Definition/Description
Septic arthritis is also commonly referred as bacterial or infectious arthritis. Septic arthritis is an intensely painful infection in a joint. [1]Bacteria, viruses and fungi may invade the joint through various routes which cause inflammation of the synovial membrane. [2] With the onset of inflammation, cytokines and proteases are released, thus resulting in potential joint destruction. [3] The infection is located in the synovial or periarticular tissues and is most commonly bacterial. [4] Bacteria or other foreign pathogens can infect either one joint or, if left untreated, can spread and cause further systemic damage. Septic arthritis may occur at any age but is more likely in children and older adults. The most commonly targeted joins in the body are the knee, hip, shoulder, ankle and wrists. [5]
Prevalence
In the United States, there are approximately 20,000 cases of septic arthritis reported each year. [5] The most common strain is the staphyloccoccus aureus which is found in 60% of positive cultured joint aspirations. In non gonococcal strains, which includes staphylococcus, this incidence can increase to 28-38 cases per 100,000 in individuals also diagnosed with Rheumatoid Arthritis. [5]
Characteristics/Clinical Presentation[2][3][4]
Typical presentation of septic arthritis in children and adults includes:
- Acute, rapid onset of pain
- Unable to move the joint through active and passive range of motion
- Typically only one joint (can be bilateral or more than one joint depending on the type of infection)
- Unable to bear any weight on the joint
- Effusion
- Joint warmth
- Skin rash
- Low grade fever
- Lymphadenopathy
- The joints of the arms and legs are the most commonly affected in adults (especially the knees)
- The hip joint is most commonly affected in children
Symptoms in Newborns/Infants [6]
- Cries when infected joint is moved
- Fever
- Unable to move the limb
- Irritability
Note: A patient may be taking medications for other types of arthritis that may mask the original signs and symptoms of septic arthritis. Early diagnosis for proper treatment is critical. [1]
Prognosis:
Several factors influence how well the joint can fight the infection including other systemic issues occurring throughout the body. For example, patients with liver or kidney disease, or diseases that make the joint more susceptible to damage such as RA can all cause poorer outcomes [4][7]. The best outcome for individuals with septic arthritis is immediate treatment. Fifty percent of adults with septic arthritis have significant decreased range of motion or chronic pain after the infection.[1][4] Poor outcome predictors in prognosis of septic arthritis include the following: Age older than 60, infection of the hip or shoulder joints, underlying rheumatoid arthritis, positive findings on synovial fluid cultures after 7 days of therapy, delay of 7 days or longer in beginning treatment.[5] Depending on associated risk factors, infection type, and response to treatment, mortality rate from septic arthritis has varied between published studies. One systematic review stated that mortality rate was around 11% between the studies assessed.[7]
Associated Co-morbidities[2]
• Systemic corticosteroid use
• Radiation therapy
• Preexisting arthritis
• Arthrocentesis: joint aspiration
• Human Immunodeficiency virus
• Diabetes Mellitus
• Alcohol or drug use
• Trauma
• Other infectious diseases
Medical Management
The course of treatment for septic arthritis is case dependent. There is no conclusive evidence on the most effective way to begin[7]. However, it is a combination of antibiotics, joint fluid removal, infection drainage, and/or total joint surgery. The course of treatment also depends on the type of joint invasion (bacterial, STD bacterial, viral etc..). The first round antibiotics can be directed at the most likely pathogen, then the joint can be tested to see what further treatment may be necessary such as needle joint aspiration or drainage to release the fluid. Another option is to perform joint aspiration before a round of antibiotics is chosen. If the infection is severe enough following a round of antibiotics and aspiration for fluid removal, surgery or even replacement of the entire joint may be necessary. [4]
Antibiotic treatment:
Typically, the sexually transmitted related bacteria (gonococcal) is treated with antibiotics that other sexually transmitted infections are treated with. For example, doxycycline, ciproflaxin, and azythromyocin, amongst many others. The non-sexually transmitted bacterial infections can be treated with common antibiotics such as penecillin, vancomyocin, (etc), depending on the severity and resistance tendencies of the bacterial strain. [4][5]
Below is non-exhaustive list of antibiotics commonly used in the treatment of septic arthritis: [5]
- Ceftriaxone (Rocephin)- Effective against gram-negative enteric rods
- Ciprofloxacin (Cipro) – Treat N gonorrhoeae and gram-negative enteric rods.
- Cefixime (Suprax) –Broad activity against gram-negative bacteria, by binding to one or more of the penicillin-binding proteins. Arrests bacterial cell wall synthesis and inhibits bacterial growth.
- Oxacillin – Oxacillin is useful against methicillin-sensitive S aureus (MSSA).
