Introduction
Originating from the work of Donald Schon[1] the concept of reflective practice is recognised as a key component of developing and maintaining professional best practice in many disciplines. This practice in the healthcare context is termed clinical reflection and is a set of skills commonly developed from university level. With the ever growing pressures for service development and self progression this is now an essential skill that should be put into practice regularly by every health care professional. [2]
So this page is going to run through:
- What is reflection and why we use it
- The reflective journey
- Different methods of reflection
What is Reflection / Reflective Practice?
Reflection and reflective practice is advocated by many professional bodies to promote high quality service delivery, but what is reflection and reflective practice? Here are some definitions:
- “Reflection is a process of reviewing an experience of practice in order to describe, analyse, evaluate and so inform learning about practice” [3]
- “Reflective practice is something more than thoughtful practice. It is that form of practice that seeks to problematise many situations of professional performance so that they can become potential learning situations and so the practitioners can continue to learn, grow and’ ‘develop in and through practice” [4]
- “a window through which the practitioner can view and focus self within the context of his/her own lived experience in ways that enable him/her to confront, understand and work towards resolving the contradictions within his/her practice between what is desirable and actual practice” [5]
- “conscious and systematic approach to thinking about experiences with the aim of learning and changing behaviours.”[6]
Clinical reflection is a tool which enables the individual to learn from their experiences and actions, this is not only applicable in the health care setting but through day to day life. It enables the individual to learn from mistakes and poor choices they take and acknowledge when things have gone well so this can be repeated; but to clinically reflect and utilise this skill in the health care setting needs some practice, as this requires critical thinking. [7] It helps the therapist to figure out what is known already and then add the new information that was gained, resulting in better understanding, knowledge and a new meaning.[6]
By “consiously looking and thinking about experiences, actions, emotions, feelings and responses” we can interpret them so that we can learn thus you become more critical about your views of practice and the world.[6]
Watch this video on reflective learning to find out more.
The Reflective Journey
It has been acknowledged that critical reflection in clinical practice is essential for clinical effectiveness and continuing professional development. There is evidence to suggest that critical reflection is difficult without expert guidance, therefore educational institutions are now incorporating this into their programmes to establish this skills early in the individual’s professional career. Reflection and critical analysis is a skill which needs to be practised in order to be developed. [8][9]
Quite often student health care professionals will start of their reflective development journeys by being given the task of keeping a reflective journal or diary of their day on clinical placements. This journal will involve certain thought provoking questions to facilitate and direct the reflection such as:
- What happened
- Why did you choose that method
- Is there any research to support your decisions
- What went well
- What could have gone better
- Action points for implementation next time [10]
It is encouraged that reflections are initially written; this will help to cement the different stages of reflection, but once this skill is developed health care professionals can do this regularly (internally) throughout the day. They then may only reflect formally (written) upon an event or activity that was particularly significant for them.[11]
Watch this small lecture from the London deanery on reflection and learning in the workplace. This is aimed at trainee doctors but the principles can be translated into any health care profession.
Methods of Reflection
There are many forms of formal reflection, all differing slightly. There is no right or wrong method of reflection as long as it is:
- A record which is useful to you
- A cue to memory
- Honestly written
- Enjoyable to complete
- Involve thinking which is objective, critical and deep
Reflection-on-action [6]
- done by novice practitioners
- after the event, thinking about “beliefs, expectations and biases”
- thinking about what happened, actions that were performed and what could change the outcome next time
- this reflection changes experience to knowledge
Reflection-in-action [6]
- “reflecting on practice while it is happening”.
- done by expert practitioners
- “on the spot research” – while the practitioner gains new understanding of the situation the situation is changed
- it requires “conscious attention to the task”
- the practitioner acts as their own supervisor and questions their own actions (meta-reflection on the reflection)
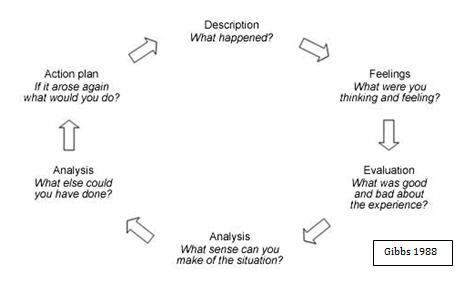
There are many different frameworks offered for structuring reflection. Here is a Gibbs Reflective Cycle (1988)
Gibbs reflective cycle is a formal structure which can be used for academic pieces of work but also in clinical practice which can be used to evidence continuing professional development. [12]
Description
The section in the reflective cycle is describing the event that is being reflected upon. Is only needs to be short and precise to give background information on the event.
Feelings
This section focuses on thoughts and feelings at the time of the event and after.
Evaluation
The evaluation is reflecting upon the experience, such as;
- How you reacted to the situation,
- How did you react after,
- How did other people react
- If it was a problem solving situation – was the issue resolved.
If there are pieces of evidence for the event you are reflecting upon you can include these here.
