should be avoided. [11]
Training the coordination between muscles should be done in two phases. Phase one will include the ‘setting’ of the muscles. In this phase the patient will learn how to subtle contract his muscles. Tactile feedback or myofeedback may be necessary during this phase. Practicing at home is important to train the duration of muscle contraction and train in other positions so that contraction is possible in every posture of daily life. In phase two the contraction should be automated. This can be trained with stabilisation exercises. Exercises on the back should be avoided because muscles should stabilise the scapula instead of the ground. The stabilisation exercises should be static and dynamic. [1] Examples of exercises are: push up plus, press-up, low-rowing, horizontal abduction, serratus punch and dynamic hug. [1]
Muscles should be trained in functional patterns (sport or activity specific patterns) instead of isolated patterns because it will cause maximal scapular muscle activations. [6]
Most abnormalities will occur in the eccentric phase of movements or with a lot of repetitions (fatigue). So it’s important not to forget to train the eccentric phase and endurance of the muscles. [10]
With shoulder patients you should always be aware of the influence on the spine. Some patients could have a high degree of Thoracic Hyperkyphosis. Which can be treated with active and passive mobilisations of the thoracic spine. [11]
References
- ↑ 1.01.11.21.31.41.51.61.71.81.9 Codman EA: The Shoulder,Boston: G.Miller & Company,1934
- ↑ 2.02.12.22.32.42.52.62.7 Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med 1998;26:325-337
- ↑ Cathcart CW: Movements of the shoulder girdle involved in those of the arm on the trunk. J Anat Physiol 1884; 18:209-218.
- ↑ 4.04.14.24.34.44.5 Struyf, F., Scapular positioning and movement in unimpaired shoulders, shoulder impingement syndrome, and glenohumeral instability, Scandinavian Journal of Medicine and Science in sports, jrg20, nr3, 2011, p352
- ↑ 5.05.15.25.35.45.55.6 Inman B, Saunders J, Abbott L: Observations of function of the shoulder joint. J Bone Joint Surg Br 2004; 26:1.
- ↑ 6.06.16.26.36.46.56.66.76.8 Lockhart RD. Movements of the Normal Shoulder Joint and of a case with Trapezius Paralysis studied by Radiogram and Experiment in the Living. J Anat 1930; 64: 288-302.
- ↑ 7.07.17.27.37.47.57.6 McQuade K, Smidt G: Dynamic scapulohumeral rhythm: The effects of external resistance during elevation of the arm in the scapular plane. J Orthop Sports Phys Ther 1998; 27:125–133.
- ↑ 8.08.18.28.3 Rundquist P, Anderson DD, Guanche CA, et al. Shoulder kinematics in subjects with frozen shoulder. Arch Phys Med Rehabil 2003; 84:1473–1479.
- ↑ 9.09.19.29.39.49.5 Barnes CJ, Van Steyn SJ, Fischer RA: The effects of age, sex, and shoulder dominance on range of motion of the shoulder. J Shoulder Elbow Surg 2001; 10:242– 246.
- ↑ 10.010.110.210.310.410.5 Smith J et al., Effect of scapular protraction and retraction on isometric shoulder elevation strength. Arch Phys Med Rehabil 2002;83:367–70.
- ↑ 11.011.111.211.311.411.511.611.7 Cleland J: A lecture on the shoulder girdle and its movements. Lancet 1881;1:11-12.