Definition/Description
Diffuse Idiopathic Skeletal Hyperostosis (DISH) refers to a non-inflammatory disease that is characterized by ossification/calcification of soft tissues, entheses, and spinal ligaments. DISH primarily affects the Anterior Longitudinal Ligament (ALL) at the attachment sites to bone in the vertebral column[1][2][3][4][5][6][7]. DISH is a complex disorder that not only affects the musculoskeletal system, but also can cause additional gastrointestinal, respiratory, cardiovascular, and neurological impairments due to bone compression of adjacent structures[1][4][6][7].
Prevalence
The reported prevalence of diffuse idiopathic skeletal hyperostosis is widely varied throughout the course of available research[5]. One of the main reasons for this variability is the different locations of structural manifestations in the vertebral column. The recent evidence of DISH reports prevalence of the disease is increased in with increasing age more prominently found in the 60s and 70s[1][2][3][7]. DISH is found to affect the axial skeleton with the thoracic spine (T7-T11), being the most common levels affected[1][2][4][7]. Other structures commonly affected include: pelvis, patella, calcaneus, and the olecranon[1][4][5]. It has also been discussed throughout the research that a genetic component has a possible place in the role of development and diagnosis of the disease[1][5][7].
Characteristics/Clinical Presentation
DISH has been found to be present asymptomatically in most clinical cases. However, due to the varying manifestations and differing locations of the characteristics of the disease, a number of characteristics can be seen in clinical presentations. These characteristics are typically attributed to altered biomechanics of the axial skeleton that lead to pain and decreased mobility. Other symptoms can include, but are not limited to the following characteristics[1][2][3][4][5][6][7]:
- Decreased ROM – Primarily in the Axial Skeleton or Peripheral Joints
- Stiffness
- Pain
- Dysphagia
- Respiratory Distress
- Odynophagia
- Cough
- Hoarseness
- Pharyngeal Perforation
- Weight Loss
- Reflux
- Dysphonia
- Horner’s Syndrome
- Aphonia
Associated Co-morbidities
DISH has been shown to have a multiple associations with a number of conditions and dysfunctions. One of the most prevalent associations according to recent research is to metabolic syndromes[1][6]. The following conditions are shown to be commonly associated with the diagnosis of DISH across the spectrum of individuals affected.
- Diabetes Mellitus[1][2][3][4][5][6][7]
- Obesity[1][2][3][4][5][6][7]
- Dyslipidemia[1][3][5][6][7]
- Hyperuricemia[1][3][5][6][7]
- Hyperinsulinemia[1][3][5][7]
- Osteoarthritis[1][3][4][6]
- Cardiovascular conditions including, but not limited to hypertension, atrial fibrillation, left ventricular hypertrophy, peripheral arterial disease, and cardiovascular disease[1][3].
- Increased Risk of Fracture[1][2][3][6]
- Neurological impairments, while typically uncommon with the presentation of this disease, can manifest in the form of spinal cord compression, muscle weakness, numbness and tingling, and sesory loss[1][4][7].
Medications
Current research does not outline a specific and definitive schedule of medications used to treat DISH. The following medications have been used as a method of control and/or manage the symptoms of the disease process[1][4][5][6].
- Analgesics
- Anti-Inflammatories
- Muscle Relaxants
- Corticosteroids
- Sedation
- Reflux Medications
- Gastro-Protectants
Diagnostic Tests/Lab Tests/Lab Values
The most commonly used classification criteria to diagnose DISH was designed by Resnick and Niwayama in 1976 and includes the following[1][2][3][5][6][7]:
- Anterolateral ossifications of at least 4 contiguous thoracic segments.
- Preservation of intervertebral disc spaces
- Absence of apophyseal joint degeneration or SI inflammatory changes.
A formal diagnosis of DISH does not require or mandate the presence of constitutional and metabolic abnormalities; however, it is known through numerous studies that systemic conditions are associated with DISH in varying degrees[2][3][5][6][7].