- Vancomycin (Vancocin) – An anti-infective agent used against methicillin-sensitive S aureus (MSSA), methicillin-resistant coagulase-negative S aureus (CONS), and ampicillin-resistant enterococci in patients allergic to penicillin.
- Linezolid (Zyvox) – An alternative antibiotic that is used in patients allergic to vancomycin and for the treatment of vancomycin-resistant enterococci.
Management regarding antibiotic choice, dosage, route of administration, and duration of treatment is unknown in the treatment of septic arthritis. In addition, no evidence has shown if closed aspiration or open arthroscopy is better at removing materials from a joint that’s infected.[8]
Joint Drainage and Surgical options (often used in combination with antibiotic treatment)
Much like antibiotics, the choice whether to use joint aspiration, arthroscopy, or total joint replacement is case dependent. There is no current definitive evidence on whether one treatment is more effective than the other. However, the most positive outcomes in general come from using one of these options. The main goal with this treatment is to continuously remove the accumulation of pus within the joint until it no longer forms. This is most commonly used in combination with the antibiotics to remove the pus both from the joint itself and via bloodstream. [4][7]
Diagnostic Tests/Lab Tests/Lab Values [1]
Joint aspiration:
Needle joint aspiration can be used as both a diagnostic tool and a treatment. A portion of the fluid can be taken out by aspiration needle to determine the type of bacteria causing the infection thus determining further course of treatment.
Other diagnostic lab values:
- Arthrocentesis with synovial fluid examination and culture
- Increased White blood cell count
- Increased Erythrocyte sedimentation rate (ESR)
- Increased Temperature
- Increased C-Reactive Protein (CRP)
- Imaging studies are used to rule out other conditions
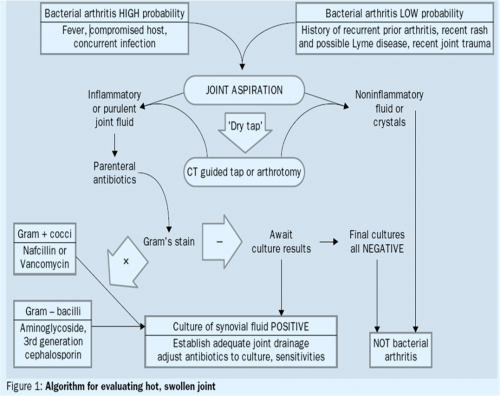
Below is an algorithm developed from a systematic review of bacterial septic arthritis patients for evaluating a hot swollen joint:
Etiology/Causes[2][3]
Septic arthritis is also known as infectious or bacterial arthritis and involves a local response causing inflammation of the synovial membrane of the joint affected. This is due to the invasion of bacteria, viruses, or fungi directly into the synovial membrane of the joint. The most common cause is bacterial, more specifically staphylococcus aureus, streptococci, or gonococci, a bacteria transferred via sexual activity. It can also be caused by viral infections such as Hepatitis B or Rubella.
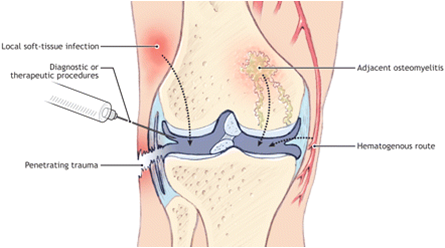
The bacterial or viral infection enters the joint via the bloodstream by three different ways:
- Direct inoculation via surgery, arthroscopy, injection, central lines, or total joint replacements.
- A wound that that breaks the skin such as a bite, cut, or open fracture.
- Another systemic infection such as osteomyelitis, cellulitis, diverticulitis, or an abscess reaches the joint causing another infection.
Associated risk factors: [3][8]
Two of the most important factors that put a patient at risk are a pre-existing joint pathology, especially Rheumatoid Arthritis, or a recent prosthetic joint surgery. Other risk factors to be considered are:
- Increasing age
- History of infection of any kind
- Autoimmune conditions such as Systemic Lupus Erythematosus
- Scleroderma or mixed connective tissue disease
- Diabetes
- Sarcoidosis
- Human bite or tick bite
- Fracture
- Central line placement
- Indwelling catheter
- Immunocompromised condition
- Chronic joint damage (RA, OA)
- Sexually transmitted infection
- Injection drug user
- Alcoholism
- Recent immunization
- Malnutrition
- Skin breakdown
- Rarely seen is a case of Infectious Arthritis as a complication from ACL reconstruction due to contaminated bone-tendon-bone allografts.
