Objective
[1]. The STREAM is used to assess patient’s coordination, functional mobility and range of motion[2]. This outcome measure has been reported to be responsive to change in acute stroke and can be used by healthcare professionals to track the progression of stroke recovery[3]. The STREAM is an easy to use tool, that requires 15 minutes to administer and very little equipment[2].
Intended Population
STREAM is intended for use in the acute, subacute, or chronic stage of a patient’s stroke rehabilitation[4].
Overview
STREAM is a performance measure to be used in stroke recovery which assesses coordination, functional mobility, and range of motion. It is composed of 30 items and takes approximately 15 minutes to administer[2].
- Items 1 through 6 are completed with the patient in supine.
- Items 7 through 21 are completed with the patient in sitting.
- Item 22 is completed with the patient in standing, no support.
- Items 23 through 25 are completed with the patient in standing, holding onto a stable support to assist balance.
- Items 26 through 30 are completed with the patient in standing and completing walking activities.
There are three domains to this outcome measure[2]:
- Upper limb voluntary movement which is scored on a 3 point ordinal scale (0-2)
- Lower limb voluntary movement which is scored on a 3 point ordinal scale (0-2)
- Basic mobility which is scored on a 4 point ordinal scale (0-3)
There is a total of 20 possible points for each of the limb subscales (total = 40 points). There is a total of 30 possible points for the mobility subscale. If an item is not tested (due to ROM, pain, other) then an “X” is marked and that item cannot be scored. Subscales are then converted into a percentage. Total scores are calculated using the average of the 3 subscale scores[2].
A Simplified Stroke Rehabilitation Assessment of Movement (S-STREAM) was developed by Hsueh et al. in 2006. This version is more efficient to administer as it consists of half the number of items in the original STREAM. This tool may be beneficial to use when a rapid assessment is clinically important to not place unreasonable demands on patients, especially in instances in which they may be seriously unwell[5].
Method of Use
Equipment
- STREAM tool print out
- Tape or pylons
- Plinth or Chair
- Stool (18 cm high)
Set Up
- Ensure you have access to stairs
- Mark 10 meters on the ground with tape or pylons
Interpretation
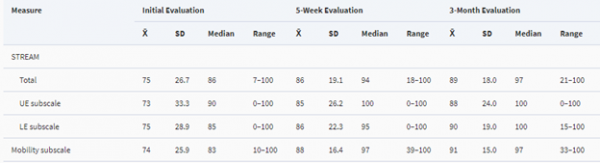
Normative Data
Ahmed et al. determined normative data for the STREAM assessment tool in 2003.
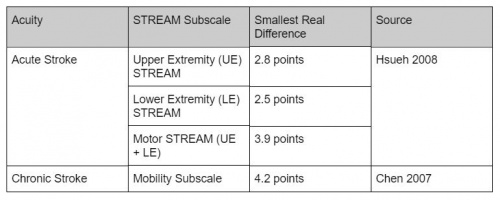
Minimal Detectable Change
Minimal Clinically Important Difference (MCID):[6]
- MCID for UE subscale = 2.2 points
- MCID for LE subscale = 1.9 points
- MCID for mobility subscale = 4.0 points
Standard Error of Measurement (SEM):[7]
SEM for chronic stroke = 1.5 points
Evidence
Reliability
Inter-rater Reliability:[8]
Inter-rater reliability of the STREAM is excellent. Inter-rater reliability for individual items of the STREAM is moderate to excellent with kappa scores ranging from 0.55 to 0.94. The intra-class correlation coefficient (ICC) for total score has been demonstrated to be 0.96 (95% confidence interval: 0.94-0.98), representing very high inter-rater reliability. Similarly, the ICCs for each subscale indicate very high inter-rater reliability. The upper extremity sub scale demonstrates the highest reliability (ICC 0.95, 0.92-0.97), followed by the lower extremity (ICC 0.92, 0.86-0.95) and mobility subscales (ICC 0.92, 0.87-0.95).