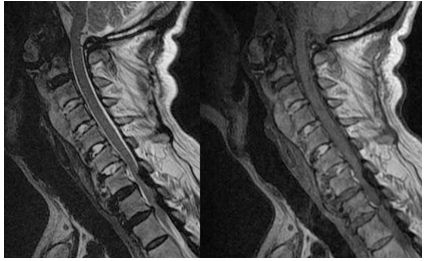
Specific features shown either through a radiograph, MRI, or CT scan in patients who are diagnosed with DISH could include a few of the following and not all are required to be seen to have the diagnosis of DISH[1][2][3][5][7]
1. Spinal Features[2]
- Flowing ossification along the anterior or right anterolateral aspects of at least 4 consecutive vertebrae
- Well preserved disc space
- No inflammation at sacroiliac joint or facet joint ankylosis
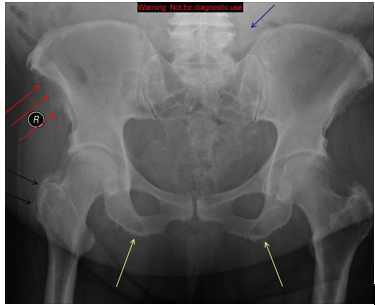
2. Extraspinal Features[2]
- Enthesopathies, which is a disorder involving attachment of tendon or ligament to bone at the entheses, are commonly seen in the iliac crest, ischial tuberosity, and greater trochanters.
- Spur formation in appendicular skeleton seen at the olecranon process, patellar ligament, and calcaneus.
Etiology/Causes
The current research on DISH lacks a definitive cause of the disease. A number of theories have been postulated that relate abnormal growth and function of osteoblasts in the osteoligamentous binding centers that; however, this is not a widely accepted theory among the current research[1][2][4][5][6]. There are certain factors that have come to be associated with DISH and are thought to have some relation to the pathophysiology behind the disease process.
- Metabolic Syndromes[1][2][3][4][5][6][7]
- Chronic Medication Use: Isotretinoin, Etretinate, Acitretin, Retinoids[3][4][5]
- Genetic Factors: HLA-B27[5][7]
- Environmental Exposures: Fluoride, Retinal, Vitamin A Toxcicity[4][5][7]
Systemic Involvement
Due to the high association of metabolic syndromes with the diagnosis of DISH, it is common to see systemic involvement in individuals who have this condition. A majority of metabolic syndromes associated with DISH have a link to obesity and a sedentary lifestyle which can in turn be a cause of diabetes, hyperlipidemia, and hypertension. The following conditions are associated with a diagnosis of DISH[1][2][3][4][5][6][7].
- Obesity
- HTN
- DM
- Hyperinsulinemia
- Dyslipidemia
- Hyperuricemia
- Metabolic Syndromes
Medical Management
Therapy and treatment for DISH is based on the individual’s presentation of symptoms due to the lack of well-designed studies evaluating the effectiveness of any type of medical management for this disease[1][3][4][5][7]. Given the lack of disease-modifying therapeutics, the suggested treatment of DISH has been directed towards musculoskeletal symptoms, the associated metabolic and constitutional comorbidities, and any other complications that may arise[1][2][3][4][5][6][7]. The majority of patients with DISH have found the use of physical therapy, analgesics, sedation, anti-inflammatory drugs, and muscle relaxants to all be successful in managing this condition[4][5][6][7]. In general, the following multi-system therapeutic interventions have been shown to work best[1]:
Non-Surgical Management
- Dietary Modification: Fluids and Soft Food
- Medications[4][6][7]
- Percutaneous Endoscopic Gastrostomy Placement[1]
- Physical Therapy[4][6]
Surgical Management
Surgical approaches have only been indicated for extreme cases where the patient has severe symptoms such as: obstructed airway and/or dysphagia, conservative approaches have failed, or they fall in the younger age range with severe signs and symptoms[1][4][5][6]. The following are surgical possibilities for those who qualify:
- Anterolateral, Lateral, or Transpharyngeal Resection of the Ossification
- Spinal Decompression
- Discectomy
- Spinal Fusion
Physical Therapy Management
Even though there is no cure for DISH, receiving physical therapy services can assist individuals in the following way who suffer with musculoskeletal or movement related impairments from the disorder[4][6]:
- Increase Mobility
- Pain Relief
- Weight Reduction
- Joint Protection
- Falls Prevention
Differential Diagnosis
There are a few features that can help assist in differentiating DISH from other pathological diseases which can include developing in joints that are rarely affected by osteoarthritis-shoulder, elbow, and metacarpophalangeal joints, developing from bone that is distant from the bone-cartilage junction, and DISH affects distinctive entheses such as the calcaneal spur and quadriceps tendon. Below are diagnoses that could potentially present with similar signs, symptoms, and findings as DISH[2][5][7]:
- Juvenile Idiopathic Arthritis (JIA) should be considered if suspected in children[2].