Systemic Involvement
Septic arthritis presents with a multitude of signs and symptoms affecting visceral systems. Joint symptoms may present in conjunction with a skin rash, low-grade fever, chills, and lymphadenopathy.[3] Bilateral joint involvement is common in the fingers, knees, shoulders, and ankles. The classic signs of infection may be present including increased temperature, swelling, redness, and loss of function. [2] Acute symptoms of an arthritic joint in the presence of fever should alert the health care provider of potential septic arthritis and should be treated as a medical emergency. [3]
Physical Therapy Management (current best evidence)[5]
The initial treatment of infectious arthritis is outside of the scope of physical therapy. It is important, first, for the physical therapist to recognize the signs and symptoms of the infection and refer out for other medical treatment. Subjective history, in combination with the physical therapist’s objective findings, is important in order to recognize the risk factors that make septic arthritis the likely diagnosis. It is important to immobilize the joint in this stage to best manage the patient’s pain and to decrease likelihood of doing further damage to the joint until proper treatment can occur.
Once the patient receives a round of antibiotic treatment in combination with either joint aspiration, debridement, or arthroscopy, the patient may then be referred back to physical therapy to be educated on how to properly protect the affected joint. Gentle mobilization of the infected joint can begin if the patient is responding well following 5 days of medical treatment. Once the infection is well-managed, current evidence states the patient will usually respond best to aggressive physical therapy to allow maximum post-infection functioning. Physical therapy needs to consist of allowing the joint to be in its functional position and positioning the joint to allow passive range of motion activities.
Differential Diagnosis
If a patient is suspected to have septic arthritis, the most important alternative diagnoses to consider are rheumatologic conditions. These include, but are not limited to, rheumatoid arthritis, vasculitis, and crystalline arthritides. Other forms of systemic arthritic conditions such as drug-induced arthritis, and all forms of reactive arthritis, may also be considered.[5] With the immediacy of joint destruction with septic arthritis, the differential diagnosis must be performed with urgency to initiate proper treatment immediately. Additional conditions that can cause global or local joint pain and swelling that may resemble septic arthritis include: osteoarthritis, HIV infection, Lyme disease, gout, and lupus. In order to properly diagnose septic arthritis over one of these other conditions, testing of joint fluid and symovial lining must be performed. A diagnosis cannot be made on clinical presentation alone.[2][3]
Case Reports/ Case Studies
Pneumococcal polyarticular septic arthritis after a single infusion of infliximab in a rheumatoid arthritis patient
A 38 year old male with RA is diagnosed with polyarticular septic arthritis after receiving immunosuppressant injections to treat his RA flare up. This case addresses the need for clinicians to recognize these injections can possibly cause the joints to become infected, the need to distinguish these symptoms from normal RA symptoms, and how RA can worsen the presentation and progression of the infection.
Resources
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1: There was a problem during the HTTP request: 422 Unprocessable Entity
Recent Related Research (from
References
- ↑ 1.01.11.21.3 Mayo Clinic [Internet]. Mayo Foundation for Medical Education and Research; 2015 [cited 2017 April 4]. Availablefrom: ↑ 2.02.12.22.32.42.5 Goodman CC, Fuller KS. Pathology: implications for the physical therapist. 4th ed. St. Louis: Saunders Elsevier; 2014.
- ↑ 3.03.13.23.33.43.53.6 Goodman CC, Snyder TEK. Differential diagnosis for physical therapists: screening for referral. 5th ed. St. Louis: Saunders Elsevier; 2012.
- ↑ 4.04.14.24.34.44.54.6 The Merck Manual [Internet]. Whitehouse Station: Merck Sharp & Dohme Corp.; 2014 [cited 2017 April 4]. Available from: ↑ 5.05.15.25.35.45.55.65.7 Brusch, J. Medscape [Internet]. Septic Arthritis; 2016 [updated 2016 October 21; [cited 2017 April 4] Available from: ↑ Pub med [Internet]. Bethesda: National Center for Biotechnology Information; 2012 [cited 2017 April 4]. Available from : ↑ 7.07.17.27.3 Matthews CJ, Weston VC, Jones A, Field M, Coakley G. Bacterial septic arthritis in adults. The Lancet. [Internet] [Cited 2017 March 28] ;2010;375(9717):846-855. Available from: ↑ 8.08.1 Matthews CJ, Kingsley G, Field M, Jones A, Weston VC, Phillips M, et al. Management of septic arthritis: a systematic review. Ann Rheum Dis. 2007 [cited 2017 April 4]; 66: 440-45. Available from NCBI with Full Text: ↑ Kherani R, Shojania K. Septic arthritis in patients with preexisting inflammatory arthritis. Canadian Medical Association Journal [Internet]. 2007 May 22 [cited 2017 April 4];176(11):1605–8. Available from: ↑ 10.010.1 YouTube. Septic arthritis of the knee arthroscopic debridement. Available at: function gtElInit() { var lib = new google.translate.TranslateService(); lib.setCheckVisibility(false); lib.translatePage('en', 'pt', function (progress, done, error) { if (progress == 100 || done || error) { document.getElementById("gt-dt-spinner").style.display = "none"; } }); }