Direct Observation Inter-rater Reliability:[1]
Direct observation reliability studies suggest excellent inter-rater agreement on the scoring of individual items on the STREAM (kappa values clustered around 0.8-0.9), with the exception of the sit to stand task (kappa value of 0.65). Similarly, inter-rater reliability for each STREAM subscale score is excellent. The upper extremity subscale demonstrates the highest reliability (GCC 0.994), followed by the lower extremity (GCC 0.993) and basic mobility subscales (GCC 0.982). There are no significant differences (p
Video Observation Intra-rater Reliability:[1]
There is perfect intra-rater agreement on the scoring 85.7 % of individual STREAM items. Intra-rater agreement for each STREAM subscale is excellent; lower extremity (GCC 0.999), basic mobility (GCC 0.999) and upper extremity (GCC 0.963), where a reliability coefficient of 0.95 is recommended. Intra-rater agreement for overall STREAM scoring is comparable (GCC 0.999).
Internal Consistency[1]
Internal consistency of the STREAM is excellent demonstrated by: mobility subscale alpha 0.965, upper and lower extremity subscale alpha 0.979 and overall STREAM score alpha 0.984.
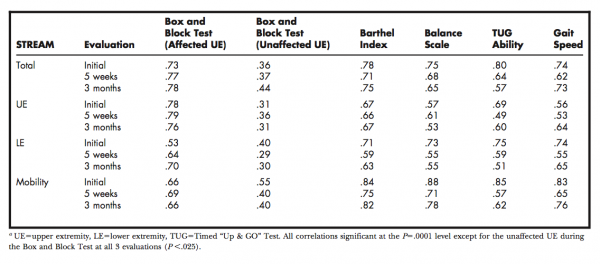
Validity[4]
The STREAM demonstrates moderate to high correlation to several outcome measures that are commonly used to evaluate motor and functional deficits in patients after acute strokes. These outcome measures include: Box and Block Test, Barthel Index, Balance Scale, Timed-Up and Go (TUG), and Gait Speed. Correlation between the STREAM and other measures of disability range from r = 0.36 and r = 0.80, specific correlations are outlined in Table One, as observed by Ahmed. Severity of stroke correlates with total and subscale STREAM scores: r = 0.66 to r = 0.77. In addition, STREAM scores successfully differentiate between levels of performance on both the Balance Scale and the Barthel Index. Because of the correlation between the STREAM and Barthel Index, the STREAM is equally useful in predicting discharge location from acute care wards after stroke. The Barthel Index is considered to be the “gold standard” for the evaluation of new outcome measures. Correlations between STREAM score and the Barthel Index score range from 0.75 to 0.78.
The STREAM score, Barthel Index and Balance Scale are most effective to measure change in individuals who experience severe symptoms after stroke. In comparison, individuals with mild to moderate symptoms show the greatest amount of change when measuring gait speed.
Responsiveness[10]
Based on standard response means (SRMs) the STREAM is highly responsive to detecting changes in motor function from 14-90 days after stroke (SRM 14-30 days post-stroke 1.17, SRM 30-90 days post-stroke 0.95). After 90 days, the STREAM becomes less responsive to change (SRM 90 – 180 days post-stroke 0.04). The changes in STREAM scores across time periods are significant (P
Limitations
One limitation of the STREAM is that it takes roughly 15 minutes to administer, which may be a significant portion of a patient’s rehabilitation appointment[4]. Some studies recommend using the S-STREAM in clinical settings as it takes less time to administer and still demonstrates reliability, validity, and responsiveness[6].
Another limitation of the STREAM is that it does have floor and ceiling effects[6]. In these cases, the S-STREAM can again be used clinically as it does not demonstrate notable floor and ceiling effects[6].
Links
http://scale-library.com/pdf/Stroke_Rehabilitation_Assessment_of_Movement_STREAM.pdf
Related Tools
The STREAM’s ability to predict discharge destination from the acute care hospital was found to be comparable to that of the following commonly used measures: Box and Block test, Berg Balance Scale, Barthel Index, Timed Up and Go test[4].