- Acromegaly[4][7]
- Fluorosis[7]
- Ochronosis[7]
Case Reports/ Case Studies
1. Radswiki, Weerakkody Y, Jones J, Schubert R, Patel M, Niknejad M et al. Diffuse idiopathic skeletal hyperostosis | Radiology Reference Article | Radiopaedia.org [Internet]. Radiopaedia.org. 2016 [cited 21 March 2016]. Available from: 2. Zhang C, Ruan D, He Q, Wen T, Yang P. Progressive dysphagia and neck pain due to diffuse idiopathic skeletal hyperostosis of the cervical spine: a case report and literature review. CIA. 2014;:553.
3. Proescholdt F, Markart M, Ertel W. Postoperative radiotherapy in diffuse idiopathic skeletal hyperostosis: prophylaxis of recurrence after resection of osteophytes from C3 to C5 in a case of dysphagia. Journal of Surgical Case Reports. 2014;2014(1)
4. Murayama K, Inoue S, Tachibana T, Maruo K, Arizumi F, Tsuji S et al. Ossified Posterior Longitudinal Ligament With Massive Ossification of the Anterior Longitudinal Ligament Causing Dysphagia in a Diffuse Idiopathic Skeletal Hyperostosis Patient. Medicine. 2015;94(32):e1295.
5. Hasegawa K, Takahashi H, Iida Y, Yokoyama Y, Fukutake K, Takamatsu R et al. Spontaneous Symptomatic Pseudoarthrosis at the L2-L3 Intervertebral Space with Diffuse Idiopathic Skeletal Hyperostosis: A Case Report. Case Reports in Orthopedics. 2013;2013:1-4.
6. Anvekar D. Neuroradiology Cases: DISH [Internet]. Neuroradiologycases.com. 2012 [cited 7 April 2016]. Available from:
Resources
References
- ↑ 1.001.011.021.031.041.051.061.071.081.091.101.111.121.131.141.151.161.171.181.191.201.211.221.231.241.251.261.27 Terzi R. Extraskeletal symptoms and comorbidities of diffuse idiopathic skeletal hyperostosis. World Journal of Clinical Cases. 2014;2(9):422
- ↑ 2.002.012.022.032.042.052.062.072.082.092.102.112.122.132.142.152.162.172.18 Radswiki, Weerakkody Y, Jones J, Schubert R, Patel M, Niknejad M et al. Diffuse idiopathic skeletal hyperostosis | Radiology Reference Article | Radiopaedia.org [Internet]. Radiopaedia.org. 2016 [cited 21 March 2016]. Available from: ↑ 3.003.013.023.033.043.053.063.073.083.093.103.113.123.133.143.153.163.173.18 Mader R, Sarzi-Puttini P, Atzeni F, Olivieri I, Pappone N, Verlaan J et al. Extraspinal manifestations of diffuse idiopathic skeletal hyperostosis. Rheumatology. 2009;48(12):1478-1481.
- ↑ 4.004.014.024.034.044.054.064.074.084.094.104.114.124.134.144.154.164.174.184.194.204.214.22 Diffuse idiopathic skeletal hyperostosis | Disease | Overview | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program [Internet]. Rarediseases.info.nih.gov. 2016 [cited 21 March 2016]. Available from: ↑ 5.005.015.025.035.045.055.065.075.085.095.105.115.125.135.145.155.165.175.185.195.205.215.225.235.245.25 Nascimento F, Neto H, Gatto L, Lages R, Demartini Z, Koppe G. Diffuse idiopathic skeletal hyperostosis: A review. Surgical Neurology International. 2014;5(4):122.
- ↑ 6.006.016.026.036.046.056.066.076.086.096.106.116.126.136.146.156.166.176.186.196.206.21 Mader R, Verlaan J, Buskila D. Diffuse idiopathic skeletal hyperostosis: clinical features and pathogenic mechanisms. Nat Rev Rheumatol. 2013;9(12):741-750.
- ↑ 7.007.017.027.037.047.057.067.077.087.097.107.117.127.137.147.157.167.177.187.197.207.217.227.237.247.257.267.27 Bombak A. Diffuse Idiopathic Skeletal Hyperostosis and the Osteological Paradox. Totem: The University of Western Ontario Journal of Anthropology. 2012;20(1):1-19.