Description [1]
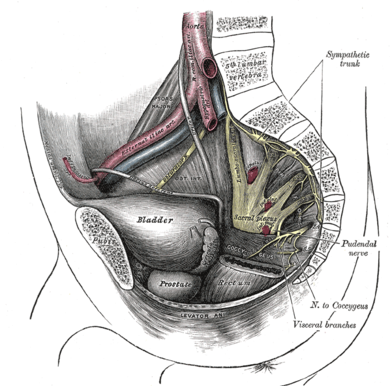
The sacral pleux is situated on the posterolateral wall of the pelvic cavity, lying anterior to the Piriformis. The sacral contributions pass out of the anterior sacral foramina and course laterally & inferiorly on the pelvic wall. A majority of the nerves originating from the sacral plexus pass through the greater sciatic foramen – inferior to the piriformis muscle – and enter the gluteal region of the lower limb. The remaining follow various courses or do not leave the pelvic cavity.
Root
The sacral plexus is formed by the anterior rami of S1 to S4 as well as the lumbosacral trunk (anterior ramus of L4 & L5). The lumbosacral trunk courses vertically into the pelvic cavity from the abdomen and passes immediately anterior to the sacro-iliac joint.
Branches
The sacral plexus provides motor and sensory innervation through the following nerves:
- Sciatic Nerve (L4 – S3)
- Pudendal Nerve (ventral divisions of S2 – S4)
- Superior Gluteal Nerve (dorsal divisions of L4 – S1)
- Inferior Gluteal Nerve (dorsal divisions of L5 – S2)
- Nerve to Obturator Internus (ventral divisions of L5 – S2)
- Nerve to Quadratus Femoris
- Posterior Femoral Cutaneous Nerve
- Perforating Cutaneous Nerve
- Nerve to Piriformis
- Obturator Nerve (L2 – L4)
Clinical relevance
- Lesions of the sacral plexus can be caused by pelvic fractures, hip surgery, malignant infiltration, local radiotherapy, and the use of orthopaedic traction tables. These lesions are usually unilateral and do not result in significant sexual dysfunction unless the sensory symptoms become disruptive.[2]
- Cancers can invade the sacral plexus causing pain radiating pain syndromes similar to sciatic nerve lesions.[3] Numbness in the perianal region as well as involvement of sympathetic fibers causing “hot and dry foot” [4] can be found.
- The sacral plexus can be entrapped by the fetal head at the pelvic brim during the final trimester of pregnancy or labour. The clinical syndrome will resemble an L5 radiculopathy and symptoms will usually resolve completely on its own 4 – 6 months post-birth. [5]
Assessment [6]
- Sensory testing has moderate sensitivity in the detection of lumbo-sacral radiculopathy
- prior knowledge of MRI results is a source of bias in sensory testing
- In clinical practice, diagnosis of lumbo-sacral radiculopathy should always be reached through the combined use of sensory, motor, and deep tendon reflex tests – not through single test results.
Treatment
| Physiotherapy [7] | – patients with severe neuropathic incontinence should first undergo intensive conservative management including physiotherapy/pelvic floor retraining (biofeedback) before surgical treatment is considered. |
| Sacral Nerve Stimulation [8] | – there is good emerging evidence for treatment of patients with end-stage faecal incontinence |
Resources
References
- ↑ Drake RL. Vogl AW. Mitchell AWM. Gray’s Anatomy for Students. 3rd edition. Philadelphia: Churchill Livingstone Elsevier. 2015.
- ↑ Vodusek DB. Boller F. editors. Neurology of Sexual and Bladder Disorders. Vol 130. Oxford: Elsevier. 2015
- ↑ Grisold W. Grisold A. Locher WN. Neuromuscular complications in cancer. Journal of Neurological Sciences. 2016;367:184-202
- ↑ Dalmau J. Graus F. Marco M. “Hot and dry foot” as initial manifestation of neoplastic lumbosacral plexopathy. Neurology. 1989;39:871.
- ↑ Said G. Krarup C. editors. Peripheral Nerve Disorders. Vol 130. Amsterdam: Elsevier. 2013.
- ↑ Tawa N. Rhoda A. Diener I. Accuracy of clinical neurological examination in diagnosing lumbo-sacral radiculopathy: a systematic literature review. BMC Musculoskeletal Disorders 2017;18:93-104
- ↑ Weledji EP. Electrophysiological Basis of Fecal Incontinence and Its Implications for Treatment. Annals of Coloproctology. 2017;33:161-168.
- ↑ Tjandra JJ. Lim JF. Matzel K. Sacral Nerve Stimulation: An Emerging Treatment for Faecal Incontinence. ANZ Journal of Surgery. 2004; 74:1098-1106.
- ↑ Ninja Nerd Science. Neurololgy | Sacral Plexus. Available from: function gtElInit() { var lib = new google.translate.TranslateService(); lib.setCheckVisibility(false); lib.translatePage('en', 'pt', function (progress, done, error) { if (progress == 100 || done || error) { document.getElementById("gt-dt-spinner").style.display = "none"; } }); }