Other stroke-specific measures that can be used to assess mobility include the Fugl-Meyer Assessment, Chedoke-McMaster Stroke Assessment, Motor Assessment Scale, and Rivermead Mobility Index.
References
- ↑ 1.01.11.21.3 Daley K, Mayo N, Wood-Dauphinée S. Reliability of Scores on the Stroke Rehabilitation Assessment of Movement (STREAM) Measure. Physical Therapy. 1999 Jan 1;79(1):8–23. https://academic.oup.com/ptj/article/79/1/8/2857712 (accessed 3 May 2018).
- ↑ 2.02.12.22.32.4 Shirley Ryan Ability Lab [Internet]. Stroke Rehabilitation Assessment of Movement measure. Chicago IL: Ability Lab; c2018 [cited 2018 May 4]. Available from: https://www.sralab.org/rehabilitation-measures/stroke-rehabilitation-assessment-movement-measure
- ↑ Sullivan JE. Measurement Characteristics and Clinical Utility of the Stroke Rehabilitation Assessment of Movement Among Stroke Patients. Arch.Phys.Med.Rehabil. 2014;95(1):207-208. https://www.archives-pmr.org/article/S0003-9993(13)00581-9/fulltext (accessed 3 May 2018).
- ↑ 4.04.14.24.3 Ahmed S, Mayo NE, Higgins J, Salbach NM, Finch L, Wood-Dauphinee SL. The Stroke Rehabilitation Assessment of Movement (STREAM): A comparison with other measures used to evaluate effects of stroke and rehabilitation. Physical Therapy 2003;83(Issue 7):617-630. https://www.ncbi.nlm.nih.gov/pubmed/12837123 (accessed 4 May 2018).
- ↑ Hsueh I, Wang W, Wang C, Sheu C, Lo S, Lin J, Hsieh C. A simplified Stroke Rehabilitation Assessment of Movement instrument. Physical Therapy 2006;86(Issue 7):936-943.
https://academic.oup.com/ptj/article/86/7/936/2805160 (accessed 4 May 2018).
- ↑ 6.06.16.26.3 Hsueh IP, Hsu MJ, Sheu CF, Lee S, Hsieh CL, Lin JH. Psychometric comparisons of 2 versions of the Fugl-Meyer Motor Scale and 2 versions of the Stroke Rehabilitation Assessment of Movement. Neurorehabilitation and Neural Repair 2008;22(Issue 6):737-744. https://www.ncbi.nlm.nih.gov/pubmed/18645189# (accessed 4 May 2018).
- ↑ Chen H, Hsieh C, Lo K, Liaw L, Chen S, Lin J. The test-retest reliability of 2 mobility performance tests in patients with chronic stroke. Neurorehabilitation and Neural Repair, 2007 July 1; 21(4), 347-352. http://journals.sagepub.com/doi/pdf/10.1177/1545968306297864 (accessed 6 May 2018)
- ↑ Wang CH, Hsieh CL, Dai MH, Chen CH, Lai YF. Inter-rater Reliability and Validity of the Stroke Rehabilitation Assessment of Movement (STREAM) Instrument. J Rehabil Med 2002;34:20-4. https://pdfs.semanticscholar.org6167/67696a553faddf1821c8d145a01dca9c9872.pdf (accessed 3 May 2018).
- ↑ Ahmed S, Mayo NE, Higgins J, Salbach NM, Finch L, Wood-Dauphinee SL. The Stroke Rehabilitation Assessment of Movement (STREAM): A comparison with other measures used to evaluate effects of stroke and rehabilitation. Physical Therapy 2003;83(Issue 7):617-630. https://www.ncbi.nlm.nih.gov/pubmed/12837123 (accessed 4 May 2018).
- ↑ Hseuh IP, Wang CH, Sheu CF, Hsieh CL. Comparison of Psychometric Properties of Three Mobility Measures for Patients with Stroke. Stroke 2003;34:1741-5. http://stroke.ahajournals.org/content/34/7/1741. (accessed 5 May 2018).