Analysis
This section is where you can really demonstrate your reflection on the experience. Pick out points that you think have hindered or enhanced the experience. What went well, and what has not gone so well. Similarly to the evaluation section where references may have been incorporated, the analysis section is where you can link your experience to what the literature is reporting. This is where you will improve your grades if this is an academic piece of work, but also useful for using it as a piece of evidence in a portfolio for continued education purposes.
Conclusion
This section is about summarising the outcome of the event being reflected upon.
- Would you do the same again
- What would you change
- Identify what you could do to stop the same things from happening in future
- or how can you make sure the same happens again to ensure the same positive outcome
Action Plan
This section is essential to any reflection, this is about what you are going to do next. How are you going to implement the changes you have identified to achieve the desired outcome next time, be it performance improvement or maintaining the standard achieved.
John’s Model for Structured Reflection (2000)
John’s Structured Reflective model is exactly that. It is a set of questions that are asked to direct the reflector through the process. This may be attractive to some people, but potentially could be a little restrictive for others. [13]
|
Description |
|
| Reflection |
|
| Influencing Factors |
|
| Evaluation |
|
| Learning |
|
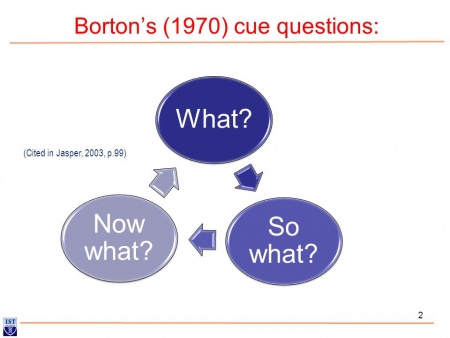
Borton’s/Driscoll’s Development Framework
Borton’s three Whats questions[14] were mapped on to an experiential learning cycle by John Driscoll[15] to form a simple a framework for supporting reflection. This framework is easy to remember and implement, and is therefore a popular option used by many health care professionals and advocated by professional bodies.
There are only 3 steps in this framework: [16]
What?
These questions prompt the reflector to describe what has happened by:
- What were the roles of the people involved?
- What was my role?
- What were the problems
- What happened
- What did I do?
So What?
This is the analysis of the reflection.:
- What was the outcome?
- What did you learn?
- What was important?
What Now?
This is one of the most important sections of a reflection. This section focuses on what will you do next / what does your learning experience mean for future practice?
- What do you need to do now?
- What were the consequences?
- How do you resolve the situation / improve the outcome?
- How will what have you learnt from this experience change your future practice? [17]
Conclusion
Now you have learnt about 3 of the main learning frameworks / reflective structures to use in clinical practice. It is important to understand that reflection is a skill that is developed through repeated practice. When selecting a model to use it is essential, as discussed previously, to try different structures and frameworks for different situations to learn which suit you and a particular context best. Day to day reflections (e.g. for CPD events) may be better suited to the Borton’s framework, whereas for an academic piece of work or a significant incident at work, a more detailed framework such as Gibbs may be more appropriate. It is also important to review relevant literature as well as your own experience and anecdotal evidence and include this within your reflections to develop an evidence based practice approach in your reflective practice.
Resources
References
- ↑ Schön DA. The reflective practitioner: How professionals think in action. Basic books; 1983.
- ↑ McClure P. Reflection on Practice. ↑ Reid B. But We’re Doing it Already! – Exploring afckLRResponse to the Concept of Reflective Practice in Order to Improve its Facilitation. Nurse Education Today 1993;13:305-309
- ↑ Jarvis P. Reflective Practice and Nursing. NursefckLREducation Today 1992;12:174-181
- ↑ Johns C. Becoming a reflective practitioner.fckLROxford: Blackwell Science, 2000
- ↑ 6.06.16.26.36.4 Paterson C, Chapman J. Enhancing skills of critical reflection to evidence learning in professional practice. Physical Therapy in Sport. 2013 Aug 1;14(3):133-8. Available from: ↑ Patterson B. Developing and Maintaining Reflection in Clinical Journals. Nursing Today 1995;15:211-220
- ↑ McClure P. Reflection on Practice. ↑ Queen Mary University of London. Guidance on Reflective Writing. ↑ McClure P. Reflection on Practice. ↑ Wessel J, Larin H. Blackwell Publishing Ltd Change in reflections of physiotherapy students over time in clinical placements. Learning in Health and Social Care 2006; 5(3):119–132
- ↑ Queen Mary University of London. Guidance on Reflective Writing. ↑ Queen Mary University of London. Guidance on Reflective Writing. ↑ Borton, T. (1970) Reach, Touch and Teach. London:Hutchinson.
- ↑ Driscoll J. Reflective practice for practise. Senior Nurse. 1994;14(1):47.
- ↑ White S,Fook J, Gardner F. Critical Reflection in Health and Social Care. Maidenhead: Open University Press, 2006
- ↑ Queen Mary University of London. Guidance on Reflective Writing. function gtElInit() { var lib = new google.translate.TranslateService(); lib.setCheckVisibility(false); lib.translatePage('en', 'pt', function (progress, done, error) { if (progress == 100 || done || error) { document.getElementById("gt-dt-spinner").style.display = "none"; } }); }
Ola!
Como podemos ajudar?